Back
Poster Session D
Epidemiology, health policy and outcomes
Session: (1750–1786) Epidemiology and Public Health Poster III
1782: Sociocultural and Moral Factors Influencing the Decision to Vaccinate Among Rheumatic Patients: A Qualitative Study
Monday, November 14, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- AM
Amaranta Manrique de Lara, BSc, MA
Hospital General de México Dr. Eduardo Liceaga
Mexico City, Federal District, Mexico
Abstract Poster Presenter(s)
Tirsa Colmenares-Roa1, Amaranta ManriquedeLara2, Virginia Pascual Ramos3, JOSE FRANCISCO MOCTEZUMA RIOS4, Irazu Contreras-Ibañez5, Everardo Alvarez-Hernandez6, Guillermo Guaracha Basañez7, Graciela Meza-LópezyOlguin4 and Ingris Pelaez-Ballestas1, 1Hospital General de México "Dr. Eduardo Liceaga", Ciudad de México, Mexico, 2Hospital General de México "Dr. Eduardo Liceaga,", Ciudad de México, Mexico, 3Instituto Nacional de Ciencias Medicas y Nutricion Salvador Zubiran, Ciudad de México, Mexico, 4HOSPITAL GENERAL DE MEXICO "Dr. Eduardo Liceaga", Ciudad de México, Mexico, 5Instituto Nacional de Nutricion Salvador Zubirán, Ciudad de México, Mexico, 6Hospital General de Mexico "Dr.Eduardo Liceaga", Ciudad de México, Mexico, 7Instituto Nacional de Ciencias Médicas y Nutrición \"Salvador Zubirn\", Ciudad de México, Mexico
Background/Purpose: Vaccination is a process that involves individual, social and moral aspects, beyond public governance of vaccines or vaccination as a public health concern. The ways people incorporate their beliefs and concerns into vaccine decision-making affect the effectiveness of these interventions for individual and community health. The aim of this study is to describe the sociocultural and moral factors that influence the decision to vaccinate in general and to vaccinate against COVID-19 specifically, among patients at the rheumatology units of two public hospitals in Mexico City.
Methods: This was a qualitative study involving individual semi-structured interviews following an interview guide. We conducted a thematic analysis using the ATLAS.ti software, with further triangulation to verify concordance and aid in the interpretation of the data from a medical anthropology framework and using a narrative ethics approach to gain insight into the participants' underlying moral values.
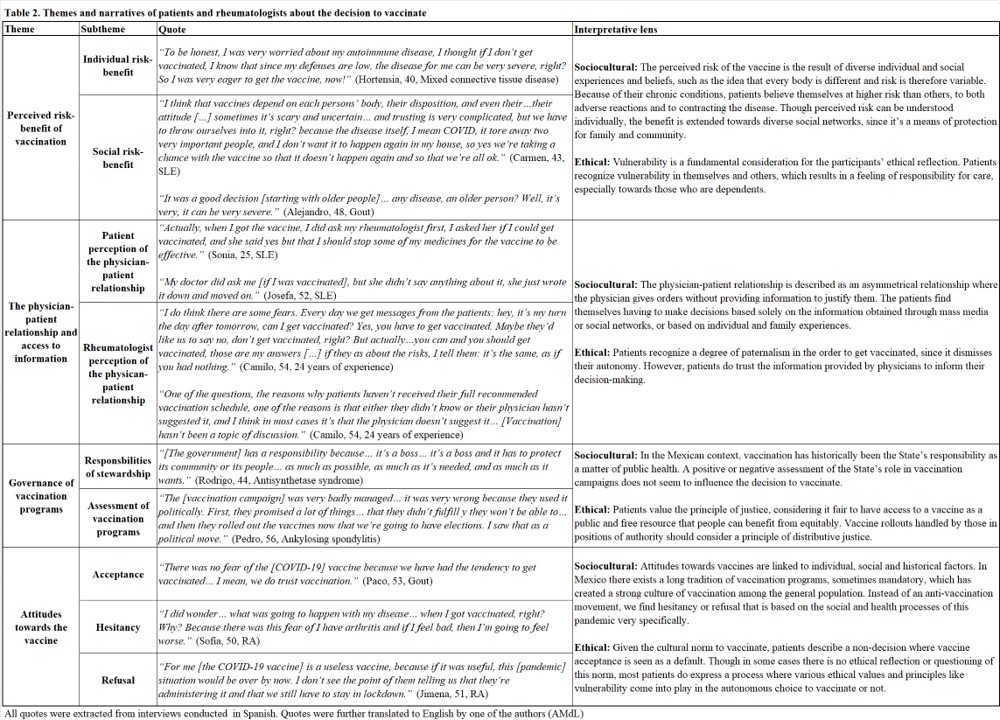
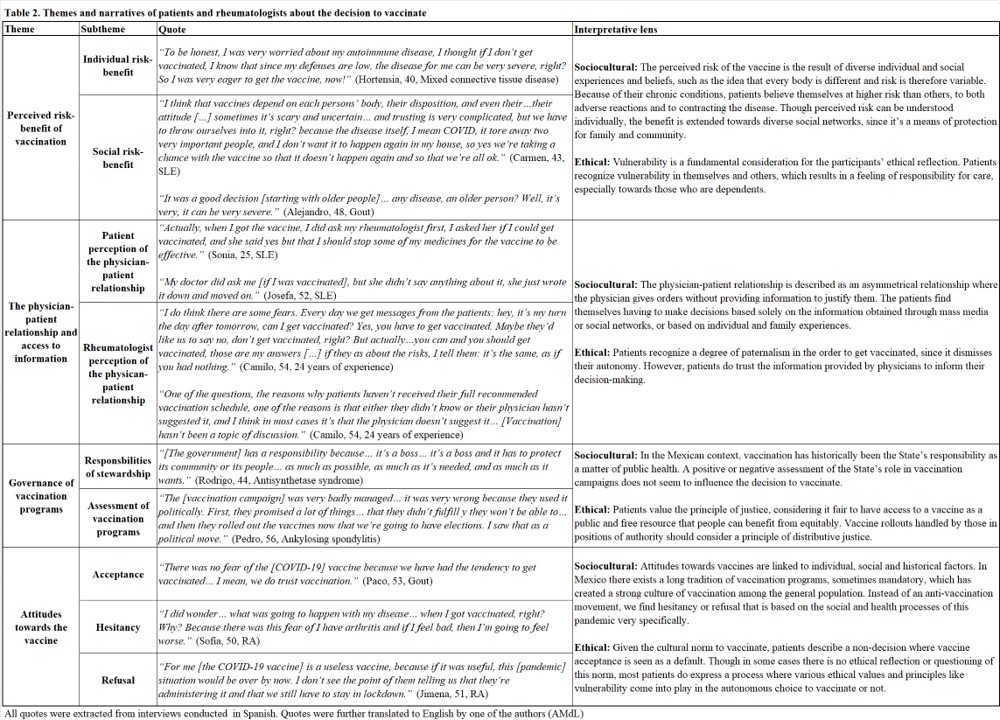
Results: We interviewed 37 patients in total, along with 3 rheumatologists (Table 1). Four core themes emerged from the analysis to understand the decision to vaccinate: 1. Perceived risk-benefit of vaccination. 2. The physician-patient relationship and access to information. 3. Governance of vaccination programs. 4. Attitudes towards the vaccine. (Table 2). Individual and family experiences with vaccination are diverse depending on the type of vaccine involved: the childhood immunization schedule is accepted without a doubt; there is a feeling of complacency so that vaccines recommended for adults, such as influenza and tetanus, are thought to not be needed; and the COVID-19 vaccine, as a new medical technology, is met with more controversy leading to hesitancy.
Conclusion: The decision to vaccinate among Mexican rheumatic patients can sometimes involve doubt and distrust, but ultimately there is acceptance in the majority of cases. Though patients make and value autonomous decisions, there exists a collective process involving sociocultural and moral aspects such as: the presence of a strong local vaccination culture that can be at conflict with experiences of (dis)trust towards vaccines; the preeminence of relational networks; vague biomedical knowledge, which is not a decisive factor for acceptance; infrequent discussion about vaccines during the medical consultation, exacerbated by the pandemic context; and the high regard of values such as vulnerability and justice. Taking into consideration the sociocultural and moral perspectives of vaccination is fundamental to understand patients' specific concerns and beliefs and thus develop effective public health interventions. These should encourage rheumatologists to prioritize having conversations about vaccination generally beyond the immediate threat of COVID-19, given the high levels of trust. Rheumatologists should understand themselves not as authorities in a vertical relationship, but as another factor that strengthen patients' moral agency and capacity to make informed, autonomous decisions.
.jpg)
Disclosures: T. Colmenares-Roa, None; A. ManriquedeLara, None; V. Pascual Ramos, None; J. MOCTEZUMA RIOS, None; I. Contreras-Ibañez, None; E. Alvarez-Hernandez, None; G. Guaracha Basañez, None; G. Meza-LópezyOlguin, None; I. Pelaez-Ballestas, None.
Background/Purpose: Vaccination is a process that involves individual, social and moral aspects, beyond public governance of vaccines or vaccination as a public health concern. The ways people incorporate their beliefs and concerns into vaccine decision-making affect the effectiveness of these interventions for individual and community health. The aim of this study is to describe the sociocultural and moral factors that influence the decision to vaccinate in general and to vaccinate against COVID-19 specifically, among patients at the rheumatology units of two public hospitals in Mexico City.
Methods: This was a qualitative study involving individual semi-structured interviews following an interview guide. We conducted a thematic analysis using the ATLAS.ti software, with further triangulation to verify concordance and aid in the interpretation of the data from a medical anthropology framework and using a narrative ethics approach to gain insight into the participants' underlying moral values.
Results: We interviewed 37 patients in total, along with 3 rheumatologists (Table 1). Four core themes emerged from the analysis to understand the decision to vaccinate: 1. Perceived risk-benefit of vaccination. 2. The physician-patient relationship and access to information. 3. Governance of vaccination programs. 4. Attitudes towards the vaccine. (Table 2). Individual and family experiences with vaccination are diverse depending on the type of vaccine involved: the childhood immunization schedule is accepted without a doubt; there is a feeling of complacency so that vaccines recommended for adults, such as influenza and tetanus, are thought to not be needed; and the COVID-19 vaccine, as a new medical technology, is met with more controversy leading to hesitancy.
Conclusion: The decision to vaccinate among Mexican rheumatic patients can sometimes involve doubt and distrust, but ultimately there is acceptance in the majority of cases. Though patients make and value autonomous decisions, there exists a collective process involving sociocultural and moral aspects such as: the presence of a strong local vaccination culture that can be at conflict with experiences of (dis)trust towards vaccines; the preeminence of relational networks; vague biomedical knowledge, which is not a decisive factor for acceptance; infrequent discussion about vaccines during the medical consultation, exacerbated by the pandemic context; and the high regard of values such as vulnerability and justice. Taking into consideration the sociocultural and moral perspectives of vaccination is fundamental to understand patients' specific concerns and beliefs and thus develop effective public health interventions. These should encourage rheumatologists to prioritize having conversations about vaccination generally beyond the immediate threat of COVID-19, given the high levels of trust. Rheumatologists should understand themselves not as authorities in a vertical relationship, but as another factor that strengthen patients' moral agency and capacity to make informed, autonomous decisions.
.jpg)
Disclosures: T. Colmenares-Roa, None; A. ManriquedeLara, None; V. Pascual Ramos, None; J. MOCTEZUMA RIOS, None; I. Contreras-Ibañez, None; E. Alvarez-Hernandez, None; G. Guaracha Basañez, None; G. Meza-LópezyOlguin, None; I. Pelaez-Ballestas, None.

