Back
Poster Session B
Antiphospholipid Syndrome
Session: (0671–0694) Antiphospholipid Syndrome Poster
0676: Presentation and Outcomes in Patients with Adrenal Hemorrhage Associated with Antiphospholipid Syndrome: A Cohort Study and Systematic Review of Literature
Sunday, November 13, 2022
9:00 AM – 10:30 AM Eastern Time
Location: Virtual Poster Hall
- JM
Jose Meade-Aguilar, MD
Mayo Clinic
Rochester, MN, United States
Abstract Poster Presenter(s)
Jose A Meade-Aguilar1, Gabriel Figueroa Parra1, Jeffrey X. Yang1, Hannah Langenfeld2, Prerna Dogra1, Irina Bancos3, Hassan Murad3, Cynthia Crowson4 and Ali Duarte-Garcia1, 1Mayo Clinic, Rochester, MN, 2Department of Quantitative Health Sciences, Mayo Clinic, Rochester, MN, 3Mayo Clinic, Rochester, 4Mayo Clinic, Eyota, MN
Background/Purpose: To describe the clinical characteristics, therapies, and outcomes of patients with antiphospholipid syndrome (APS) and adrenal hemorrhage (AH).
Methods: We performed a multicenter retrospective cohort study identifying patients with APS and AH, up to December 12, 2021. We included patients with APS meeting the Sydney criteria and an episode of AH, defined as the presence of imaging consistent with AH or a biopsy revealing hemorrhagic infarction of the adrenal glands.
A Systematic Review of the Literature (SLR) was performed according to the PRISMA guidelines. We did a comprehensive search in multiple databases from their inception to October 20, 2021, in any language. Two reviewers independently screened and reviewed the articles and extracted information. We included case reports/case series reporting cases that met the inclusion criteria used for the cohort. Extracted data included demographics and clinical characteristics at presentation, laboratory data, radiologic findings, therapeutic strategies, and clinical outcomes. Descriptive statistics were used to summarize data. Survival analysis (Kaplan-Meier and Cox models) were used on the cohort only to evaluate factors associated with mortality and radiological remission.
Results: 240 patients were included, 59 (25%) from the cohort and 181 (75%) from the SLR. The mean age was 46.8 (14.96) years, and 44% were female. The median time of APS duration before AH was 3.8 years, and the median follow-up was 10.8 months. History of venous thrombosis was present in 65%, a prior stroke in 12%, and obstetric morbidity in 24%. The most common non-thrombotic APS manifestation was thrombocytopenia (46%), and 21% of the patients had SLE. 80% of the patients had a positive LA, 76% anticardiolipin (aCL) IgG, 46% aCL IgM, 57% anti-β2 glycoprotein-I (β2GPI) IgG, and 36% β2GPI IgM. At presentation, 46% of patients had nausea/vomiting, 80% abdominal pain, and 31% hypotension (Table 1). 83% had a CT scan imaging consistent with acute adrenal hematoma, and 69% of these were bilateral. Adrenal insufficiency was present in 63%, and 47% received hydrocortisone as hormonal substitutive therapy. 58% were receiving anticoagulation before AH and 73% received anticoagulation as treatment. Analysis derived from the cohort showed that radiological remission was documented in 6.6% at 1-year and 41.4% at 5-year follow-ups (Figure 1A). Radiological remission was less likely among those with thrombocytopenia (HR: 0.35) (Figure 2). Death was reported in 27% of patients, with a rate of 1.7% at 1-year and 11.3% at 5-years (Figure 1B). Positive β2GPI IgG and IgM were significantly associated with mortality (HR: 2.66 and 3.32, respectively).
Conclusion: AH is a rare manifestation of APS; the majority of the patients have bilateral adrenal gland involvement. Most patients will develop adrenal insufficiency. Thrombocytopenia is associated with AH and persistent hemorrhage in imaging. Positivity to β2GPI was associated with mortality.
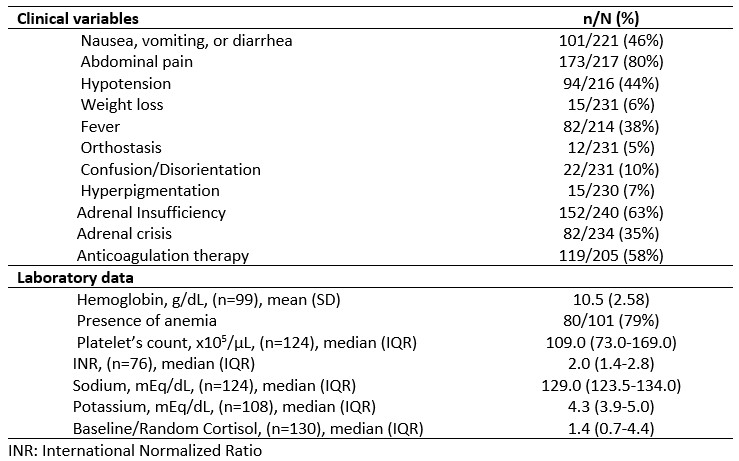 Table 1. Clinical manifestations and laboratory data of the cohort and systematic review, at presentation of patients with adrenal hemorrhage and antiphospholipid syndrome.
Table 1. Clinical manifestations and laboratory data of the cohort and systematic review, at presentation of patients with adrenal hemorrhage and antiphospholipid syndrome.
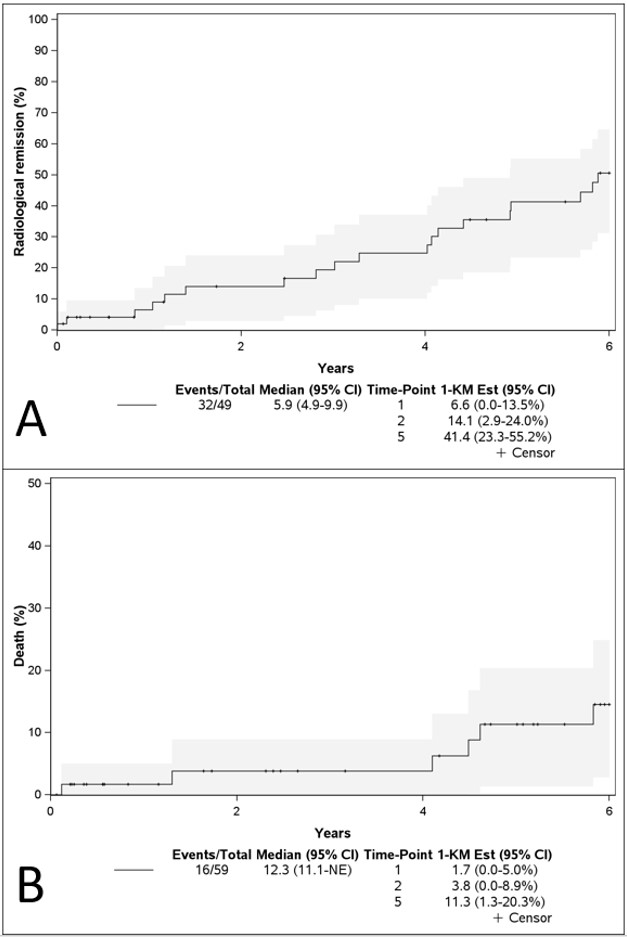 Figure 1. Cumulative incidence of (A) radiological remission and (B) mortality in patients in patients from the cohort with adrenal hemorrhage and antiphospholipid syndrome.
Figure 1. Cumulative incidence of (A) radiological remission and (B) mortality in patients in patients from the cohort with adrenal hemorrhage and antiphospholipid syndrome.
.jpg) Figure 2. Hazard Ratios (95% IC) adjusted for sex and age of variables associated with radiological remission and mortality in patients with incident adrenal hemorrhage and antiphospholipid syndrome.
Figure 2. Hazard Ratios (95% IC) adjusted for sex and age of variables associated with radiological remission and mortality in patients with incident adrenal hemorrhage and antiphospholipid syndrome.
Disclosures: J. Meade-Aguilar, None; G. Figueroa Parra, None; J. Yang, None; H. Langenfeld, None; P. Dogra, None; I. Bancos, hra pharma, corcept, recordati, spruce, sparrow, lantheus, adrenas; H. Murad, None; C. Crowson, None; A. Duarte-Garcia, None.
Background/Purpose: To describe the clinical characteristics, therapies, and outcomes of patients with antiphospholipid syndrome (APS) and adrenal hemorrhage (AH).
Methods: We performed a multicenter retrospective cohort study identifying patients with APS and AH, up to December 12, 2021. We included patients with APS meeting the Sydney criteria and an episode of AH, defined as the presence of imaging consistent with AH or a biopsy revealing hemorrhagic infarction of the adrenal glands.
A Systematic Review of the Literature (SLR) was performed according to the PRISMA guidelines. We did a comprehensive search in multiple databases from their inception to October 20, 2021, in any language. Two reviewers independently screened and reviewed the articles and extracted information. We included case reports/case series reporting cases that met the inclusion criteria used for the cohort. Extracted data included demographics and clinical characteristics at presentation, laboratory data, radiologic findings, therapeutic strategies, and clinical outcomes. Descriptive statistics were used to summarize data. Survival analysis (Kaplan-Meier and Cox models) were used on the cohort only to evaluate factors associated with mortality and radiological remission.
Results: 240 patients were included, 59 (25%) from the cohort and 181 (75%) from the SLR. The mean age was 46.8 (14.96) years, and 44% were female. The median time of APS duration before AH was 3.8 years, and the median follow-up was 10.8 months. History of venous thrombosis was present in 65%, a prior stroke in 12%, and obstetric morbidity in 24%. The most common non-thrombotic APS manifestation was thrombocytopenia (46%), and 21% of the patients had SLE. 80% of the patients had a positive LA, 76% anticardiolipin (aCL) IgG, 46% aCL IgM, 57% anti-β2 glycoprotein-I (β2GPI) IgG, and 36% β2GPI IgM. At presentation, 46% of patients had nausea/vomiting, 80% abdominal pain, and 31% hypotension (Table 1). 83% had a CT scan imaging consistent with acute adrenal hematoma, and 69% of these were bilateral. Adrenal insufficiency was present in 63%, and 47% received hydrocortisone as hormonal substitutive therapy. 58% were receiving anticoagulation before AH and 73% received anticoagulation as treatment. Analysis derived from the cohort showed that radiological remission was documented in 6.6% at 1-year and 41.4% at 5-year follow-ups (Figure 1A). Radiological remission was less likely among those with thrombocytopenia (HR: 0.35) (Figure 2). Death was reported in 27% of patients, with a rate of 1.7% at 1-year and 11.3% at 5-years (Figure 1B). Positive β2GPI IgG and IgM were significantly associated with mortality (HR: 2.66 and 3.32, respectively).
Conclusion: AH is a rare manifestation of APS; the majority of the patients have bilateral adrenal gland involvement. Most patients will develop adrenal insufficiency. Thrombocytopenia is associated with AH and persistent hemorrhage in imaging. Positivity to β2GPI was associated with mortality.
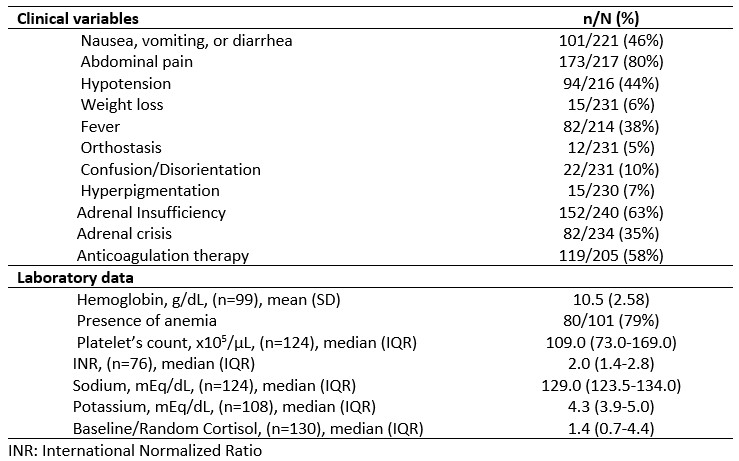 Table 1. Clinical manifestations and laboratory data of the cohort and systematic review, at presentation of patients with adrenal hemorrhage and antiphospholipid syndrome.
Table 1. Clinical manifestations and laboratory data of the cohort and systematic review, at presentation of patients with adrenal hemorrhage and antiphospholipid syndrome.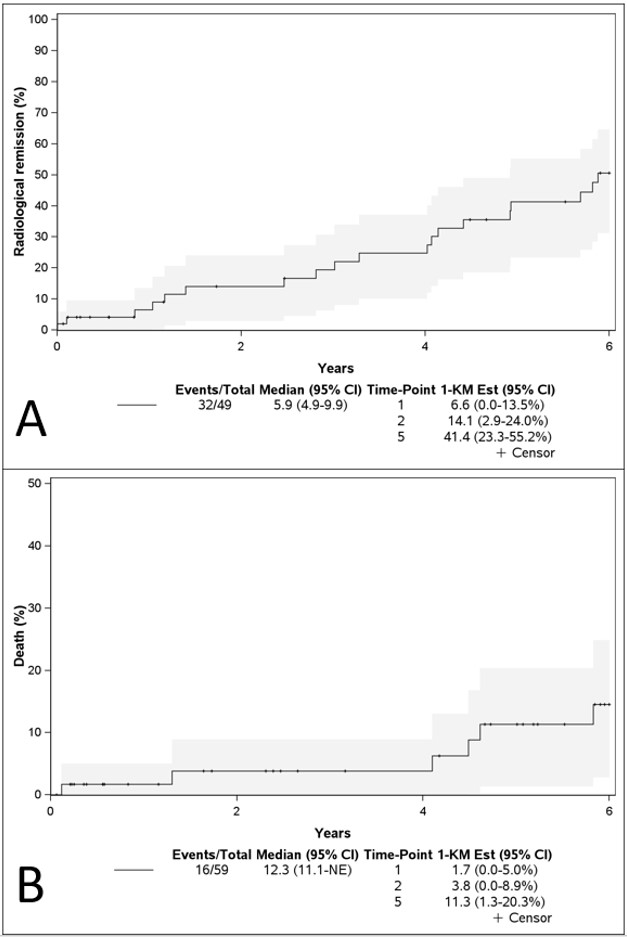 Figure 1. Cumulative incidence of (A) radiological remission and (B) mortality in patients in patients from the cohort with adrenal hemorrhage and antiphospholipid syndrome.
Figure 1. Cumulative incidence of (A) radiological remission and (B) mortality in patients in patients from the cohort with adrenal hemorrhage and antiphospholipid syndrome..jpg) Figure 2. Hazard Ratios (95% IC) adjusted for sex and age of variables associated with radiological remission and mortality in patients with incident adrenal hemorrhage and antiphospholipid syndrome.
Figure 2. Hazard Ratios (95% IC) adjusted for sex and age of variables associated with radiological remission and mortality in patients with incident adrenal hemorrhage and antiphospholipid syndrome. Disclosures: J. Meade-Aguilar, None; G. Figueroa Parra, None; J. Yang, None; H. Langenfeld, None; P. Dogra, None; I. Bancos, hra pharma, corcept, recordati, spruce, sparrow, lantheus, adrenas; H. Murad, None; C. Crowson, None; A. Duarte-Garcia, None.

