Back
Poster Session B
Fibrosing rheumatic diseases (scleroderma, MCTD, IgG4-related disease, scleroderma mimics)
Session: (1046–1070) Systemic Sclerosis and Related Disorders – Clinical Poster I
1050: Clinically Recognized Depression and Mental Health Treatment in a Single Center Cohort of Patients with Systemic Sclerosis
Sunday, November 13, 2022
9:00 AM – 10:30 AM Eastern Time
Location: Virtual Poster Hall
- MS
Marissa Savoie, MD, BA
Massachusetts General Hospital
Boston, MA, United States
Abstract Poster Presenter(s)
Marissa Savoie1, Alexandra Poeschla1, na lu2, Yuqing Zhang3, Marcy Bolster1, Sara Schoenfeld1 and Flavia Castelino1, 1Massachusetts General Hospital, Boston, MA, 2Arthritis Research Canada, Boston, MA, 3Massachusetts General Hospital, Quincy, MA
Background/Purpose: The prevalence of depression among patients with systemic sclerosis (SSc) is 35-65%1, yet little is known about mental health care utilization in SSc. It is unclear whether depressive symptoms are influenced by somatic symptoms or if psychological coping relates to functional impairment and prognosis. In this study, we describe mental health diagnoses, depression treatment, and symptom burden in SSc in relation to Center for Epidemiologic Studies Depression Scale Revised (CESD-R) scores.
Methods: The Prospective Registry in Scleroderma at Massachusetts General Hospital (PRISM) is a longitudinal registry of SSc patients, followed annually. All participants fulfill the 2013 American College of Rheumatology / European League Against Rheumatism Classification for SSc and completed the CESD-R at least once. Physicians were notified about elevated CESD-R scores in real-time to prompt evaluation. Among participants with CESD-R score ≥16, indicating possible depression, a chart review was performed for mental health diagnoses and treatment. We examined the relation of demographic and clinical factors to presence of recognized mental health diagnosis or treatment using logistic regression. Further, we evaluated association of SSc symptom burden and Covid-19 pandemic with continuous CESD-R score using linear regression.
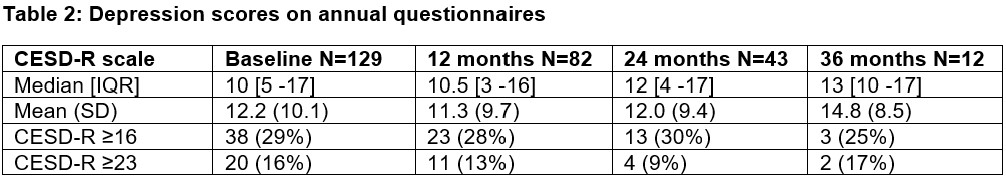
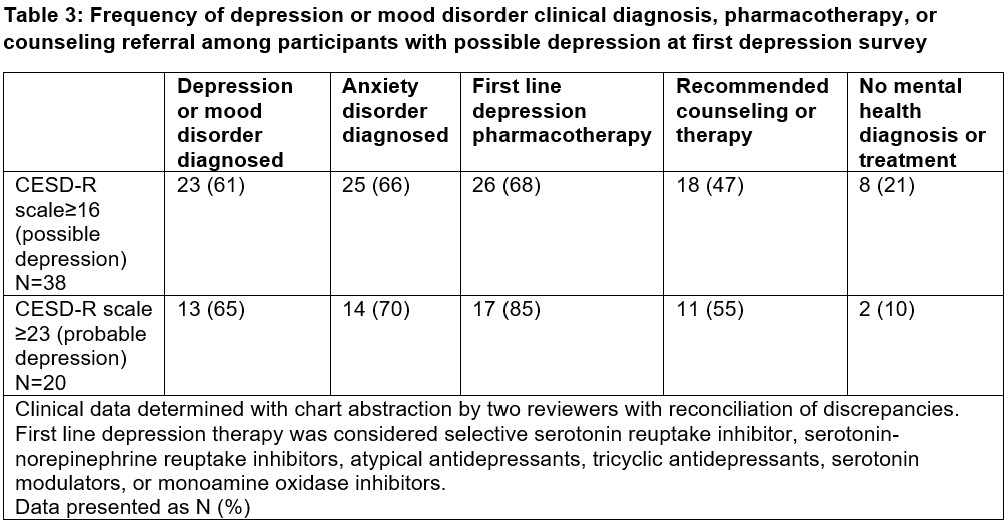
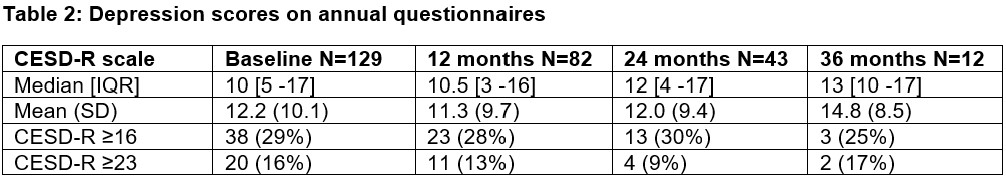
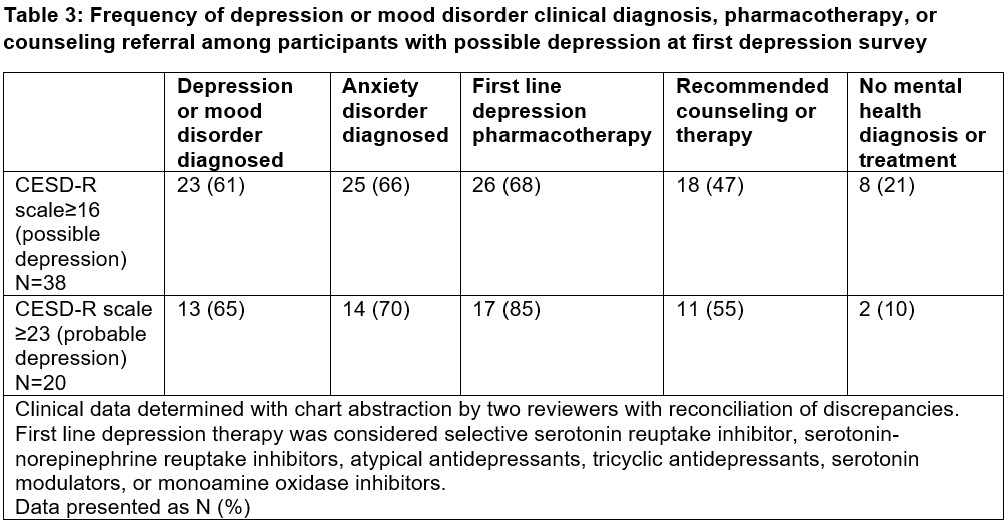
Results: Of 214 patients enrolled in PRISM, 129 participants (38% diffuse, 59% limited, and 3% sine scleroderma) completed at least one CESD-R questionnaire (Table 1). At first survey 29% had possible depression (CESD-R ≥16) and 16% had probable depression (CESD-R ≥23) (Table 2). Median depression scores were similar over 3 years of annual follow-up although significant loss to follow-up occurred. Of 38 participants with possible depression (CESD-R ≥16), 61% were diagnosed with a depressive disorder and 68% received first-line medication for depression (Table 3). In a multivariable logistic regression model, none of the evaluated variables (CESD-R score, age, gender, employment status, race, ethnicity) were associated with mental health diagnosis or treatment among participants with CESD-R ≥16. Higher Mahler’s dyspnea index (MDI) and University of California Los Angeles Scleroderma Clinical Trials Consortium Gastrointestinal (UCLA SCTC GIT) total score were associated with higher CESD-R score (p=0.01, p< 0.01 respectively).
Conclusion: In this single center, longitudinal SSc cohort completing annual depression questionnaires, 29% had significant depressive symptoms, but only a minority (10%) of participants with probable depression were not clinically diagnosed with or treated for a mental health condition. Similar to prior studies, dyspnea and gastrointestinal symptoms were associated with depression symptoms. Depression questionnaires in clinical practice may offer a way to identify mood disorders among patients with SSc.
References
1. Thombs BD, Hudson M, Taillefer SS, Baron M, Canadian Scleroderma Research Group. Prevalence and clinical correlates of symptoms of depression in patients with systemic sclerosis. Arthritis Rheum 2008;59(4):504–509.
.jpg)
Disclosures: M. Savoie, None; A. Poeschla, None; n. lu, None; Y. Zhang, ChemoCentryx; M. Bolster, Johnson and Johnson, Merck Manual, Cumberland, Corbus Inc., PracticeUpdate, Rheumatology Research Foundation; S. Schoenfeld, None; F. Castelino, Boehringer-Ingelheim.
Background/Purpose: The prevalence of depression among patients with systemic sclerosis (SSc) is 35-65%1, yet little is known about mental health care utilization in SSc. It is unclear whether depressive symptoms are influenced by somatic symptoms or if psychological coping relates to functional impairment and prognosis. In this study, we describe mental health diagnoses, depression treatment, and symptom burden in SSc in relation to Center for Epidemiologic Studies Depression Scale Revised (CESD-R) scores.
Methods: The Prospective Registry in Scleroderma at Massachusetts General Hospital (PRISM) is a longitudinal registry of SSc patients, followed annually. All participants fulfill the 2013 American College of Rheumatology / European League Against Rheumatism Classification for SSc and completed the CESD-R at least once. Physicians were notified about elevated CESD-R scores in real-time to prompt evaluation. Among participants with CESD-R score ≥16, indicating possible depression, a chart review was performed for mental health diagnoses and treatment. We examined the relation of demographic and clinical factors to presence of recognized mental health diagnosis or treatment using logistic regression. Further, we evaluated association of SSc symptom burden and Covid-19 pandemic with continuous CESD-R score using linear regression.
Results: Of 214 patients enrolled in PRISM, 129 participants (38% diffuse, 59% limited, and 3% sine scleroderma) completed at least one CESD-R questionnaire (Table 1). At first survey 29% had possible depression (CESD-R ≥16) and 16% had probable depression (CESD-R ≥23) (Table 2). Median depression scores were similar over 3 years of annual follow-up although significant loss to follow-up occurred. Of 38 participants with possible depression (CESD-R ≥16), 61% were diagnosed with a depressive disorder and 68% received first-line medication for depression (Table 3). In a multivariable logistic regression model, none of the evaluated variables (CESD-R score, age, gender, employment status, race, ethnicity) were associated with mental health diagnosis or treatment among participants with CESD-R ≥16. Higher Mahler’s dyspnea index (MDI) and University of California Los Angeles Scleroderma Clinical Trials Consortium Gastrointestinal (UCLA SCTC GIT) total score were associated with higher CESD-R score (p=0.01, p< 0.01 respectively).
Conclusion: In this single center, longitudinal SSc cohort completing annual depression questionnaires, 29% had significant depressive symptoms, but only a minority (10%) of participants with probable depression were not clinically diagnosed with or treated for a mental health condition. Similar to prior studies, dyspnea and gastrointestinal symptoms were associated with depression symptoms. Depression questionnaires in clinical practice may offer a way to identify mood disorders among patients with SSc.
References
1. Thombs BD, Hudson M, Taillefer SS, Baron M, Canadian Scleroderma Research Group. Prevalence and clinical correlates of symptoms of depression in patients with systemic sclerosis. Arthritis Rheum 2008;59(4):504–509.
.jpg)
Disclosures: M. Savoie, None; A. Poeschla, None; n. lu, None; Y. Zhang, ChemoCentryx; M. Bolster, Johnson and Johnson, Merck Manual, Cumberland, Corbus Inc., PracticeUpdate, Rheumatology Research Foundation; S. Schoenfeld, None; F. Castelino, Boehringer-Ingelheim.

