Back
Poster Session B
Spondyloarthritis (SpA) including psoriatic arthritis (PsA)
Session: (1004–1034) Spondyloarthritis Including PsA – Diagnosis, Manifestations, and Outcomes Poster II
1030: Diagnostic Usefulness of Anti-PPM1A-IgM in Patients with Ankylosing Spondylitis
Sunday, November 13, 2022
9:00 AM – 10:30 AM Eastern Time
Location: Virtual Poster Hall
- YL
Yeo-Jin Lee, MD
Asan medical center
Songpa-gu, Seoul, South Korea
Abstract Poster Presenter(s)
Yeo jin lee1, Eun-Ju Lee2, Soo Min Ahn2, Seokchan Hong2, Ji Seon Oh3, Chang Keun Lee2, Bin Yoo2 and Yong Gil Kim2, 1Asan medical center, Seoul, Republic of Korea, 2Department of Rheumatology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Republic of Korea, Seoul, Republic of Korea, 3Department of Information Medicine, Big Data Research Center, Asan Medical Center, Seoul, Republic of Korea
Background/Purpose: Ankylosing spondylitis (AS) has been known to have auto-inflammatory nature, hence, the efficacy of autoantibodies is low. However, studies on autoantibodies are ongoing, with some studies showing associations. Previous studies showed that anti-PPM1A IgG was increased in patients with AS and associated with radiographic progression (ref: JS Lee et al. 2020 JCM). However, the diagnostic usefulness was limited due to relatively low sensitivity and specificity (ref: YG Kim et al. 2014 ANR). Therefore, this study aimed to evaluate the usefulness of anti-PPM1A-IgM rather than IgG in patients with active AS before anti-TNF agent administration compared with those with active rheumatoid arthritis (RA).
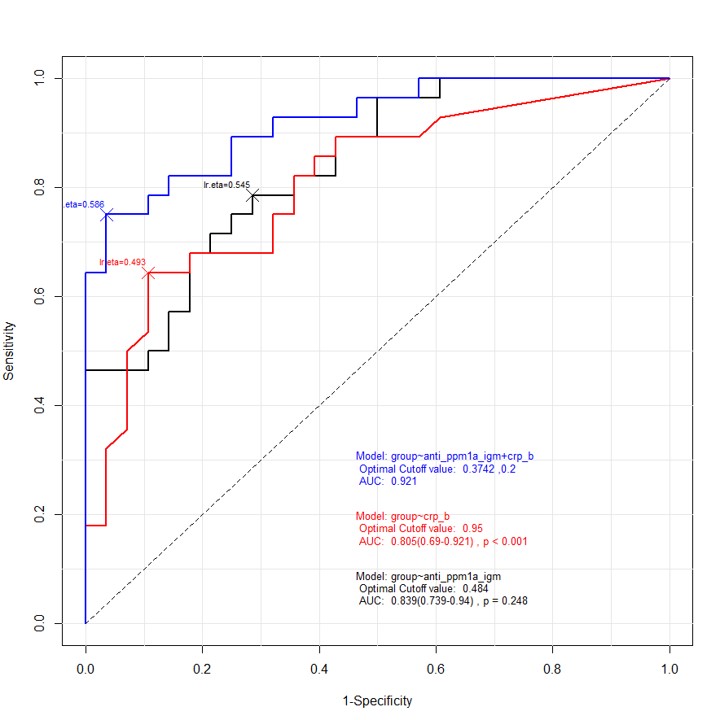
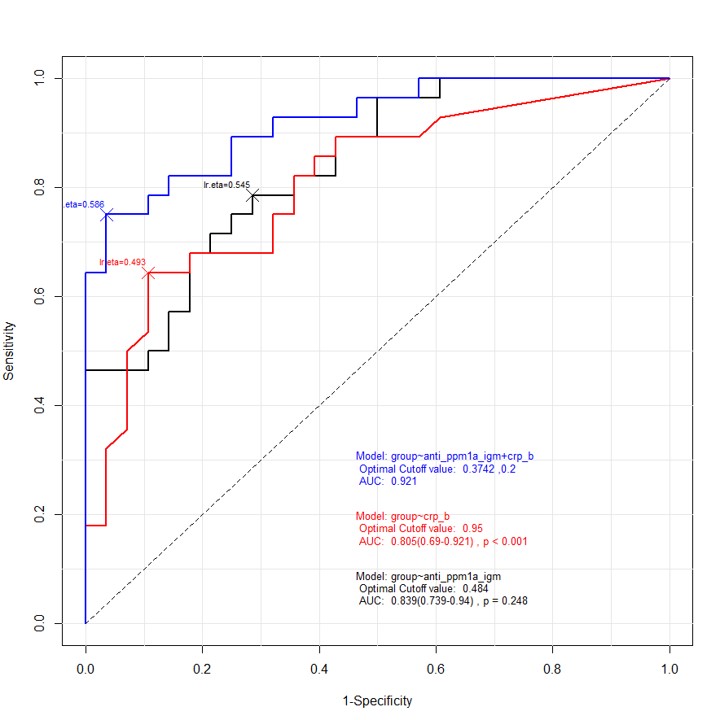
Methods: Serum samples were obtained from the registry cohort in a single-tertiary center in Korea. The serum levels of Anti-PPM1A-IgG/IgM were measured by direct sandwich enzyme-linked immunosorbent assay. Electronic medical records including laboratory data, Bath AS Disease Activity Index (BASDAI), and radiographic findings were reviewed. Receiver operating characteristic (ROC) analysis was used for the prediction of diagnostic sensitivity and specificity.
Results: Samples were collected from 16 healthy controls (HC), 28 patients diagnosed with AS, and 28 patients with RA. Anti-PPM1A-IgM was significantly lower in the AS group than that in other groups (0.39 vs. 0.62 in RA vs. 1.12 in HC, p=0.000). Among 28 patients with AS, high grade sacroiliitis (grade 3 or 4) was seen in 20 patients and HLA-B27 positivity in 27 patients; the median BASDAI was 6.00 (interquartile range, 5.35–6.80). Regarding the diagnostic usefulness of AS compared with that of RA, the area under the curve (AUC) of anti-PPM1A IgM was 0.839 (p=0.000, sensitivity 78.6%, specificity 71.4%) and of C-reactive protein (CRP) was 0.805 (p=0.000, sensitivity 64.3%, specificity 89.3%). However, anti-PPM1A-IgG and erythrocyte sedimentation rate did not show significance. When ROC analysis was performed using both CRP and anti-PPM1A-IgM, a sensitivity of 75% and specificity of 96.4% were identified with an AUC of 0.921.
Conclusion:
In conclusion, decreased level of anti-PPM1A-IgM implies high diagnostic utility in patients with active AS. Thus, when sacroiliitis cannot be checked, CRP and anti-PPM1A-IgM measurements can be used in the diagnosis of AS with differentiation from active RA.
Reference:
J Clin Med. 2020;9(12):3968
Arthritis Rheumatol. 2014;66(10):2793-2803
Disclosures: Y. lee, None; E. Lee, None; S. Ahn, None; S. Hong, None; J. Oh, None; C. Lee, None; B. Yoo, None; Y. Kim, None.
Background/Purpose: Ankylosing spondylitis (AS) has been known to have auto-inflammatory nature, hence, the efficacy of autoantibodies is low. However, studies on autoantibodies are ongoing, with some studies showing associations. Previous studies showed that anti-PPM1A IgG was increased in patients with AS and associated with radiographic progression (ref: JS Lee et al. 2020 JCM). However, the diagnostic usefulness was limited due to relatively low sensitivity and specificity (ref: YG Kim et al. 2014 ANR). Therefore, this study aimed to evaluate the usefulness of anti-PPM1A-IgM rather than IgG in patients with active AS before anti-TNF agent administration compared with those with active rheumatoid arthritis (RA).
Methods: Serum samples were obtained from the registry cohort in a single-tertiary center in Korea. The serum levels of Anti-PPM1A-IgG/IgM were measured by direct sandwich enzyme-linked immunosorbent assay. Electronic medical records including laboratory data, Bath AS Disease Activity Index (BASDAI), and radiographic findings were reviewed. Receiver operating characteristic (ROC) analysis was used for the prediction of diagnostic sensitivity and specificity.
Results: Samples were collected from 16 healthy controls (HC), 28 patients diagnosed with AS, and 28 patients with RA. Anti-PPM1A-IgM was significantly lower in the AS group than that in other groups (0.39 vs. 0.62 in RA vs. 1.12 in HC, p=0.000). Among 28 patients with AS, high grade sacroiliitis (grade 3 or 4) was seen in 20 patients and HLA-B27 positivity in 27 patients; the median BASDAI was 6.00 (interquartile range, 5.35–6.80). Regarding the diagnostic usefulness of AS compared with that of RA, the area under the curve (AUC) of anti-PPM1A IgM was 0.839 (p=0.000, sensitivity 78.6%, specificity 71.4%) and of C-reactive protein (CRP) was 0.805 (p=0.000, sensitivity 64.3%, specificity 89.3%). However, anti-PPM1A-IgG and erythrocyte sedimentation rate did not show significance. When ROC analysis was performed using both CRP and anti-PPM1A-IgM, a sensitivity of 75% and specificity of 96.4% were identified with an AUC of 0.921.
Conclusion:
In conclusion, decreased level of anti-PPM1A-IgM implies high diagnostic utility in patients with active AS. Thus, when sacroiliitis cannot be checked, CRP and anti-PPM1A-IgM measurements can be used in the diagnosis of AS with differentiation from active RA.
Reference:
J Clin Med. 2020;9(12):3968
Arthritis Rheumatol. 2014;66(10):2793-2803
Disclosures: Y. lee, None; E. Lee, None; S. Ahn, None; S. Hong, None; J. Oh, None; C. Lee, None; B. Yoo, None; Y. Kim, None.

