Back
Poster Session B
Epidemiology, health policy and outcomes
Session: (0724–0751) Health Services Research Poster II
0739: Effect of Tailored Self-Management Interventions on Health Outcomes in Individuals with Chronic Musculoskeletal Conditions
Sunday, November 13, 2022
9:00 AM – 10:30 AM Eastern Time
Location: Virtual Poster Hall
- EW
Ellen Wang, MSc
University of British Columbia, Arthritis Research Canada
Vancouver, BC, Canada
Abstract Poster Presenter(s)
Ellen Wang1, Isabel Rodrigues2 and Linda Li3, 1University of British Columbia, Arthritis Research Canada, Vancouver, BC, Canada, 2McMaster University, GERAS Centre for Aging Research, Hamilton, ON, Canada, 3University of British Columbia, Vancouver, BC, Canada
Background/Purpose: Self-management, has been recognized as an essential component of successful chronic musculoskeletal (MSK) management; yet existing reviews of self-management interventions have found only modest effects. Tailoring is the act of aligning and tuning components of the intervention to the unique characteristics of an individual. Thus, tailored self-management interventions account for patient needs, preferences, and values; and improve the perceived relevance of knowledge, problem-solving, symptom management, healthy behaviours, patient-provider communication, and use of community resources. Our aim is to determine the effect of tailored self-management interventions on health outcomes for individuals living with chronic MSK conditions.
Methods: We searched 5 databases (MEDLINE, EMBASE, CINAHL, PsycINFO, CENTRAL) and appropriate grey literature (i.e., Open Science Database, ProQuest Dissertations and Theses) for articles published up to January 31st, 2022. Two independent reviewers screened the titles/abstracts and reviewed the full articles of those meeting eligibility. Studies were eligible if they were available in English and included 1) individually prescribed interventions based on subjective and objective assessments; 2) participants with an existing chronic MSK condition (ICD-10); 3) a non-tailored or usual care control. We conducted meta-analyses for the outcomes of pain, physical function, and quality of life. Methodological quality was evaluated using the Cochrane risk-of-bias tool.
Results: Our search yielded 1558 articles; of those, 26 articles (described 20 unique interventions) met the eligibility criteria. All 20 were randomized controlled trials (RCTs) and included participants with inflammatory arthritis, osteoarthritis, and chronic pain conditions. Interventions were multimodal and 90% included a combination of self-management education, exercise/physical activity, or cognitive/behavioural counselling. Pain was assessed by Visual Analogue Scale/Numeric Rating Scale (VAS/NRS) and Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain. Combining 3 studies with 456 participants, a moderate effect was found in VAS/NRS pain with a SMD= -0.59 [95% CI: -0.78, -0.40, p< 0.001]. Combining 3 studies with 564 participants a small effect was found in WOMAC pain, SMD= -0.12 [95% CI: -0.46, 0.23, p= 0.50] (Fig 1). 5 RCTs with 1181 participants evaluated physical function. The pooled analysis of WOMAC physical function and Short Form Health Survey physical component found a small effect, SMD= 0.07 [95% CI (-0.06, 0.21), p= 0.29] (Fig 2). 3 RCTs with 731 participants evaluated quality of life (QoL). The pooled analysis of Assessment of QoL, Rheumatoid Arthritis QoL and EuroQol 5 Dimension 3 Levels found a small effect, SMD= 0.07 [95% CI: -0.07, 0.22, p= 0.34] (Fig 3). All meta-analyzed interventions were at high risk of bias for participant blinding.
Conclusion: Tailored self-management interventions were found to have a moderate effect on VAS/NRS pain; and non-significant effects on WOMAC pain, physical function, and quality of life. More research is needed to determine the optimal combination of modalities.
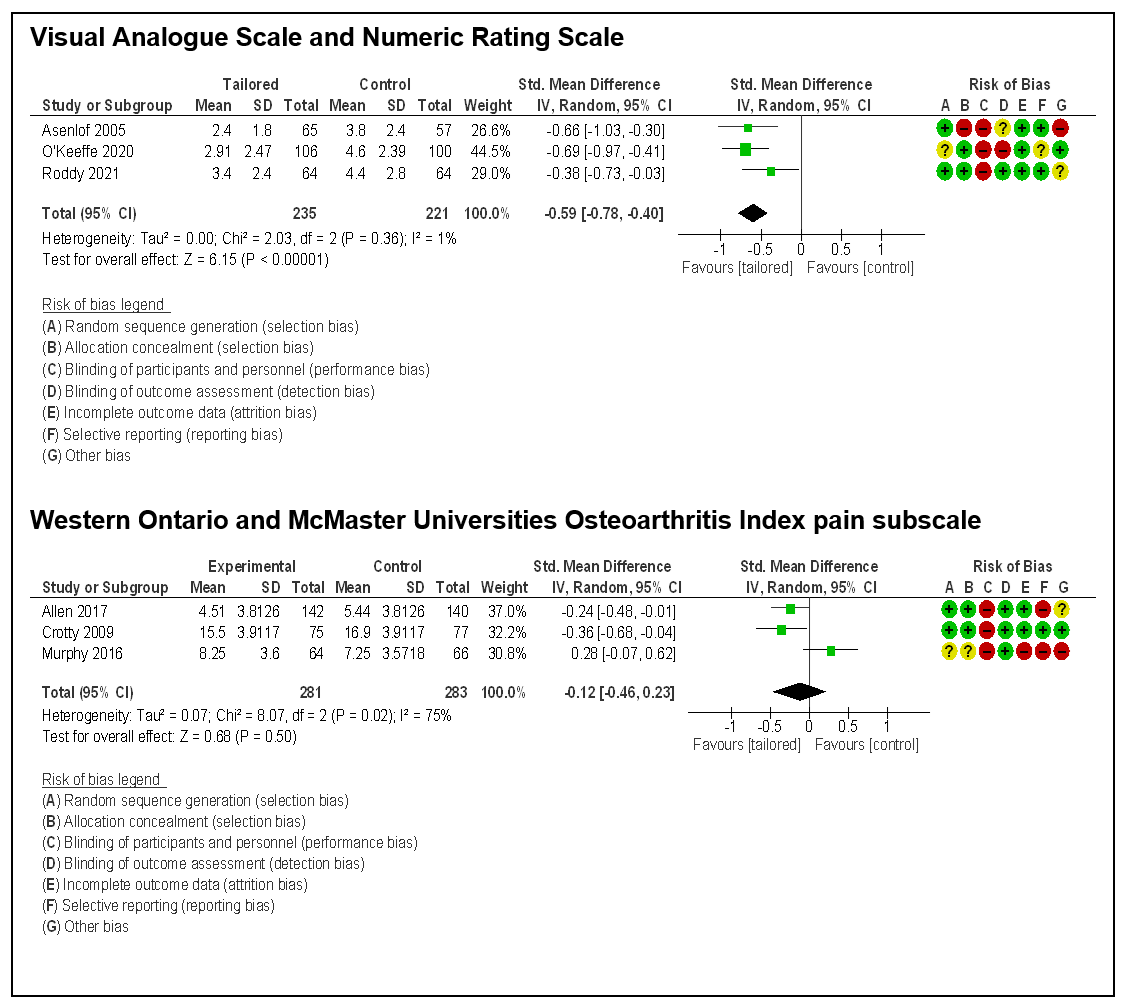 Figure 1 - Pain
Figure 1 - Pain
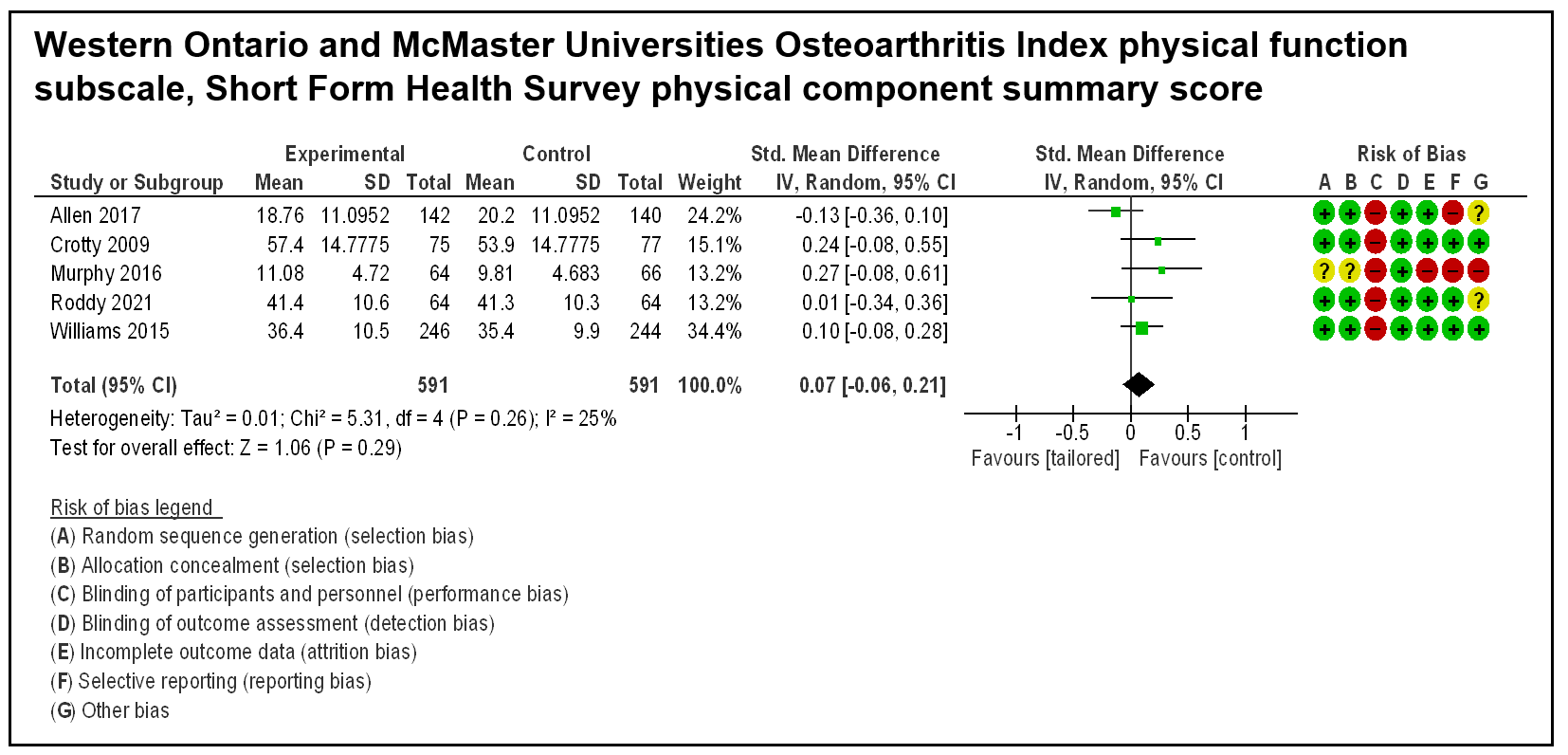 Figure 2 - Physical Function
Figure 2 - Physical Function
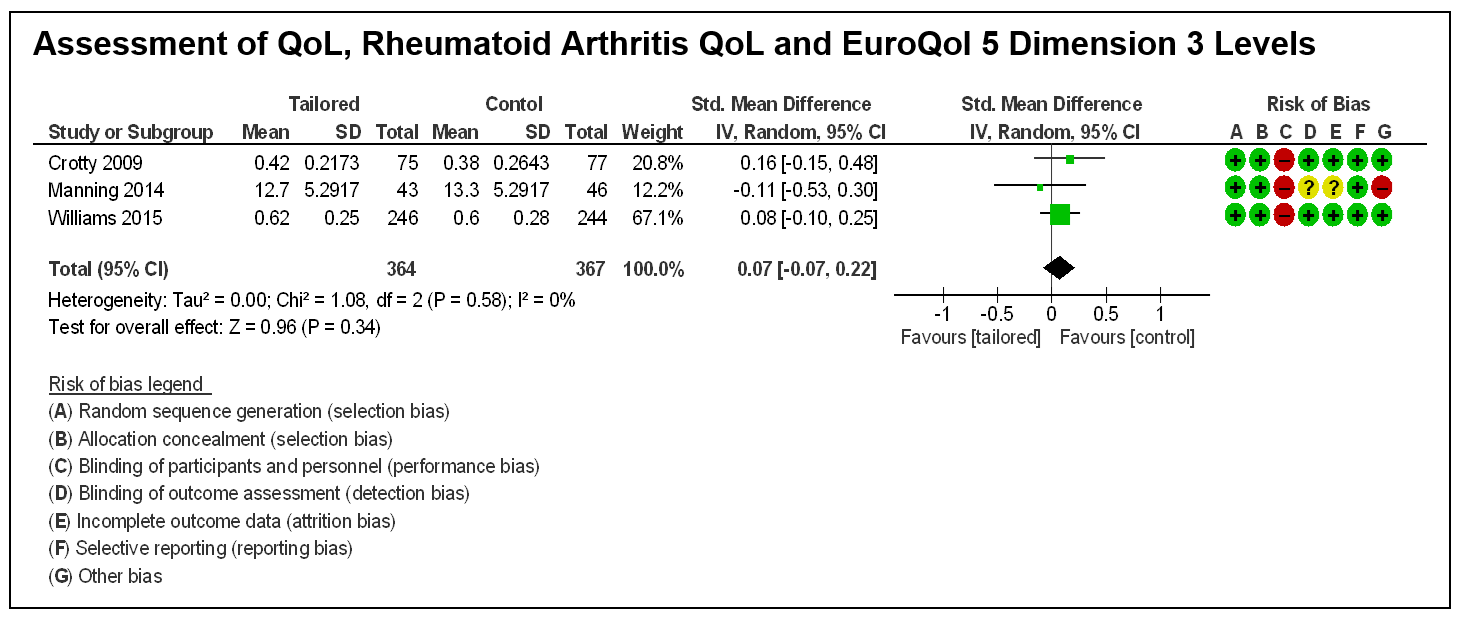 Figure 3 - Quality of Life
Figure 3 - Quality of Life
Disclosures: E. Wang, None; I. Rodrigues, None; L. Li, None.
Background/Purpose: Self-management, has been recognized as an essential component of successful chronic musculoskeletal (MSK) management; yet existing reviews of self-management interventions have found only modest effects. Tailoring is the act of aligning and tuning components of the intervention to the unique characteristics of an individual. Thus, tailored self-management interventions account for patient needs, preferences, and values; and improve the perceived relevance of knowledge, problem-solving, symptom management, healthy behaviours, patient-provider communication, and use of community resources. Our aim is to determine the effect of tailored self-management interventions on health outcomes for individuals living with chronic MSK conditions.
Methods: We searched 5 databases (MEDLINE, EMBASE, CINAHL, PsycINFO, CENTRAL) and appropriate grey literature (i.e., Open Science Database, ProQuest Dissertations and Theses) for articles published up to January 31st, 2022. Two independent reviewers screened the titles/abstracts and reviewed the full articles of those meeting eligibility. Studies were eligible if they were available in English and included 1) individually prescribed interventions based on subjective and objective assessments; 2) participants with an existing chronic MSK condition (ICD-10); 3) a non-tailored or usual care control. We conducted meta-analyses for the outcomes of pain, physical function, and quality of life. Methodological quality was evaluated using the Cochrane risk-of-bias tool.
Results: Our search yielded 1558 articles; of those, 26 articles (described 20 unique interventions) met the eligibility criteria. All 20 were randomized controlled trials (RCTs) and included participants with inflammatory arthritis, osteoarthritis, and chronic pain conditions. Interventions were multimodal and 90% included a combination of self-management education, exercise/physical activity, or cognitive/behavioural counselling. Pain was assessed by Visual Analogue Scale/Numeric Rating Scale (VAS/NRS) and Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain. Combining 3 studies with 456 participants, a moderate effect was found in VAS/NRS pain with a SMD= -0.59 [95% CI: -0.78, -0.40, p< 0.001]. Combining 3 studies with 564 participants a small effect was found in WOMAC pain, SMD= -0.12 [95% CI: -0.46, 0.23, p= 0.50] (Fig 1). 5 RCTs with 1181 participants evaluated physical function. The pooled analysis of WOMAC physical function and Short Form Health Survey physical component found a small effect, SMD= 0.07 [95% CI (-0.06, 0.21), p= 0.29] (Fig 2). 3 RCTs with 731 participants evaluated quality of life (QoL). The pooled analysis of Assessment of QoL, Rheumatoid Arthritis QoL and EuroQol 5 Dimension 3 Levels found a small effect, SMD= 0.07 [95% CI: -0.07, 0.22, p= 0.34] (Fig 3). All meta-analyzed interventions were at high risk of bias for participant blinding.
Conclusion: Tailored self-management interventions were found to have a moderate effect on VAS/NRS pain; and non-significant effects on WOMAC pain, physical function, and quality of life. More research is needed to determine the optimal combination of modalities.
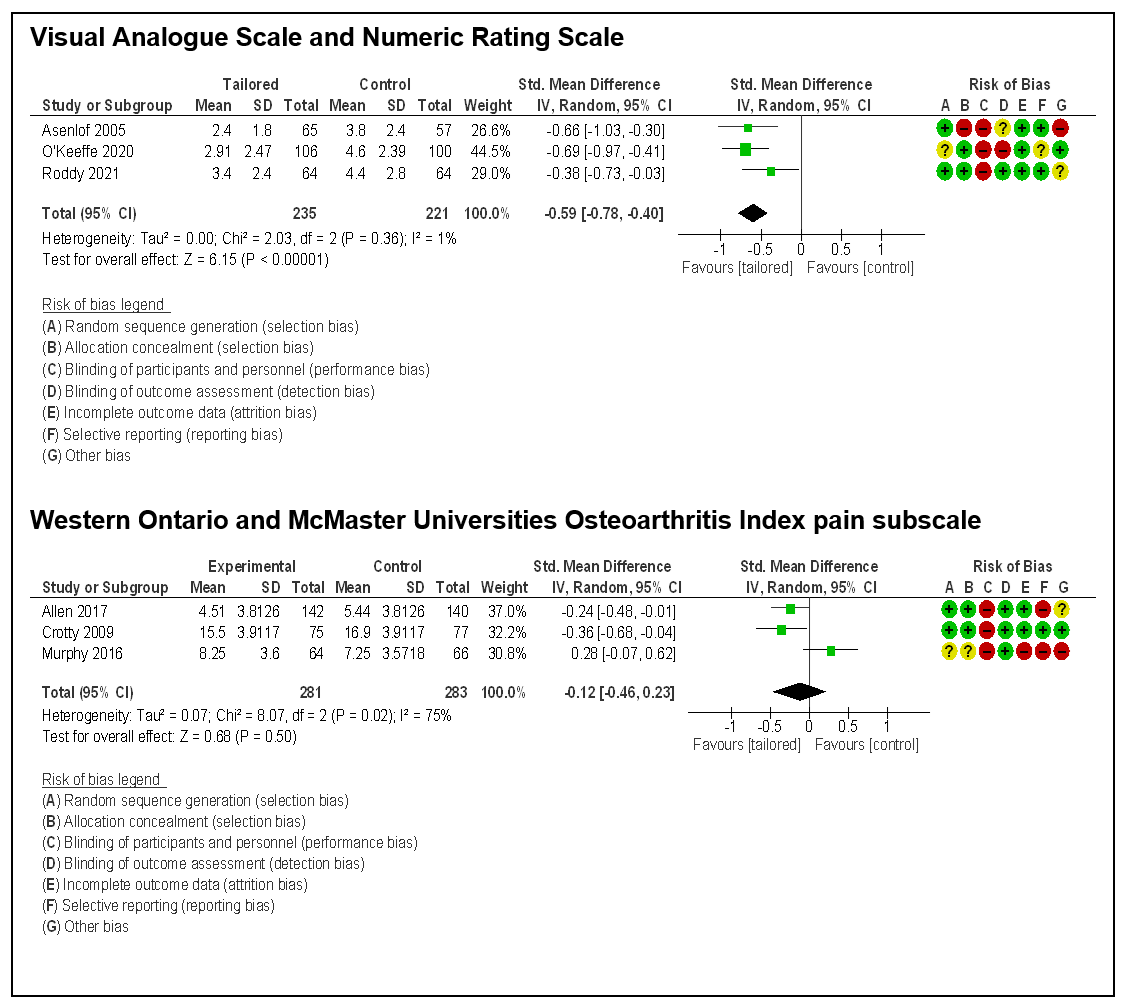 Figure 1 - Pain
Figure 1 - Pain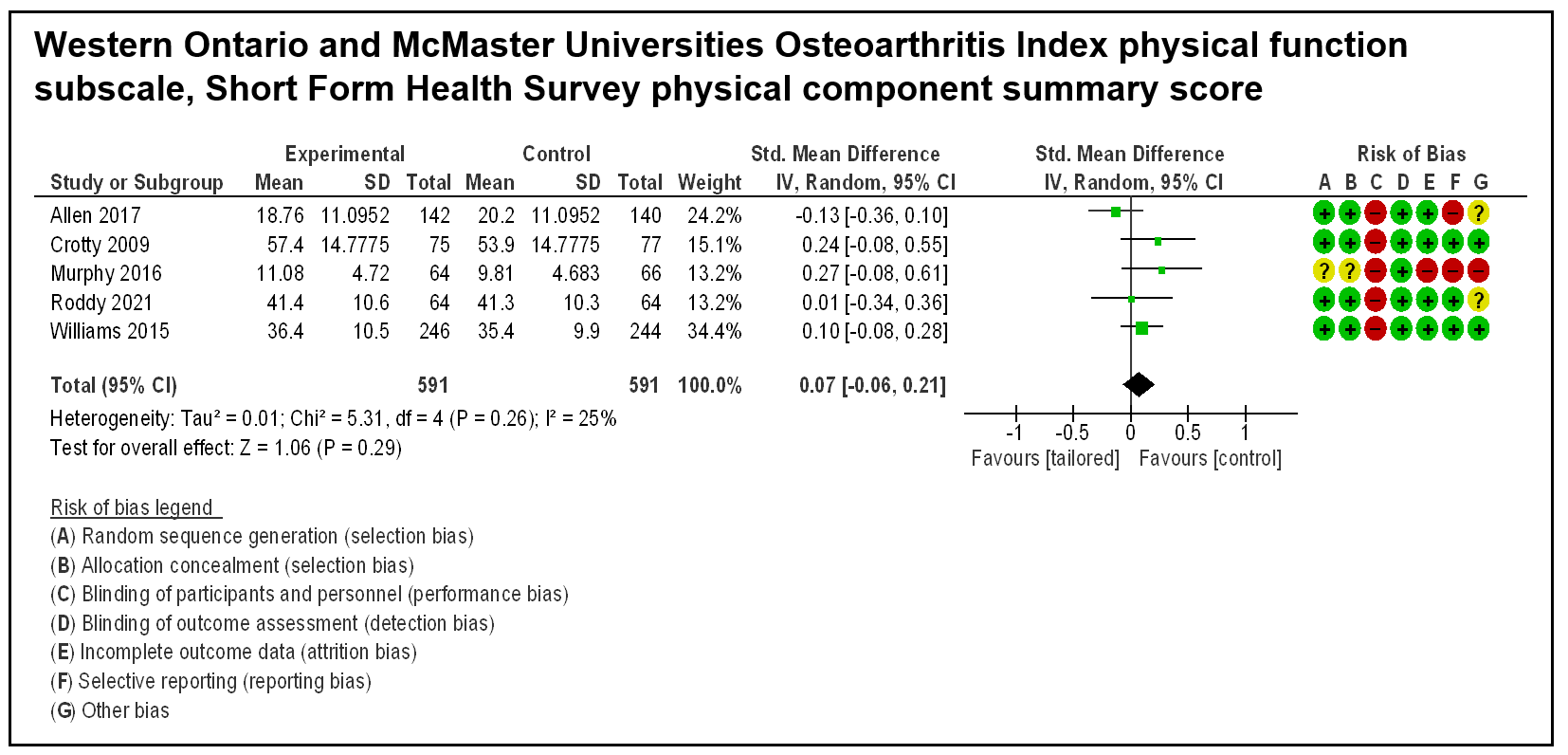 Figure 2 - Physical Function
Figure 2 - Physical Function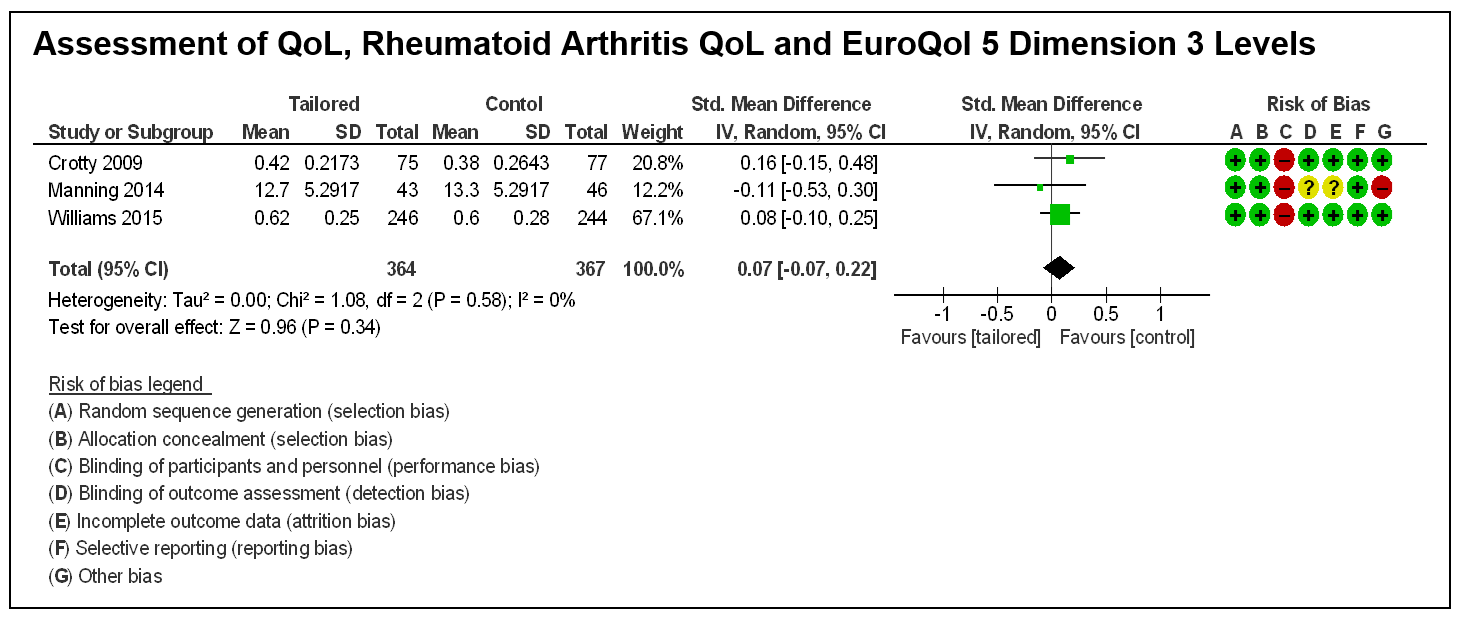 Figure 3 - Quality of Life
Figure 3 - Quality of Life Disclosures: E. Wang, None; I. Rodrigues, None; L. Li, None.

