Back
Poster Session B
Antiphospholipid Syndrome
Session: (0671–0694) Antiphospholipid Syndrome Poster
0672: Immune Thrombocytopenia Could Be an Independent Phenotype of Primary Antiphospholipid Syndrome
Sunday, November 13, 2022
9:00 AM – 10:30 AM Eastern Time
Location: Virtual Poster Hall
- YS
Yu Shi, MD
Chinese Academy of Medical Sciences, Peking Union Medical College
Dongcheng Qu, Beijing, China
Abstract Poster Presenter(s)
Yu Shi1, Jiuliang Zhao2 and Xiaofeng Zeng2, 1Chinese Academy of Medical Sciences, Peking Union Medical College, Dongcheng Qu, China, 2Department of Rheumatology, Peking Union Medical College Hospital (PUMCH), Chinese Academy of Medical Sciences National Clinical Research Center for Dermatologic and Immunologic Diseases (NCRC-DID), Beijing, China
Background/Purpose: Among patients with immune thrombocytopenia (ITP), 10-30% of them were found with positive antiphospholipid antibodies (aPLs) but without typical clinical manifestations of antiphospholipid syndrome (APS), especially thrombotic events.
Methods: This is a single center prospective cohort study consecutively enrolling thrombocytopenic patients with continuous positive aPLs. Patients developing thrombotic events are classified as the APS group. Then we compare the clinical characteristics and prognosis between aPLs carriers and patients with APS.
Results: This cohort included 47 thrombocytopenic patients with continuous positive aPLs and 55 with diagnosed primary APS. The proportion of multiple risk factors of thrombosis including smoking, hypertension, and higher levels of homocysteine are higher in the APS group (p = 0.03, 0.04, 0.03, respectively) (Table 1). The platelet count of aPLs carriers at admission was lower than APS patients [26×109/L (9×109/L, 46×109/L) vs 64×109/L (24×109/L, 89×109/L), p = 0.0002]. The proportion of positive anti-β2-glycoprotein I, anticardiolipin and lupus anticoagulant separately was similar, but triple aPLs positivity is more common in primary APS patients with thrombocytopenia [24 (51.1%) vs 40 (72.7%), p = 0.04]. Regarding the treatment response, the complete response (CR) rate is similar between aPLs carriers and primary APS patients with thrombocytopenia (p = 0.2). Nonetheless, the proportion of response, no response and relapse differed significantly between the two groups [13 (27.7%) vs 4 (7.3%), p < 0.0001; 5 (10.6%) vs 8 (14.5%), p < 0.0001; 5 (10.6%) vs 8 (14.5%), p < 0.0001, respectively]. In Kaplan-Meier analysis (Figure 1), primary APS patients had significantly more thrombotic events than aPLs carriers (p = 0.0006).
Conclusion: In the absence of other high risk factor for thrombosis, Thrombocytopenia could be an independent and long-lasting clinical phenotype for aPLs carriers.
.jpg) Table 1. Demographic and clinical characteristics of aPLs carriers and primary APS patients with thrombocytopenia.
Table 1. Demographic and clinical characteristics of aPLs carriers and primary APS patients with thrombocytopenia.
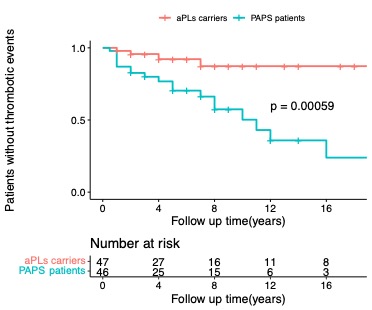 Figure 1. Kaplan-Meier curve of thrombotic events between aPLs carriers and primary APS patients with thrombocytopenia.
Figure 1. Kaplan-Meier curve of thrombotic events between aPLs carriers and primary APS patients with thrombocytopenia.
Disclosures: Y. Shi, None; J. Zhao, None; X. Zeng, None.
Background/Purpose: Among patients with immune thrombocytopenia (ITP), 10-30% of them were found with positive antiphospholipid antibodies (aPLs) but without typical clinical manifestations of antiphospholipid syndrome (APS), especially thrombotic events.
Methods: This is a single center prospective cohort study consecutively enrolling thrombocytopenic patients with continuous positive aPLs. Patients developing thrombotic events are classified as the APS group. Then we compare the clinical characteristics and prognosis between aPLs carriers and patients with APS.
Results: This cohort included 47 thrombocytopenic patients with continuous positive aPLs and 55 with diagnosed primary APS. The proportion of multiple risk factors of thrombosis including smoking, hypertension, and higher levels of homocysteine are higher in the APS group (p = 0.03, 0.04, 0.03, respectively) (Table 1). The platelet count of aPLs carriers at admission was lower than APS patients [26×109/L (9×109/L, 46×109/L) vs 64×109/L (24×109/L, 89×109/L), p = 0.0002]. The proportion of positive anti-β2-glycoprotein I, anticardiolipin and lupus anticoagulant separately was similar, but triple aPLs positivity is more common in primary APS patients with thrombocytopenia [24 (51.1%) vs 40 (72.7%), p = 0.04]. Regarding the treatment response, the complete response (CR) rate is similar between aPLs carriers and primary APS patients with thrombocytopenia (p = 0.2). Nonetheless, the proportion of response, no response and relapse differed significantly between the two groups [13 (27.7%) vs 4 (7.3%), p < 0.0001; 5 (10.6%) vs 8 (14.5%), p < 0.0001; 5 (10.6%) vs 8 (14.5%), p < 0.0001, respectively]. In Kaplan-Meier analysis (Figure 1), primary APS patients had significantly more thrombotic events than aPLs carriers (p = 0.0006).
Conclusion: In the absence of other high risk factor for thrombosis, Thrombocytopenia could be an independent and long-lasting clinical phenotype for aPLs carriers.
.jpg) Table 1. Demographic and clinical characteristics of aPLs carriers and primary APS patients with thrombocytopenia.
Table 1. Demographic and clinical characteristics of aPLs carriers and primary APS patients with thrombocytopenia.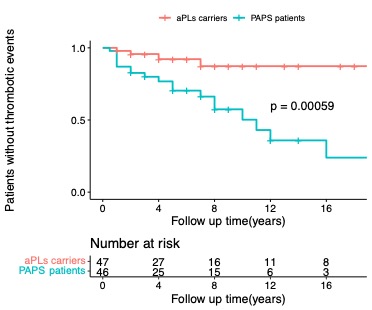 Figure 1. Kaplan-Meier curve of thrombotic events between aPLs carriers and primary APS patients with thrombocytopenia.
Figure 1. Kaplan-Meier curve of thrombotic events between aPLs carriers and primary APS patients with thrombocytopenia.Disclosures: Y. Shi, None; J. Zhao, None; X. Zeng, None.

