Back
Poster Session B
Reproductive health
Session: (0939–0969) Reproductive Issues in Rheumatic Disorders Poster
0967: Patterns of Breastfeeding Among Women with and Without Systemic Lupus Erythematosus
Sunday, November 13, 2022
9:00 AM – 10:30 AM Eastern Time
Location: Virtual Poster Hall
- LW
Laurel Wolf, MD
Medical University of South Carolina
Charleston, SC, United States
Abstract Poster Presenter(s)
Laurel Wolf, Erin Hynd, stephanie Bray, Dulaney Wilson, Jim Oates and Diane Kamen, Medical University of South Carolina, Charleston, SC
Background/Purpose: Benefits of breastfeeding for maternal and infant health outcomes are well-known. However, many barriers to initiating and maintaining breastfeeding have been identified, particularly for women with systemic lupus erythematosus (SLE). Studies of breastfeeding in SLE are limited. Our goal is to test the hypothesis that women with SLE have lower rates of breastfeeding than the general population and identify factors associated with breastfeeding.
Methods: Data for this nested case-control study was obtained from an ongoing IRB-approved longitudinal registry of patients with SLE and non-SLE controls. Information on demographics, breastfeeding, and medical, social, and obstetric history was obtained. Males and women without reported pregnancy were excluded. Pearson's chi-squared testing was performed for categorical variables and two-sample t-tests were performed for continuous variables. Multivariate logistic regression was performed.
Results: Study population included 439 patients with SLE and 264 non-SLE controls (116 unrelated controls) with at least one reported pregnancy. There were 813 deliveries among patients and 609 among controls (249 unrelated controls). There was a higher proportion of non-Black women and a lower rate of employment in the SLE group compared to controls (Table 1). Patients with SLE were older at their first pregnancy, had fewer pregnancies, and fewer live births (Table 1). Rates of breastfeeding increased with increasing age quartiles from < 20 to >29 years old (p< 0.01). Breastfeeding initiation rates did not differ in SLE cases (25.2%) compared to all controls (30.5%) but were significantly lower compared to unrelated controls (32.9%) (Table 1). Of those who breastfed, duration was not significantly different between patients with SLE and controls. The odds of breastfeeding were significantly higher in related (OR=1.51; 95% CI 1.07-2.13) and unrelated (OR=1.96; 95% CI=1.38-2.78) controls after adjustment for Black race, education, and year of pregnancy. Black women of all groups were less likely to initiate breastfeeding after adjustment for case/control status, education, and year of pregnancy (OR=0.50; 95% CI=0.33-0.77). Similarly, when the analysis was limited to SLE patients, Black women were less likely to initiate breastfeeding compared to non-Black women (23.7% vs 30.3%, p=0.02; OR=0.61; 9%% CI=0.40-0.96) after adjustment for year of pregnancy, education, and employment status.
Conclusion: Breastfeeding initiation rates were low among patients with SLE as well as controls compared to national averages over the same time period. Patients with SLE were less likely to initiate breastfeeding than controls, and Black patients were less likely to breastfeed than non-Black patients. These findings emphasize the need to continue to investigate modifiable barriers to breastfeeding, particularly among Black women with SLE.
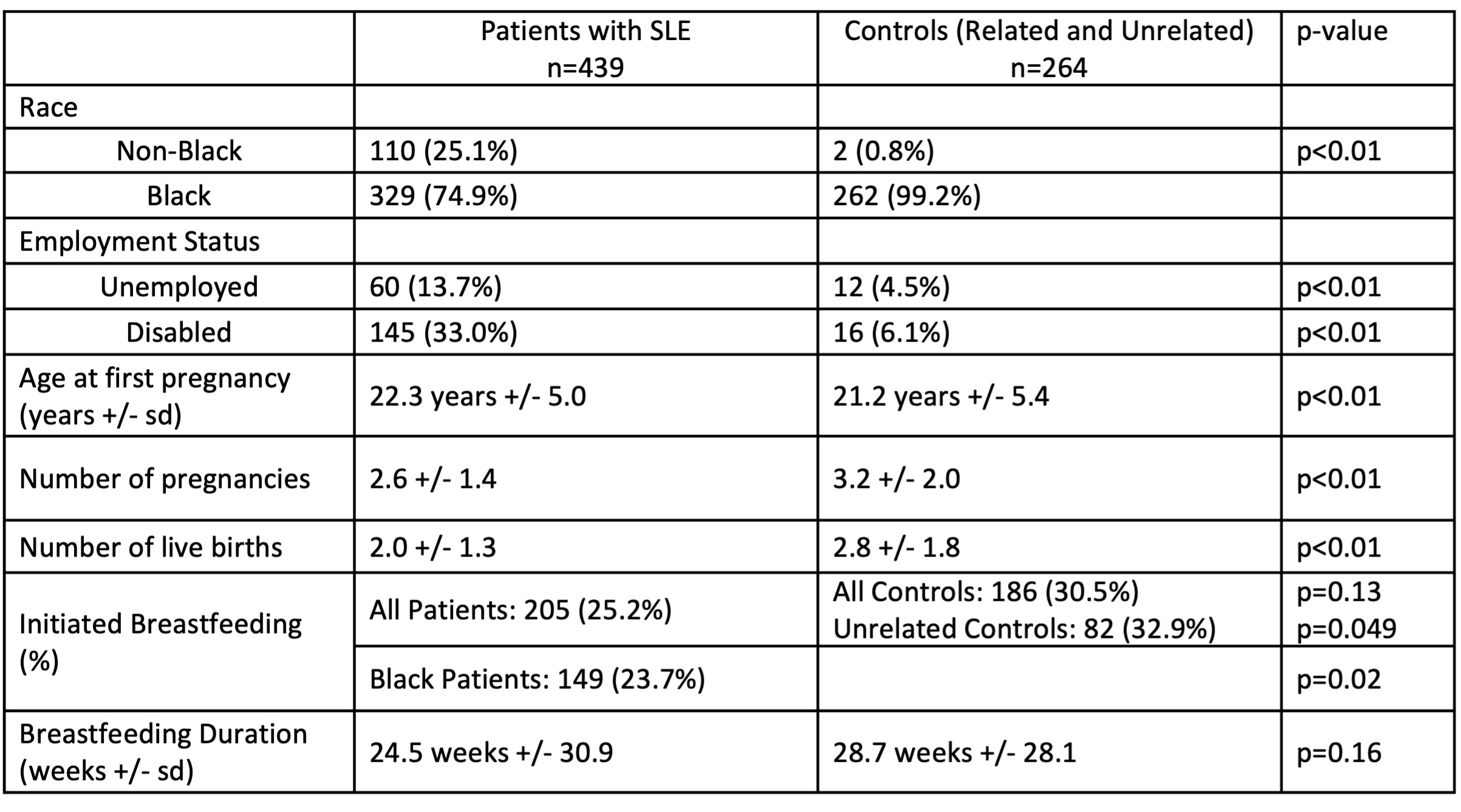 Table 1: Demographics, Pregnancy, and Breastfeeding Characteristics
Table 1: Demographics, Pregnancy, and Breastfeeding Characteristics
Disclosures: L. Wolf, None; E. Hynd, None; s. Bray, None; D. Wilson, None; J. Oates, None; D. Kamen, None.
Background/Purpose: Benefits of breastfeeding for maternal and infant health outcomes are well-known. However, many barriers to initiating and maintaining breastfeeding have been identified, particularly for women with systemic lupus erythematosus (SLE). Studies of breastfeeding in SLE are limited. Our goal is to test the hypothesis that women with SLE have lower rates of breastfeeding than the general population and identify factors associated with breastfeeding.
Methods: Data for this nested case-control study was obtained from an ongoing IRB-approved longitudinal registry of patients with SLE and non-SLE controls. Information on demographics, breastfeeding, and medical, social, and obstetric history was obtained. Males and women without reported pregnancy were excluded. Pearson's chi-squared testing was performed for categorical variables and two-sample t-tests were performed for continuous variables. Multivariate logistic regression was performed.
Results: Study population included 439 patients with SLE and 264 non-SLE controls (116 unrelated controls) with at least one reported pregnancy. There were 813 deliveries among patients and 609 among controls (249 unrelated controls). There was a higher proportion of non-Black women and a lower rate of employment in the SLE group compared to controls (Table 1). Patients with SLE were older at their first pregnancy, had fewer pregnancies, and fewer live births (Table 1). Rates of breastfeeding increased with increasing age quartiles from < 20 to >29 years old (p< 0.01). Breastfeeding initiation rates did not differ in SLE cases (25.2%) compared to all controls (30.5%) but were significantly lower compared to unrelated controls (32.9%) (Table 1). Of those who breastfed, duration was not significantly different between patients with SLE and controls. The odds of breastfeeding were significantly higher in related (OR=1.51; 95% CI 1.07-2.13) and unrelated (OR=1.96; 95% CI=1.38-2.78) controls after adjustment for Black race, education, and year of pregnancy. Black women of all groups were less likely to initiate breastfeeding after adjustment for case/control status, education, and year of pregnancy (OR=0.50; 95% CI=0.33-0.77). Similarly, when the analysis was limited to SLE patients, Black women were less likely to initiate breastfeeding compared to non-Black women (23.7% vs 30.3%, p=0.02; OR=0.61; 9%% CI=0.40-0.96) after adjustment for year of pregnancy, education, and employment status.
Conclusion: Breastfeeding initiation rates were low among patients with SLE as well as controls compared to national averages over the same time period. Patients with SLE were less likely to initiate breastfeeding than controls, and Black patients were less likely to breastfeed than non-Black patients. These findings emphasize the need to continue to investigate modifiable barriers to breastfeeding, particularly among Black women with SLE.
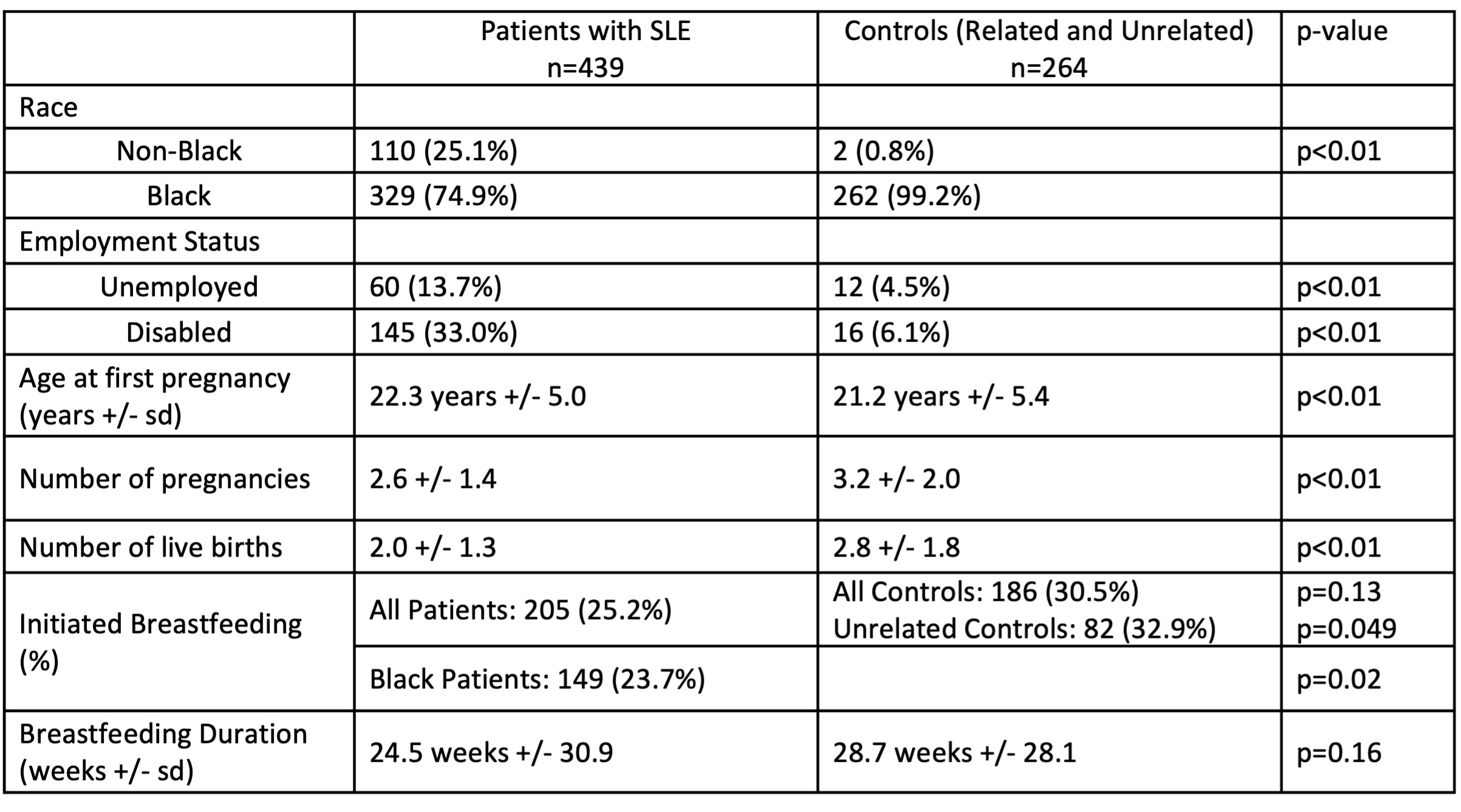 Table 1: Demographics, Pregnancy, and Breastfeeding Characteristics
Table 1: Demographics, Pregnancy, and Breastfeeding CharacteristicsDisclosures: L. Wolf, None; E. Hynd, None; s. Bray, None; D. Wilson, None; J. Oates, None; D. Kamen, None.

