Back
Poster Session B
Fibrosing rheumatic diseases (scleroderma, MCTD, IgG4-related disease, scleroderma mimics)
Session: (1046–1070) Systemic Sclerosis and Related Disorders – Clinical Poster I
1055: Associations of Potential Risk Factors with Severe Outcomes in Scleroderma Renal Crisis: Results from a Single Center Study
Sunday, November 13, 2022
9:00 AM – 10:30 AM Eastern Time
Location: Virtual Poster Hall
- AL
Alex Luta, MD
MedStar Georgetown University Hospital
Rockville, MD, United States
Abstract Poster Presenter(s)
Alex Luta1, Saloni Godbole1 and Virginia Steen2, 1Medstar Georgetown University Hospital, Washington, DC, 2Georgetown University School of Medicine, Washington, DC
Background/Purpose: Scleroderma Renal Crisis (SRC) is a severe and life-threatening complication of Systemic Sclerosis (SSc). Given the rare nature of SSc, it is challenging to collect data to further our understanding of SRC. We sought to collect and analyze data on SRC patients to allow us to better understand this condition by discovering new insights regarding risk factors for severe outcomes.
Methods: Our institution is part of a 4-center study on SRC, but for this aspect of the study, we analyzed data from 44 patients at our institution who experienced SRC over a 12-year period (from 2008 to 2020). We performed chart reviews and collected over 100 data points per patient. We specifically evaluated the following outcomes with Chi-Squared and Fisher’s exact tests: dialysis at time of SRC, dialysis at 6 months after SRC, and 1-year survival post-SRC. We report odds ratios (ORs) and corresponding 95% confidence intervals (CIs).
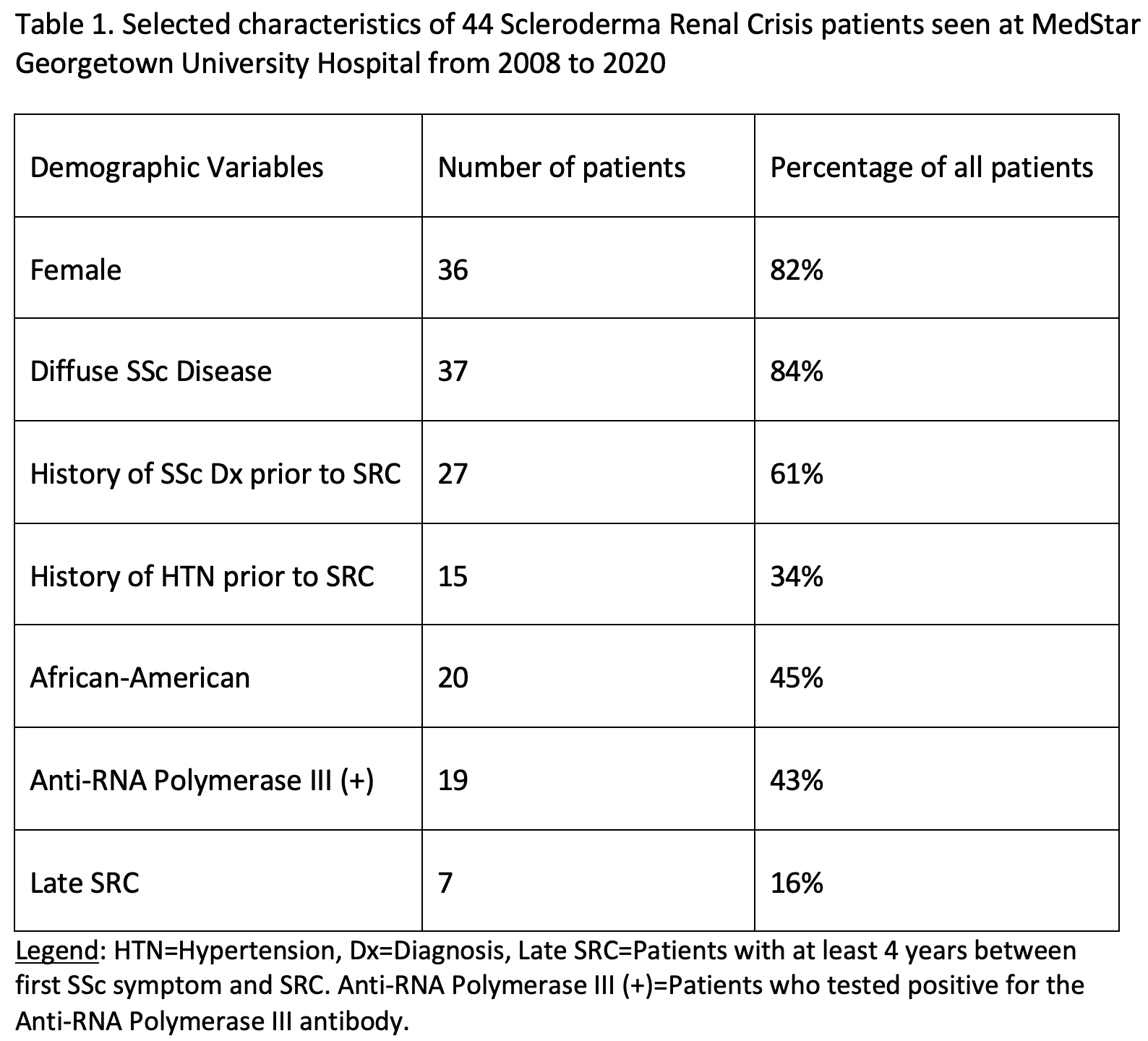
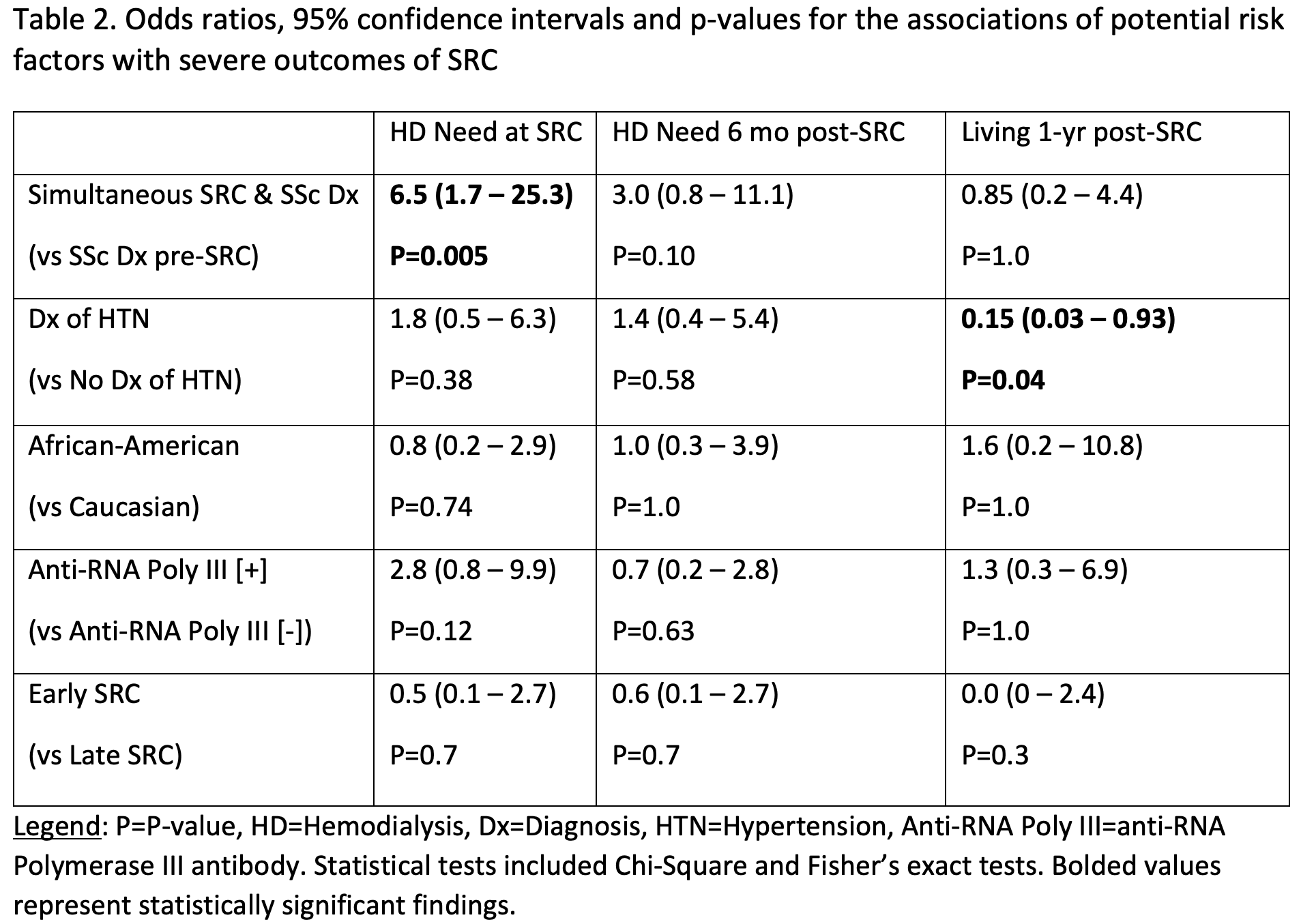
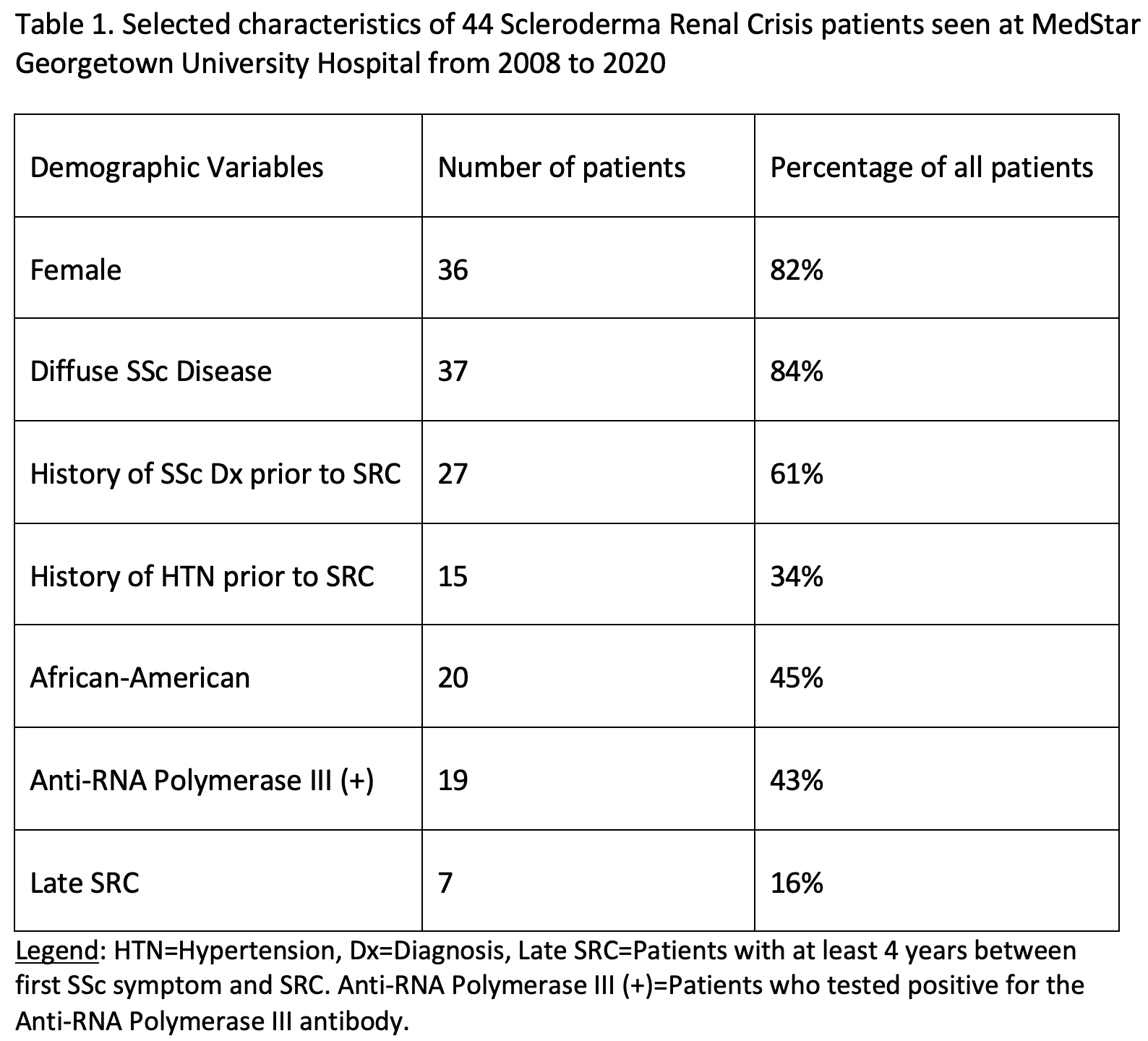
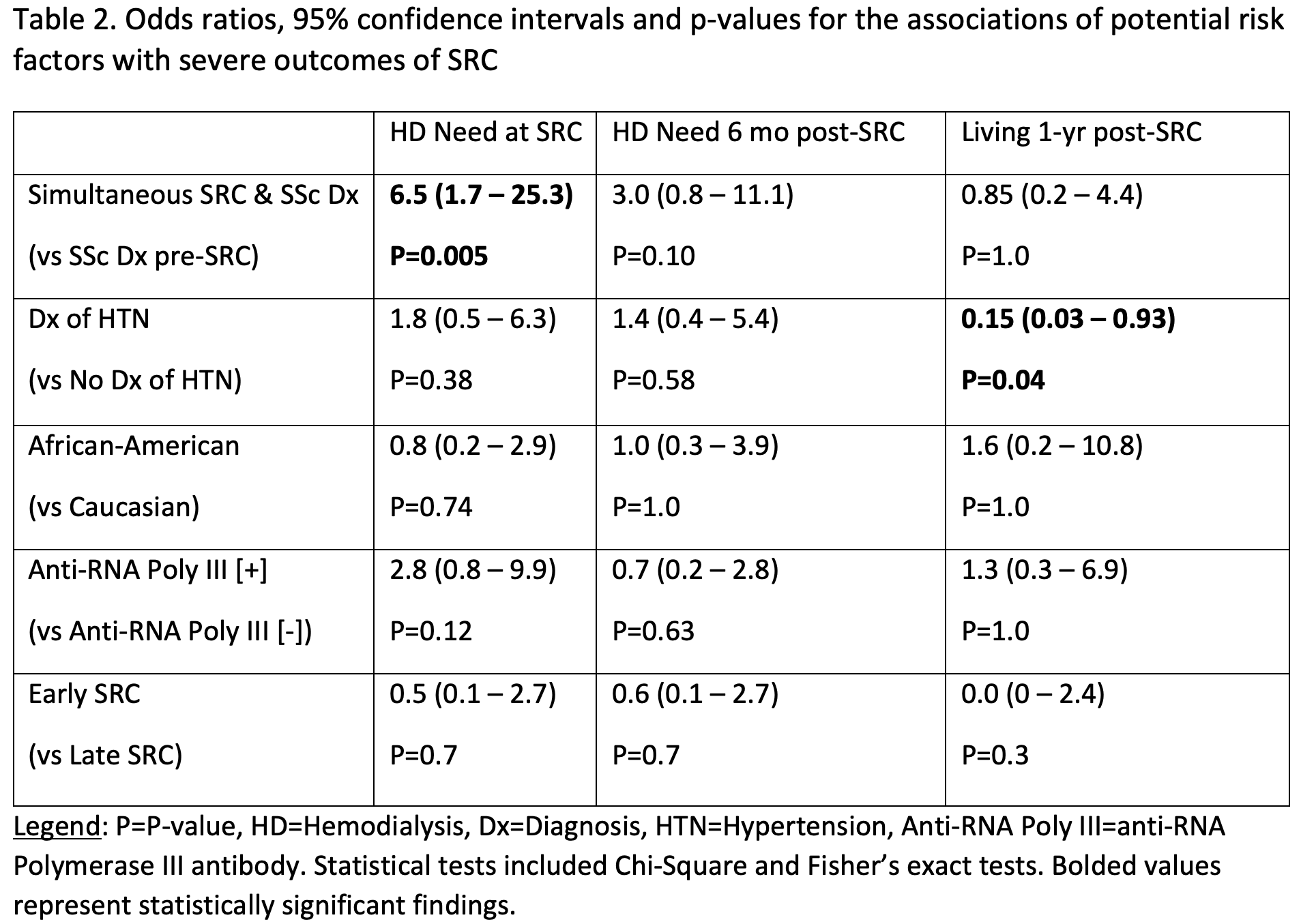
Results: We present selected demographic information of our SRC patients in Table 1.Patients who did not have a diagnosis of SSc before SRC had a statistically significant higher odds of requiring dialysis during SRC compared to patients who had a prior diagnosis of SSc (Table 2).SRC is associated with malignant hypertension, and we found that patients with a prior history of hypertension (HTN) had a statistically significant higher odds of 1-year mortality compared to patients without HTN (Table 2). While there are reports suggesting that African-American patients have worse SRC outcomes than Caucasians, we did not find any significant differences regarding odds of development of worse outcomes in our 20 African-American patients (Table 2). (It is important to note that the Caucasian patients had a higher risk profile compared to the African-American patients, as they were more likely to be older and male. Because older age and male sex are independent risk factors for severe outcomes, this may in part explain our findings). Although it has been suggested that patients with anti-RNA Polymerase III antibodies may have a more rapidly progressive and aggressive SSc disease course, our study did not find any difference in odds of severe outcomes for patients with or without this antibody (Table 2). Lastly, we investigated differences in outcomes regarding patients with early and late SRC. We did not find any significant differences regarding odds of severe outcomes (Table 2), possibly due to sparse data (there were only 7 patients with late SRC).
Conclusion: Our finding that patients that did not have a diagnosis of SSc before SRC had a statistically significant higher odds of requiring dialysis during SRC is both new and clinically significant. We plan to further investigate the characteristics of the patient population that had simultaneous diagnoses of SSc and SRC to better understand this finding. Hypotheses to test include that they had a more rapid, severe form of SSc or had a delay in recognition of and treatment for SRC. Given the small sample sizes, we will re-test our hypotheses (and test new hypotheses) on a larger dataset. This will further advance our understanding of SRC risk factors, allow Rheumatologists to more effectively risk-stratify SSc patients, and may help prevent severe outcomes.
Disclosures: A. Luta, SurgiBox, Inc.; S. Godbole, None; V. Steen, None.
Background/Purpose: Scleroderma Renal Crisis (SRC) is a severe and life-threatening complication of Systemic Sclerosis (SSc). Given the rare nature of SSc, it is challenging to collect data to further our understanding of SRC. We sought to collect and analyze data on SRC patients to allow us to better understand this condition by discovering new insights regarding risk factors for severe outcomes.
Methods: Our institution is part of a 4-center study on SRC, but for this aspect of the study, we analyzed data from 44 patients at our institution who experienced SRC over a 12-year period (from 2008 to 2020). We performed chart reviews and collected over 100 data points per patient. We specifically evaluated the following outcomes with Chi-Squared and Fisher’s exact tests: dialysis at time of SRC, dialysis at 6 months after SRC, and 1-year survival post-SRC. We report odds ratios (ORs) and corresponding 95% confidence intervals (CIs).
Results: We present selected demographic information of our SRC patients in Table 1.Patients who did not have a diagnosis of SSc before SRC had a statistically significant higher odds of requiring dialysis during SRC compared to patients who had a prior diagnosis of SSc (Table 2).SRC is associated with malignant hypertension, and we found that patients with a prior history of hypertension (HTN) had a statistically significant higher odds of 1-year mortality compared to patients without HTN (Table 2). While there are reports suggesting that African-American patients have worse SRC outcomes than Caucasians, we did not find any significant differences regarding odds of development of worse outcomes in our 20 African-American patients (Table 2). (It is important to note that the Caucasian patients had a higher risk profile compared to the African-American patients, as they were more likely to be older and male. Because older age and male sex are independent risk factors for severe outcomes, this may in part explain our findings). Although it has been suggested that patients with anti-RNA Polymerase III antibodies may have a more rapidly progressive and aggressive SSc disease course, our study did not find any difference in odds of severe outcomes for patients with or without this antibody (Table 2). Lastly, we investigated differences in outcomes regarding patients with early and late SRC. We did not find any significant differences regarding odds of severe outcomes (Table 2), possibly due to sparse data (there were only 7 patients with late SRC).
Conclusion: Our finding that patients that did not have a diagnosis of SSc before SRC had a statistically significant higher odds of requiring dialysis during SRC is both new and clinically significant. We plan to further investigate the characteristics of the patient population that had simultaneous diagnoses of SSc and SRC to better understand this finding. Hypotheses to test include that they had a more rapid, severe form of SSc or had a delay in recognition of and treatment for SRC. Given the small sample sizes, we will re-test our hypotheses (and test new hypotheses) on a larger dataset. This will further advance our understanding of SRC risk factors, allow Rheumatologists to more effectively risk-stratify SSc patients, and may help prevent severe outcomes.
Disclosures: A. Luta, SurgiBox, Inc.; S. Godbole, None; V. Steen, None.

