Back
Poster Session B
Juvenile idiopathic arthritis (JIA) and pediatric joint disorders
Session: (0850–0880) Pediatric Rheumatology – Clinical Poster I: JIA
0873: Celiac-Associated Arthritis: Clinical Features, Treatment, and Outcomes
Sunday, November 13, 2022
9:00 AM – 10:30 AM Eastern Time
Location: Virtual Poster Hall
- AA
Ana Luiza Altaffer, MD
Texas Children's Hospital
Houston, TX, United States
Abstract Poster Presenter(s)
Ana Luiza Altaffer1 and Pamela Weiss2, 1Children's Hospital of Philadelphia, Philadelphia, PA, 2Children's Hospital of Philadelphia, Glen Mills, PA
Background/Purpose: Although arthritis is recognized as one of the extra-intestinal manifestations of celiac disease, little is known about the clinical course and outcomes of celiac-associated arthritis in the pediatric population. This study aims to describe clinical characteristics, treatment regimens, and outcomes of children with celiac disease and arthritis.
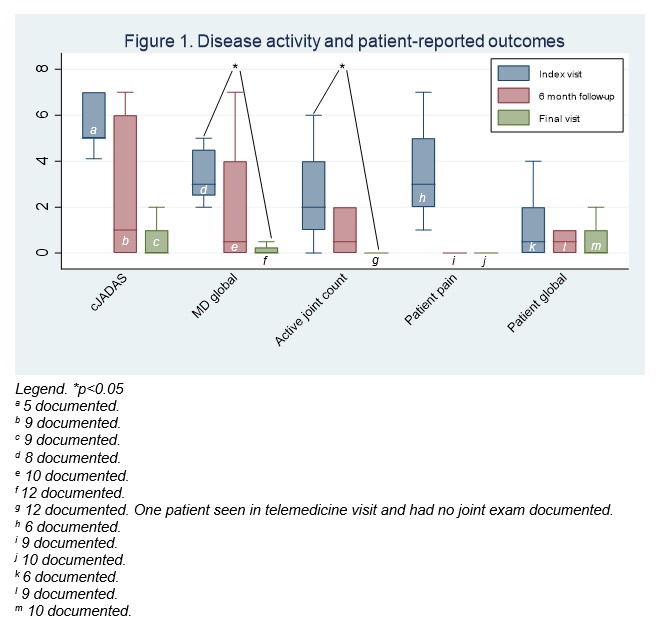
Methods: This was a retrospective cohort study of children with celiac disease seen in pediatric rheumatology clinic between 2004 and 2021 for joint complaints. Data was abstracted from electronic health records. Patient demographics and clinical manifestations were evaluated using standard descriptive statistics. Physician- and patient-reported outcomes were evaluated at the index visit (first recorded visit), at the 6 month follow-up, and at the last recorded visit, and were compared using Wilcoxon signed-rank tests.
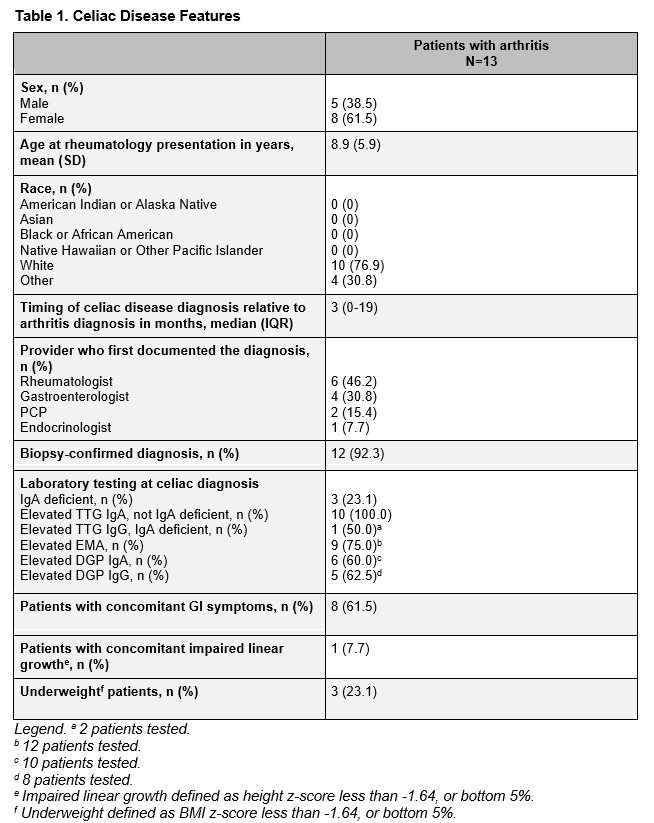
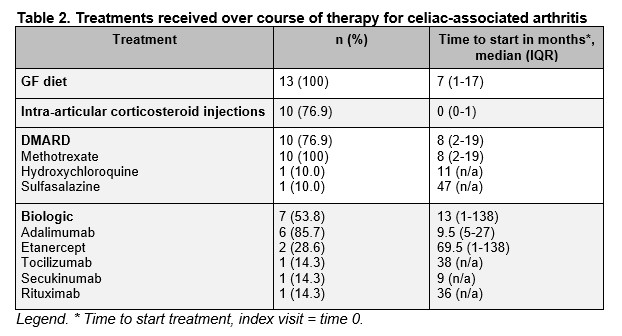
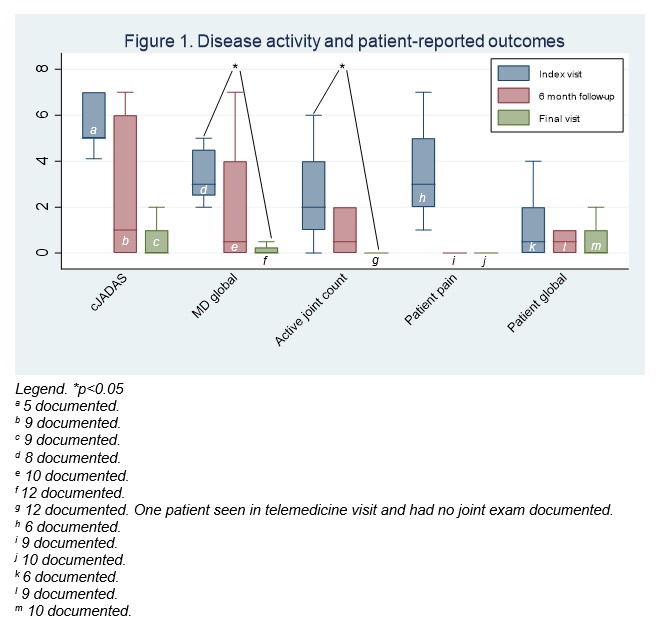
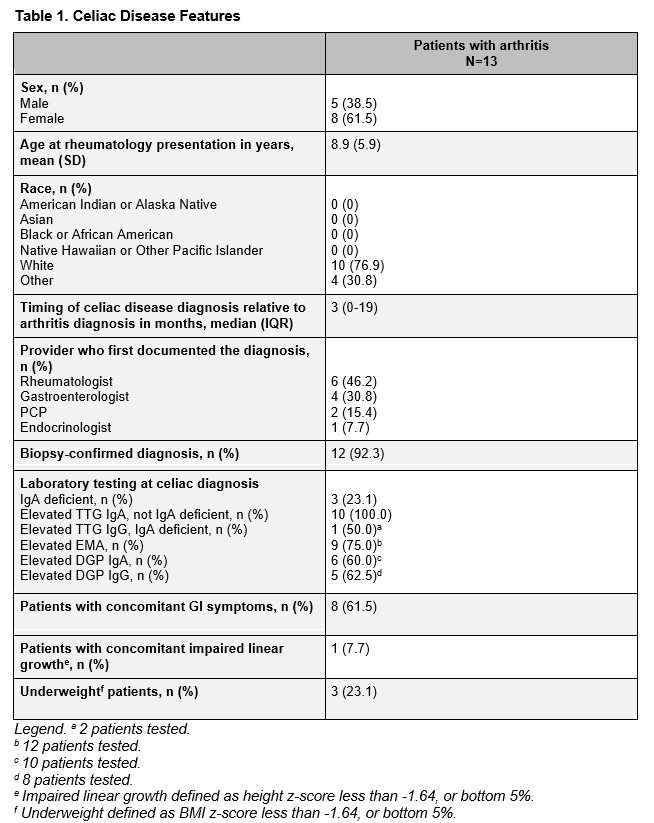
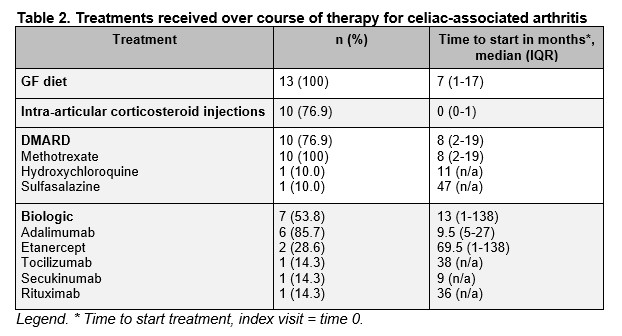
Results: Twenty-nine patients with celiac disease were evaluated for joint complaints, and 13 were diagnosed with arthritis. Their mean age was 8.9 years (SD 5.9), and 61.5% were female. Celiac disease diagnosis was made before arthritis diagnosis in only 2 cases (15.4%). Median timing of celiac disease diagnosis was 3 months following arthritis diagnosis (IQR 0-19 months). Initial testing that led to the diagnosis of celiac disease was obtained by the rheumatologist in 6 cases (46.2%). Only 8 patients (61.5%) had concomitant GI symptoms, and of these, 3 patients had BMI z-scores < -1.64 and 1 had impaired linear growth. Arthritis presentation was most often oligoarticular (76.9%) and asymmetric (84.6%). The most frequently involved joint was the knee (69.2%). Most cases required systemic therapy (n=11, 84.6%) with DMARDs, biologics, or a combination of both. Of the 10 patients who required systemic therapy and reported compliance with the gluten-free diet, 3 (30%) were able to stop systemic medications. Two of 3 patients who cleared celiac serologies came off systemic medications. Statistically significant improvement was noted in the number of joints involved (p=0.02) and physician global assessment of disease activity (p=0.03) between the index and final rheumatology visit.
Conclusion: Rheumatologists play an important role in the identification of celiac disease, as arthritis was the presenting symptom in most cases and was not always associated with GI symptoms or poor weight gain. The arthritis is most often oligoarticular and asymmetric. Most children required systemic therapy. The gluten-free diet may not be sufficient to manage arthritis, but antibody clearance may be an indicator of higher likelihood of disease control off medications. Nevertheless, outcomes are promising with a combination of diet and medical therapy.
Disclosures: A. Altaffer, None; P. Weiss, None.
Background/Purpose: Although arthritis is recognized as one of the extra-intestinal manifestations of celiac disease, little is known about the clinical course and outcomes of celiac-associated arthritis in the pediatric population. This study aims to describe clinical characteristics, treatment regimens, and outcomes of children with celiac disease and arthritis.
Methods: This was a retrospective cohort study of children with celiac disease seen in pediatric rheumatology clinic between 2004 and 2021 for joint complaints. Data was abstracted from electronic health records. Patient demographics and clinical manifestations were evaluated using standard descriptive statistics. Physician- and patient-reported outcomes were evaluated at the index visit (first recorded visit), at the 6 month follow-up, and at the last recorded visit, and were compared using Wilcoxon signed-rank tests.
Results: Twenty-nine patients with celiac disease were evaluated for joint complaints, and 13 were diagnosed with arthritis. Their mean age was 8.9 years (SD 5.9), and 61.5% were female. Celiac disease diagnosis was made before arthritis diagnosis in only 2 cases (15.4%). Median timing of celiac disease diagnosis was 3 months following arthritis diagnosis (IQR 0-19 months). Initial testing that led to the diagnosis of celiac disease was obtained by the rheumatologist in 6 cases (46.2%). Only 8 patients (61.5%) had concomitant GI symptoms, and of these, 3 patients had BMI z-scores < -1.64 and 1 had impaired linear growth. Arthritis presentation was most often oligoarticular (76.9%) and asymmetric (84.6%). The most frequently involved joint was the knee (69.2%). Most cases required systemic therapy (n=11, 84.6%) with DMARDs, biologics, or a combination of both. Of the 10 patients who required systemic therapy and reported compliance with the gluten-free diet, 3 (30%) were able to stop systemic medications. Two of 3 patients who cleared celiac serologies came off systemic medications. Statistically significant improvement was noted in the number of joints involved (p=0.02) and physician global assessment of disease activity (p=0.03) between the index and final rheumatology visit.
Conclusion: Rheumatologists play an important role in the identification of celiac disease, as arthritis was the presenting symptom in most cases and was not always associated with GI symptoms or poor weight gain. The arthritis is most often oligoarticular and asymmetric. Most children required systemic therapy. The gluten-free diet may not be sufficient to manage arthritis, but antibody clearance may be an indicator of higher likelihood of disease control off medications. Nevertheless, outcomes are promising with a combination of diet and medical therapy.
Disclosures: A. Altaffer, None; P. Weiss, None.

