Back
Poster Session D
Sjögren's syndrome
Session: (2017–2051) Sjögren's Syndrome – Basic and Clinical Science Poster
2026: Serum and Tear Autoantibodies from nor Mice as Potential Diagnostic Indicators of Local and Systemic Inflammation in Sjögren’s Syndrome
Monday, November 14, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- SS
Shruti Singh Kakan, MS, BS
University of Southern California, Keck School of Medicine
Los Angeles, CA, United States
Abstract Poster Presenter(s)
Shruti Singh Kakan1, Yaping Ju2, Maria Edman2 and Sarah Hamm-Alvarez3, 1Department of Pharmacology and Pharmaceutical Sciences, School of Pharmacy, University of Southern California; Department of Ophthalmology, Keck School of Medicine, Roski Eye Institute, University of Southern California, Los Angeles, CA, 2Department of Ophthalmology, Keck School of Medicine, Roski Eye Institute, University of Southern California, Los Angeles, CA, 3Department of Ophthalmology, Keck School of Medicine, Roski Eye Institute, University of Southern California; Department of Pharmacology and Pharmaceutical Sciences, School of Pharmacy, University of Southern California, Los Angeles, CA
Background/Purpose: Sjögren's Syndrome (SS) is an autoimmune disease characterized by infiltration of lymphocytes into lacrimal (LG) and salivary (SG) glands and their concurrent loss of tear and saliva production, respectively, as well as the development of systemic symptoms. Diagnosis of SS takes ~3 years, due in part to manifestation of symptoms that overlap with other autoimmune diseases. Ro/SSA (and previously, ANA and La/SSB) serum autoantibodies, currently utilized for diagnosis, are only present in 50-60% of SS patients and are also detected in patients with systemic lupus erythematosus and rheumatoid arthritis. As the LG is specifically affected in SS, leading to established changes in tear composition, we hypothesized that the presence of tear autoantibodies may also aid in distinguishing SS from other autoimmune diseases. Here, we have used two SS mouse models, the male NOD (non-obese diabetic) which spontaneously develops SS-like dacryoadenitis, and the male NOR/Ltj (non-obese diabetes resistant, alternative to NOD) to investigate the changes in autoantibody composition of tear fluid and serum for an array of autoantigens, relative to age-matched healthy control BALB/c mice.
Methods: Serum samples were collected from 16-week-old male NOR (n=6), and age and sex-matched healthy BALB/c mice (n=3). Pooled tears were collected from the same mice following in situ topical carbachol stimulation of LG. Additional serum samples were collected from 8-week and 24-week male NOD mice (n=3) and age-matched healthy male BALB/c mice (n=3). Tears and serum were screened for IgG/IgM reactivity against a panel of 128 autoantigens at the UT Southwestern Microarray Core Facility, Dallas, TX. Instrument normalized data was analyzed in RStudio with data points with signal to noise ratio (SNR) < 3 excluded from the analysis3.
Results: Total IgG antibodies were 2.3 and 1.96-fold elevated in serum and tears, respectively, of NOR mice (padj< 0.05 both). IgG autoantibodies against Pm/Scl-100 (10.8-fold, p= 2.6 x10-5), La/SSB (9.7-fold, p= 2.5 x10-5), PL-7 (6.8-fold, p= 0.01) and PCNA (4.4-fold, p= 0.04) were significantly elevated in serum of NOR mice relative to healthy BALB/c. Interestingly, IgG autoantibodies against the same autoantigens were also significantly increased in serum of male NOD. On the other hand, IgG autoantibodies against Jo-1 (25.2-fold, p = 2.4x10-3), β-2 glycoprotein (28.5-fold, p=8.6x10-3), complements C6 & C7, and EBNA1 were significantly increased ( >3-fold, p< 0.01, all) in tears of NOR mice but remained unchanged in serum of the same mice relative to BALB/c. While no changes were detected in IgM immunoreactivity for any of the antigens in serum of NOR mice, IgM autoantibodies against Thyroid Peroxidase (TPO) (13.8-fold, p= 4.2x10-4) and Histone H4 (3.5-fold, p =1.7x10-6) were significantly elevated in tears of NOR mice.
Conclusion: Tears of male NOR mouse, a model of SS, have autoantibody profiles distinct from serum and may reflect local inflammation in the LG occurring independent of and/or prior to systemic inflammation. Additionally, four serum autoantibodies found elevated in NOR mice were validated in the male NOD mice. Further investigation of these autoantibodies is necessary in tears of SS patients.
.jpg) Figure 1. Serum IgG autoantibodies in male NOR (above) and NOD (below) mice. The NOD mice develop autoimmune dacryoadenitis at about 6-8 weeks, whereas the NOR, which is a NOD-related MHC-syngeneic strain, have a later onset of dacryoadenitis at about 14-16 weeks. Though the NOD is the most established mouse model for SS, the eventual development of diabetes beyond 20 weeks is a confounder for studying SS, which the diabetes resistant NOR model obviates. La/SSB, Sjögren’s Syndrome Antigen B; PM/Scl-100, Polymyositis/Systemic Sclerosis Antigen 100; PL-7, anti-threonyl-tRNA synthetase-7; PCNA - Proliferating Cell Nuclear Antigen; (ns – not significant, * p < 0.01, ** p < 0.005, *** p < 10-3, **** p < 10-4, moderated t-tests and a priori contrasts computed using the R Package limma, alpha value=0.01 as described previously by Kiripolsky J, et al Clinical Immunology. 2017 Oct).
Figure 1. Serum IgG autoantibodies in male NOR (above) and NOD (below) mice. The NOD mice develop autoimmune dacryoadenitis at about 6-8 weeks, whereas the NOR, which is a NOD-related MHC-syngeneic strain, have a later onset of dacryoadenitis at about 14-16 weeks. Though the NOD is the most established mouse model for SS, the eventual development of diabetes beyond 20 weeks is a confounder for studying SS, which the diabetes resistant NOR model obviates. La/SSB, Sjögren’s Syndrome Antigen B; PM/Scl-100, Polymyositis/Systemic Sclerosis Antigen 100; PL-7, anti-threonyl-tRNA synthetase-7; PCNA - Proliferating Cell Nuclear Antigen; (ns – not significant, * p < 0.01, ** p < 0.005, *** p < 10-3, **** p < 10-4, moderated t-tests and a priori contrasts computed using the R Package limma, alpha value=0.01 as described previously by Kiripolsky J, et al Clinical Immunology. 2017 Oct).
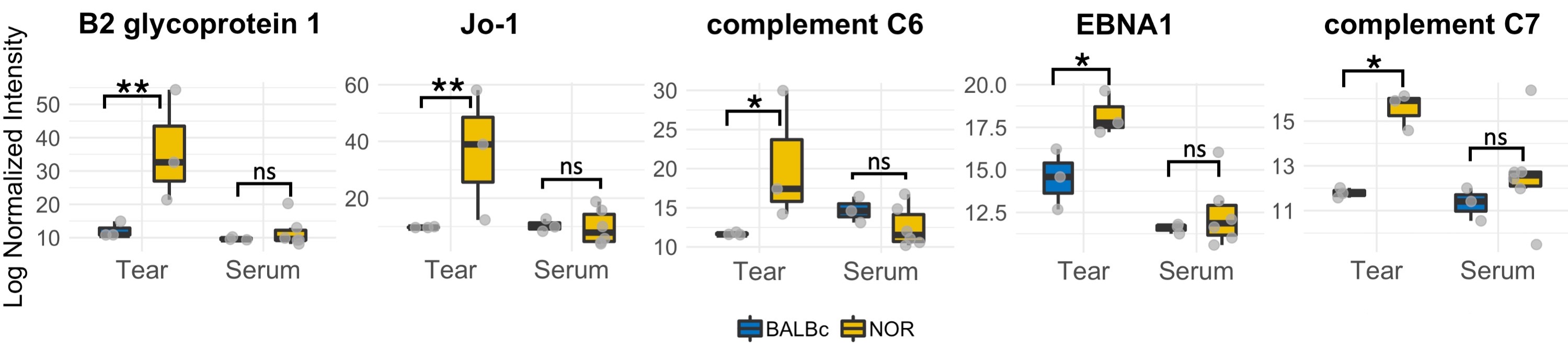 Figure 2. Tear specific IgG autoantibodies in male NOR mice. EBNA, Epstein-Barr Virus Nuclear Antigen 1; Jo-1, anti-histidine-tRNA ligase -1. (ns – not significant, * p < 0.01, ** p < 0.001, moderated t-tests and a priori contrasts computed using linear model for series of array (limma) R package, alpha value=0.01)
Figure 2. Tear specific IgG autoantibodies in male NOR mice. EBNA, Epstein-Barr Virus Nuclear Antigen 1; Jo-1, anti-histidine-tRNA ligase -1. (ns – not significant, * p < 0.01, ** p < 0.001, moderated t-tests and a priori contrasts computed using linear model for series of array (limma) R package, alpha value=0.01)
Disclosures: S. Singh Kakan, None; Y. Ju, None; M. Edman, Oyster Point Pharma; S. Hamm-Alvarez, Oyster Point Pharma.
Background/Purpose: Sjögren's Syndrome (SS) is an autoimmune disease characterized by infiltration of lymphocytes into lacrimal (LG) and salivary (SG) glands and their concurrent loss of tear and saliva production, respectively, as well as the development of systemic symptoms. Diagnosis of SS takes ~3 years, due in part to manifestation of symptoms that overlap with other autoimmune diseases. Ro/SSA (and previously, ANA and La/SSB) serum autoantibodies, currently utilized for diagnosis, are only present in 50-60% of SS patients and are also detected in patients with systemic lupus erythematosus and rheumatoid arthritis. As the LG is specifically affected in SS, leading to established changes in tear composition, we hypothesized that the presence of tear autoantibodies may also aid in distinguishing SS from other autoimmune diseases. Here, we have used two SS mouse models, the male NOD (non-obese diabetic) which spontaneously develops SS-like dacryoadenitis, and the male NOR/Ltj (non-obese diabetes resistant, alternative to NOD) to investigate the changes in autoantibody composition of tear fluid and serum for an array of autoantigens, relative to age-matched healthy control BALB/c mice.
Methods: Serum samples were collected from 16-week-old male NOR (n=6), and age and sex-matched healthy BALB/c mice (n=3). Pooled tears were collected from the same mice following in situ topical carbachol stimulation of LG. Additional serum samples were collected from 8-week and 24-week male NOD mice (n=3) and age-matched healthy male BALB/c mice (n=3). Tears and serum were screened for IgG/IgM reactivity against a panel of 128 autoantigens at the UT Southwestern Microarray Core Facility, Dallas, TX. Instrument normalized data was analyzed in RStudio with data points with signal to noise ratio (SNR) < 3 excluded from the analysis3.
Results: Total IgG antibodies were 2.3 and 1.96-fold elevated in serum and tears, respectively, of NOR mice (padj< 0.05 both). IgG autoantibodies against Pm/Scl-100 (10.8-fold, p= 2.6 x10-5), La/SSB (9.7-fold, p= 2.5 x10-5), PL-7 (6.8-fold, p= 0.01) and PCNA (4.4-fold, p= 0.04) were significantly elevated in serum of NOR mice relative to healthy BALB/c. Interestingly, IgG autoantibodies against the same autoantigens were also significantly increased in serum of male NOD. On the other hand, IgG autoantibodies against Jo-1 (25.2-fold, p = 2.4x10-3), β-2 glycoprotein (28.5-fold, p=8.6x10-3), complements C6 & C7, and EBNA1 were significantly increased ( >3-fold, p< 0.01, all) in tears of NOR mice but remained unchanged in serum of the same mice relative to BALB/c. While no changes were detected in IgM immunoreactivity for any of the antigens in serum of NOR mice, IgM autoantibodies against Thyroid Peroxidase (TPO) (13.8-fold, p= 4.2x10-4) and Histone H4 (3.5-fold, p =1.7x10-6) were significantly elevated in tears of NOR mice.
Conclusion: Tears of male NOR mouse, a model of SS, have autoantibody profiles distinct from serum and may reflect local inflammation in the LG occurring independent of and/or prior to systemic inflammation. Additionally, four serum autoantibodies found elevated in NOR mice were validated in the male NOD mice. Further investigation of these autoantibodies is necessary in tears of SS patients.
.jpg) Figure 1. Serum IgG autoantibodies in male NOR (above) and NOD (below) mice. The NOD mice develop autoimmune dacryoadenitis at about 6-8 weeks, whereas the NOR, which is a NOD-related MHC-syngeneic strain, have a later onset of dacryoadenitis at about 14-16 weeks. Though the NOD is the most established mouse model for SS, the eventual development of diabetes beyond 20 weeks is a confounder for studying SS, which the diabetes resistant NOR model obviates. La/SSB, Sjögren’s Syndrome Antigen B; PM/Scl-100, Polymyositis/Systemic Sclerosis Antigen 100; PL-7, anti-threonyl-tRNA synthetase-7; PCNA - Proliferating Cell Nuclear Antigen; (ns – not significant, * p < 0.01, ** p < 0.005, *** p < 10-3, **** p < 10-4, moderated t-tests and a priori contrasts computed using the R Package limma, alpha value=0.01 as described previously by Kiripolsky J, et al Clinical Immunology. 2017 Oct).
Figure 1. Serum IgG autoantibodies in male NOR (above) and NOD (below) mice. The NOD mice develop autoimmune dacryoadenitis at about 6-8 weeks, whereas the NOR, which is a NOD-related MHC-syngeneic strain, have a later onset of dacryoadenitis at about 14-16 weeks. Though the NOD is the most established mouse model for SS, the eventual development of diabetes beyond 20 weeks is a confounder for studying SS, which the diabetes resistant NOR model obviates. La/SSB, Sjögren’s Syndrome Antigen B; PM/Scl-100, Polymyositis/Systemic Sclerosis Antigen 100; PL-7, anti-threonyl-tRNA synthetase-7; PCNA - Proliferating Cell Nuclear Antigen; (ns – not significant, * p < 0.01, ** p < 0.005, *** p < 10-3, **** p < 10-4, moderated t-tests and a priori contrasts computed using the R Package limma, alpha value=0.01 as described previously by Kiripolsky J, et al Clinical Immunology. 2017 Oct).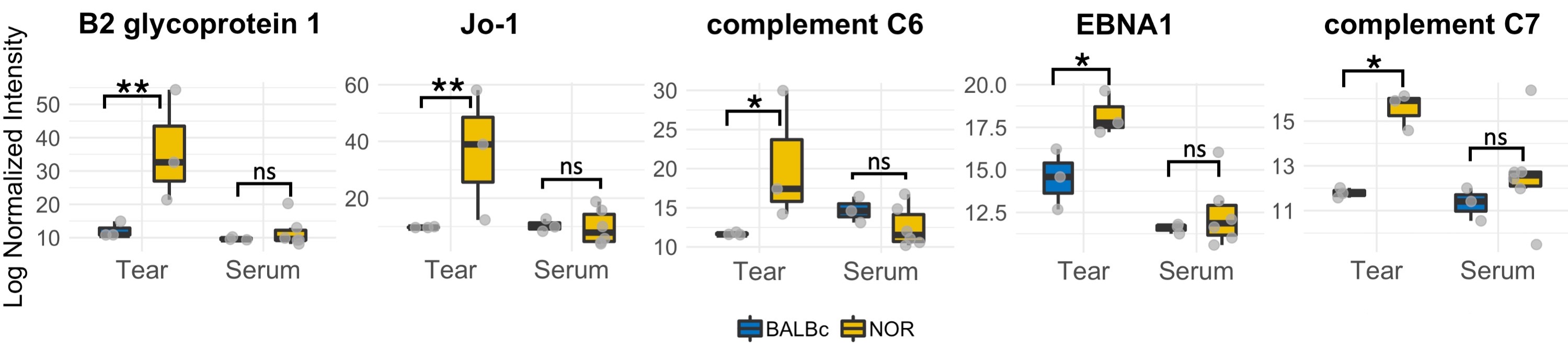 Figure 2. Tear specific IgG autoantibodies in male NOR mice. EBNA, Epstein-Barr Virus Nuclear Antigen 1; Jo-1, anti-histidine-tRNA ligase -1. (ns – not significant, * p < 0.01, ** p < 0.001, moderated t-tests and a priori contrasts computed using linear model for series of array (limma) R package, alpha value=0.01)
Figure 2. Tear specific IgG autoantibodies in male NOR mice. EBNA, Epstein-Barr Virus Nuclear Antigen 1; Jo-1, anti-histidine-tRNA ligase -1. (ns – not significant, * p < 0.01, ** p < 0.001, moderated t-tests and a priori contrasts computed using linear model for series of array (limma) R package, alpha value=0.01)Disclosures: S. Singh Kakan, None; Y. Ju, None; M. Edman, Oyster Point Pharma; S. Hamm-Alvarez, Oyster Point Pharma.

