Back
Poster Session B
Infection-related rheumatic syndromes
Session: (0779–0806) Infection-related Rheumatic Disease Poster
0804: Incidence and Risk Factors of Active Tuberculosis in Patients with Rheumatic Diseases Complicated with Tuberculosis Infection: A Multicenter Prospective Cohort Study
Sunday, November 13, 2022
9:00 AM – 10:30 AM Eastern Time
Location: Virtual Poster Hall
- YL
Yuchen Liu, MD
Peking Union Medical College Hospital
Beijing, Beijing, China
Abstract Poster Presenter(s)
Lifan Zhang1, yuchen liu2, xiaoqing zou3, shi chen2, yanan ma2, huimin ma4, qifei cao4, zhengrong yang4, Fengchun ZHANG5, Yan Zhao5, Xiaofeng Zeng6 and Xiaoqing Liu1, 1Division of Infectious Diseases, Department of Internal medicine, State Key Laboratory of Complex Severe and Rare Disease, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College; Clinical Epidemiology Unit, Peking Union Medical College, International Clinical Epidemiology Network; Center for Tuberculosis Research, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China, 2Division of Infectious Diseases, Department of Internal medicine, State Key Laboratory of Complex Severe and Rare Disease, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College; Peking Union Medical College Hospital, Peking Union Medical College, Beijing, China, 3Division of Infectious Diseases, Department of Internal medicine, State Key Laboratory of Complex Severe and Rare Disease, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College; School of Population Medicine and Public Health, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China, 4Division of Infectious Diseases, Department of Internal medicine, State Key Laboratory of Complex Severe and Rare Disease, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China, 5Peking Union Medical College Hospital, Beijing, China, 6Department of Rheumatology, Peking Union Medical College Hospital (PUMCH), Chinese Academy of Medical Sciences National Clinical Research Center for Dermatologic and Immunologic Diseases (NCRC-DID), Beijing, China
Background/Purpose: China remains a high-burden country of both rheumatic disease (RD) and tuberculosis (TB) till today. Patients with RD are considered as a high-risk population of TB, and those complicated with TB infection deserve more attention, while there is no guideline on TB prevention and management for this population. The purpose of this study was to investigate the incidence of active tuberculosis (ATB) in RD patients complicated with TB infection (including both latent tuberculosis infection [LTBI] and previous TB), and to analyze the risk factors of TB reactivation, which help formulating TB prevention and management strategies for patients with RD in China.
Methods: We conducted a multi-centered prospective cohort study. Patients confirmed of RD complicated with TB infection from both outpatient and outpatient department of 13 Grade A tertiary hospital in the eastern, central, and western regions of China from September 2014 to March 2016 were recruited. Baseline demographic characteristics, clinical diagnosis, treatment, and laboratory tests were collected. The incidence of ATB was assessed during followed up. Incidence was estimated by the Kaplan–Meier method, and differences in incidence were evaluated with a log-rank test. Multivariable analyses with the Cox proportional-hazards model were used to explore the risk factors for developing ATB.
Results: 904 patients with RD complicated with TB infection were enrolled in this study. The average age of patients in this cohort was 47±14 (mean±SD) years old, women accounted for 70.8%, patients with rheumatoid arthritis (295/904, 32.6%) and systemic lupus erythematosus (209/904, 23.1%) together accounted for more than 50% of the cohort. The median follow-up time was 72 months. During the 6-year follow-up, 26 cases of ATB occurred. The 1-year ATB incidence rate was 664/100000 (95%CI 244/100000-1439/100000), and the 5-year ATB cumulative incidence rate was 2549/100000 (95%CI 1604/100000 -3834/100000). Multivariable Cox proportional hazard model analysis showed that the maximum glucocorticoids dosage (adjusted HR [aHR]=2.43, 95%CI 1.05-5.62, p=0.039 for 30-60mg/d equivalent prednisone; aHR=4.80, 95%CI 1.49-15.44, p=0.008 for >60mg/d equivalent prednisone) and TB contact (aHR=7.25, 95%CI 2.14-24.54, p=0.001) were independent risk factors for ATB.
Conclusion: Patients with RD complicated with TB infection had a higher risk of developing ATB. The use of medium to high dosage of glucocorticoids and the history of TB exposure might be independent risk factors for developing ATB, in which case TB preventive treatment should be considered.
†: Lifan Zhang and Yuchen Liu contributed equally to this work.
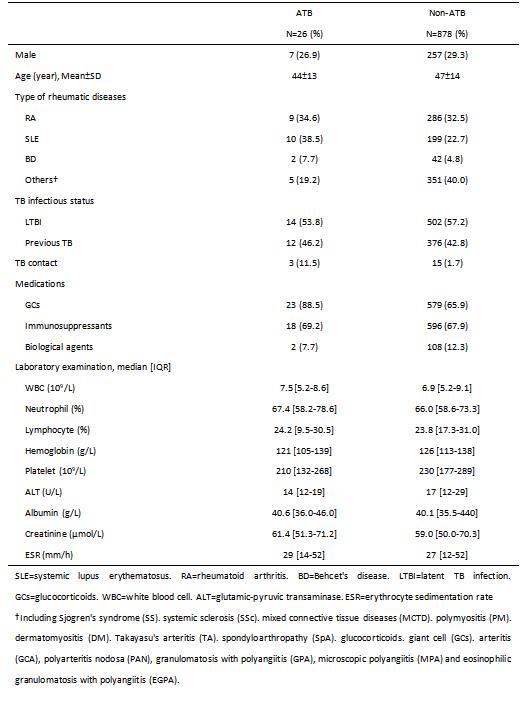 Table 1. General characteristics of 904 enrolled patients with rheumatic diseases complicated with TB infection
Table 1. General characteristics of 904 enrolled patients with rheumatic diseases complicated with TB infection
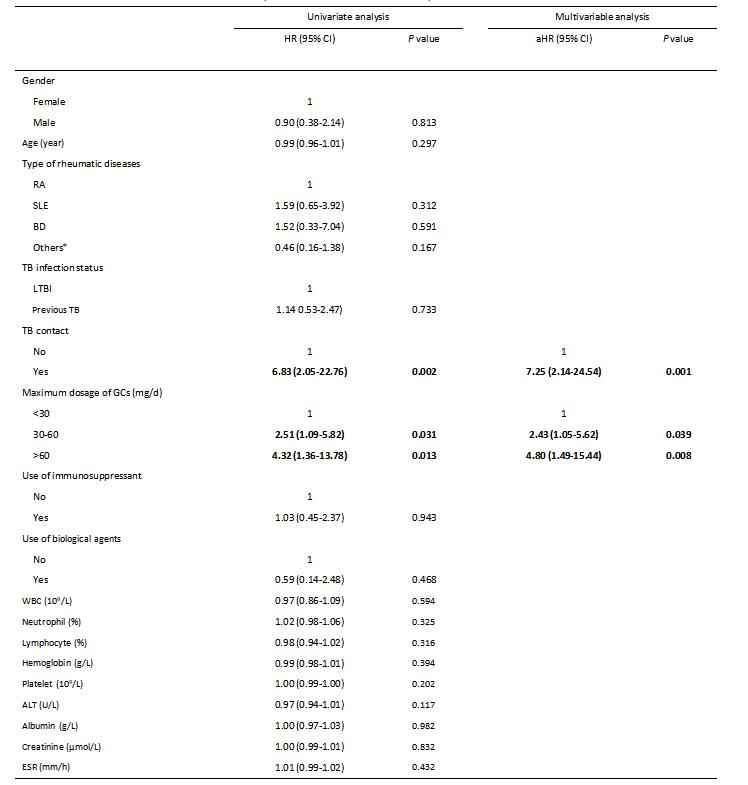 Table 2. Potential risk factors of the incidence of ATB in patients with rheumatic diseases complicated with TB infection
Table 2. Potential risk factors of the incidence of ATB in patients with rheumatic diseases complicated with TB infection
SLE=systemic lupus erythematosus. RA=rheumatoid arthritis. BD=Behcet's disease. LTBI=latent TB infection. GCs=glucocorticoids. WBC=white blood cell. ALT=glutamic-pyruvic transaminase. ESR=erythrocyte sedimentation rate
*Including Sjogren's syndrome (SS), systemic sclerosis (SSc), mixed connective tissue disease (MCTD), polymyositis (PM), dermatomyositis (DM), Takayasu arthritis (TA), giant cell arthritis (GCA), polyarteritis nodosa (PAN), granulomatosis with polyangiitis (GPA), microscopic polyarteritis (MPA), eosinophilic granulomatosis with polyangiitis (EGPA), ankylosing spondylitis (AS) and psoriatic arthritis (PsA)
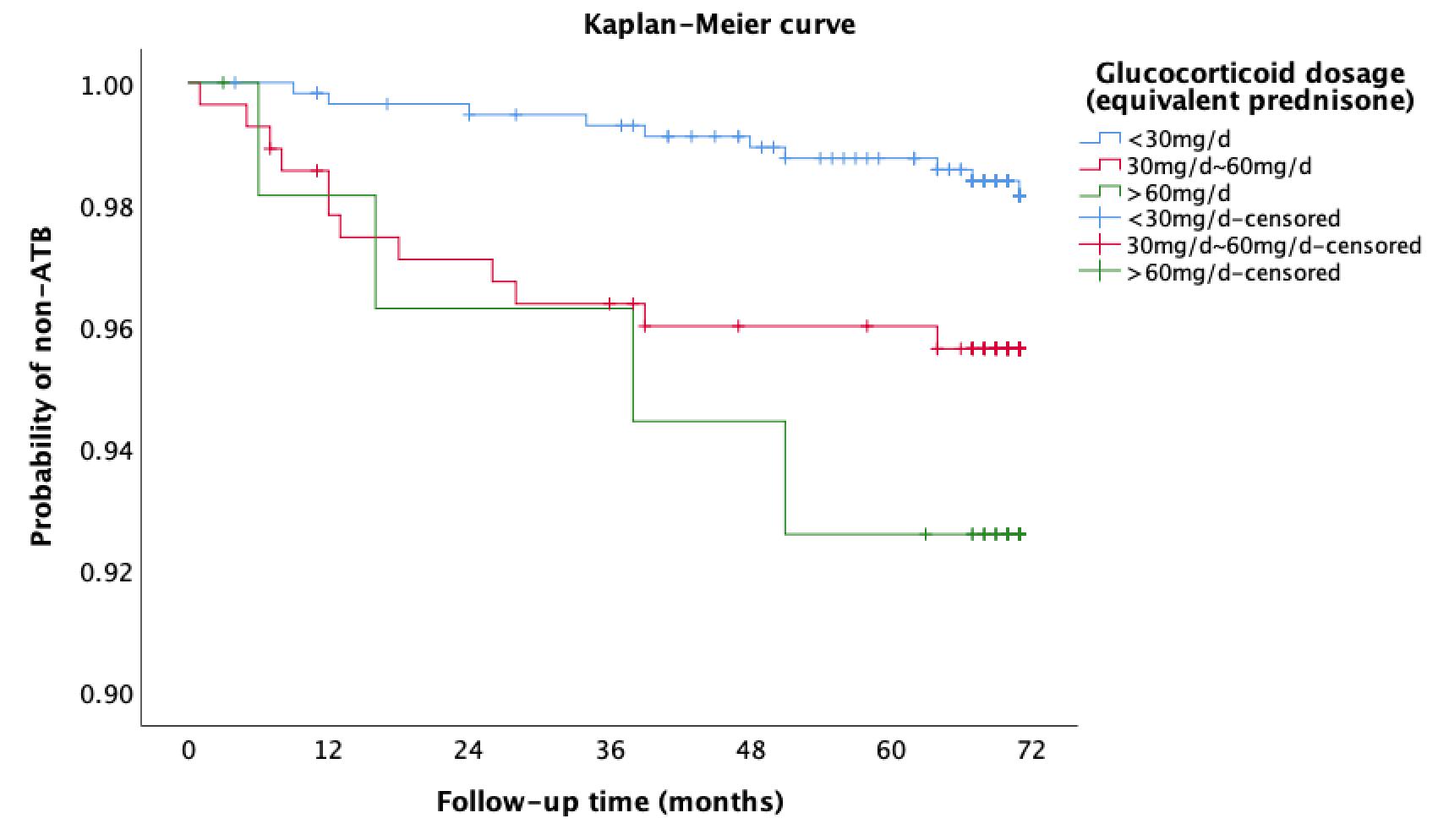 Figure 1. Incidence of ATB in patients with rheumatic diseases complicated with TB infection according to maximum daily dosage of GCs
Figure 1. Incidence of ATB in patients with rheumatic diseases complicated with TB infection according to maximum daily dosage of GCs
Disclosures: L. Zhang, None; y. liu, None; x. zou, None; s. chen, None; y. ma, None; h. ma, None; q. cao, None; z. yang, None; F. ZHANG, None; Y. Zhao, None; X. Zeng, None; X. Liu, None.
Background/Purpose: China remains a high-burden country of both rheumatic disease (RD) and tuberculosis (TB) till today. Patients with RD are considered as a high-risk population of TB, and those complicated with TB infection deserve more attention, while there is no guideline on TB prevention and management for this population. The purpose of this study was to investigate the incidence of active tuberculosis (ATB) in RD patients complicated with TB infection (including both latent tuberculosis infection [LTBI] and previous TB), and to analyze the risk factors of TB reactivation, which help formulating TB prevention and management strategies for patients with RD in China.
Methods: We conducted a multi-centered prospective cohort study. Patients confirmed of RD complicated with TB infection from both outpatient and outpatient department of 13 Grade A tertiary hospital in the eastern, central, and western regions of China from September 2014 to March 2016 were recruited. Baseline demographic characteristics, clinical diagnosis, treatment, and laboratory tests were collected. The incidence of ATB was assessed during followed up. Incidence was estimated by the Kaplan–Meier method, and differences in incidence were evaluated with a log-rank test. Multivariable analyses with the Cox proportional-hazards model were used to explore the risk factors for developing ATB.
Results: 904 patients with RD complicated with TB infection were enrolled in this study. The average age of patients in this cohort was 47±14 (mean±SD) years old, women accounted for 70.8%, patients with rheumatoid arthritis (295/904, 32.6%) and systemic lupus erythematosus (209/904, 23.1%) together accounted for more than 50% of the cohort. The median follow-up time was 72 months. During the 6-year follow-up, 26 cases of ATB occurred. The 1-year ATB incidence rate was 664/100000 (95%CI 244/100000-1439/100000), and the 5-year ATB cumulative incidence rate was 2549/100000 (95%CI 1604/100000 -3834/100000). Multivariable Cox proportional hazard model analysis showed that the maximum glucocorticoids dosage (adjusted HR [aHR]=2.43, 95%CI 1.05-5.62, p=0.039 for 30-60mg/d equivalent prednisone; aHR=4.80, 95%CI 1.49-15.44, p=0.008 for >60mg/d equivalent prednisone) and TB contact (aHR=7.25, 95%CI 2.14-24.54, p=0.001) were independent risk factors for ATB.
Conclusion: Patients with RD complicated with TB infection had a higher risk of developing ATB. The use of medium to high dosage of glucocorticoids and the history of TB exposure might be independent risk factors for developing ATB, in which case TB preventive treatment should be considered.
†: Lifan Zhang and Yuchen Liu contributed equally to this work.
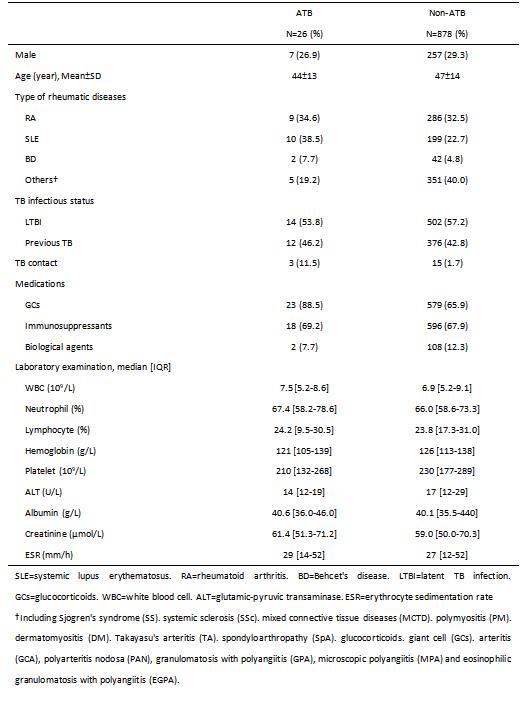 Table 1. General characteristics of 904 enrolled patients with rheumatic diseases complicated with TB infection
Table 1. General characteristics of 904 enrolled patients with rheumatic diseases complicated with TB infection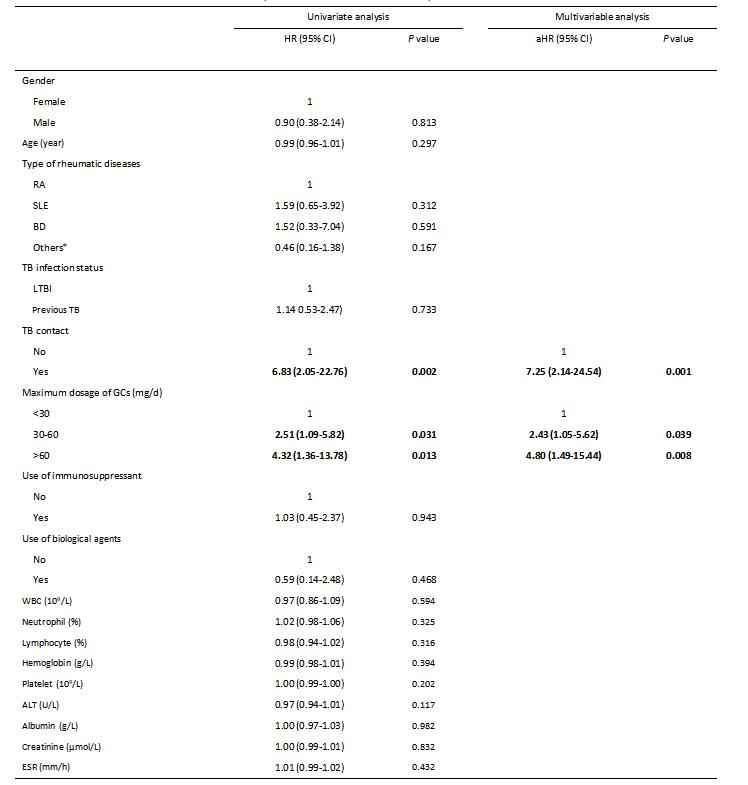 Table 2. Potential risk factors of the incidence of ATB in patients with rheumatic diseases complicated with TB infection
Table 2. Potential risk factors of the incidence of ATB in patients with rheumatic diseases complicated with TB infectionSLE=systemic lupus erythematosus. RA=rheumatoid arthritis. BD=Behcet's disease. LTBI=latent TB infection. GCs=glucocorticoids. WBC=white blood cell. ALT=glutamic-pyruvic transaminase. ESR=erythrocyte sedimentation rate
*Including Sjogren's syndrome (SS), systemic sclerosis (SSc), mixed connective tissue disease (MCTD), polymyositis (PM), dermatomyositis (DM), Takayasu arthritis (TA), giant cell arthritis (GCA), polyarteritis nodosa (PAN), granulomatosis with polyangiitis (GPA), microscopic polyarteritis (MPA), eosinophilic granulomatosis with polyangiitis (EGPA), ankylosing spondylitis (AS) and psoriatic arthritis (PsA)
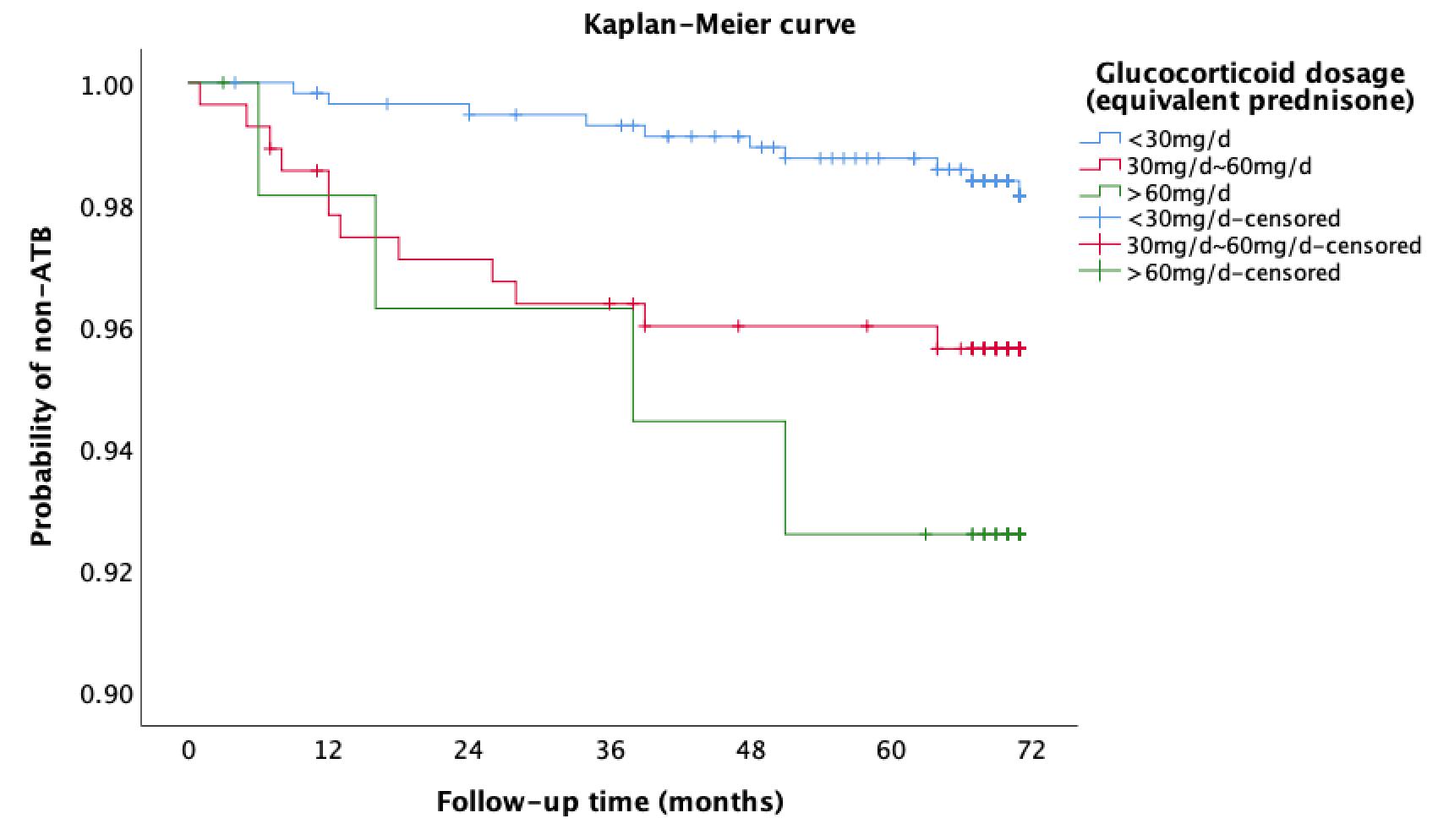 Figure 1. Incidence of ATB in patients with rheumatic diseases complicated with TB infection according to maximum daily dosage of GCs
Figure 1. Incidence of ATB in patients with rheumatic diseases complicated with TB infection according to maximum daily dosage of GCsDisclosures: L. Zhang, None; y. liu, None; x. zou, None; s. chen, None; y. ma, None; h. ma, None; q. cao, None; z. yang, None; F. ZHANG, None; Y. Zhao, None; X. Zeng, None; X. Liu, None.

