Back
Poster Session B
Fibrosing rheumatic diseases (scleroderma, MCTD, IgG4-related disease, scleroderma mimics)
Session: (1046–1070) Systemic Sclerosis and Related Disorders – Clinical Poster I
1069: Renal Involvement Other Than Renal Crisis in Systemic Sclerosis: A Retrospective Monocentric Cohort Study
Sunday, November 13, 2022
9:00 AM – 10:30 AM Eastern Time
Location: Virtual Poster Hall
- GB
Gaelle Becel, MD
APHP
Paris, France
Abstract Poster Presenter(s)
Gaelle Becel1, Bertrand Dunogue1, Benjamin Chaigne1, Benjamin Thoreau2, Alexis Regent1, Alexandre Karras3, Benjamin Terrier1 and Luc Mouthon1, 1National Referral Center for Rare Systemic Autoimmune Diseases, Cochin Hospital, Paris, France, 2AP-HP, Université Paris Cité, INSERM U1016, CNR UMR 8104, Paris, France, 3HEGP, Paris, France
Background/Purpose: Scleroderma renal crisis has extensively been described over the past decades because of its severity. The use of angiotensin-converting enzyme inhibitors has clearly improved its outcome. However, few data are available on chronic renal impairment in systemic sclerosis (SSc). The aim of this study is to describe the different types of renal involvement observed in SSc in order to establish their frequency and to identify potential predictive factors.
Methods: Clinical and biological data from patients with systemic sclerosis (SSc) cared for in our Internal Medicine Department between 01/01/1989 and 12/31/2020 were retrospectively analyzed. Diagnosis was based on the 2013 ACR/EULAR Classification Criteria for SSc. At least two measurements of serum creatinine during follow up assessments were required for inclusion in this study. Patients who presented a renal crisis, chronic renal failure (glomerular filtration rate CKD-EPI < 60 mL/min/1.73 m2) or proteinuria (at least one sample proteinuria value > 0.5 g/g among the available values) during their follow-up were identified.
Results: 649 patients including 106 males (16%) were included in this study; 6% of them developed a renal crisis, 13% a chronic renal failure and 11% a proteinuria. Chronic renal failure and proteinuria occurred without renal crisis in about 70% of cases.
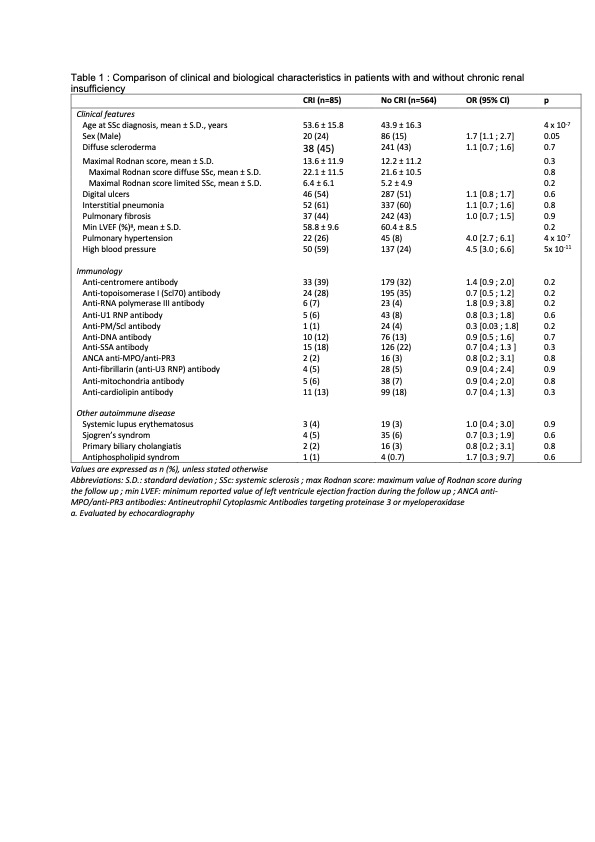
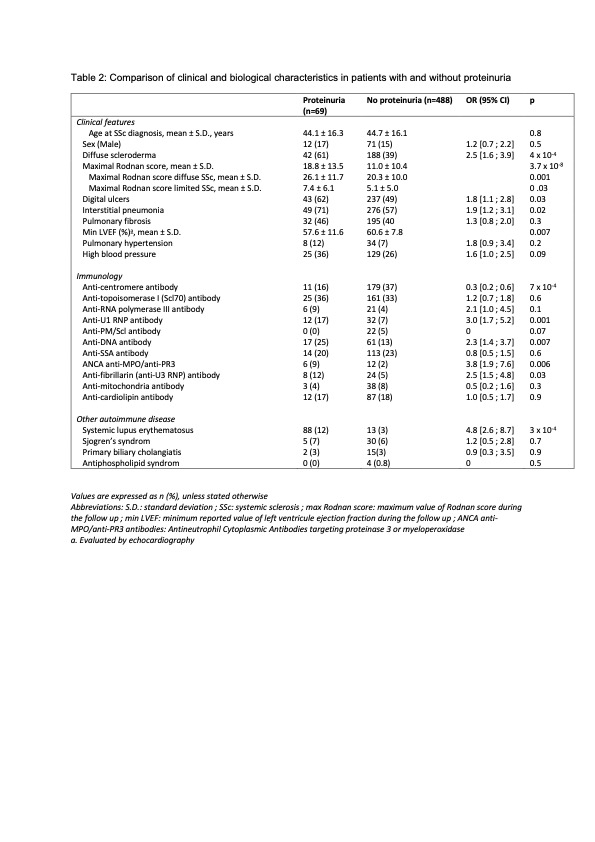
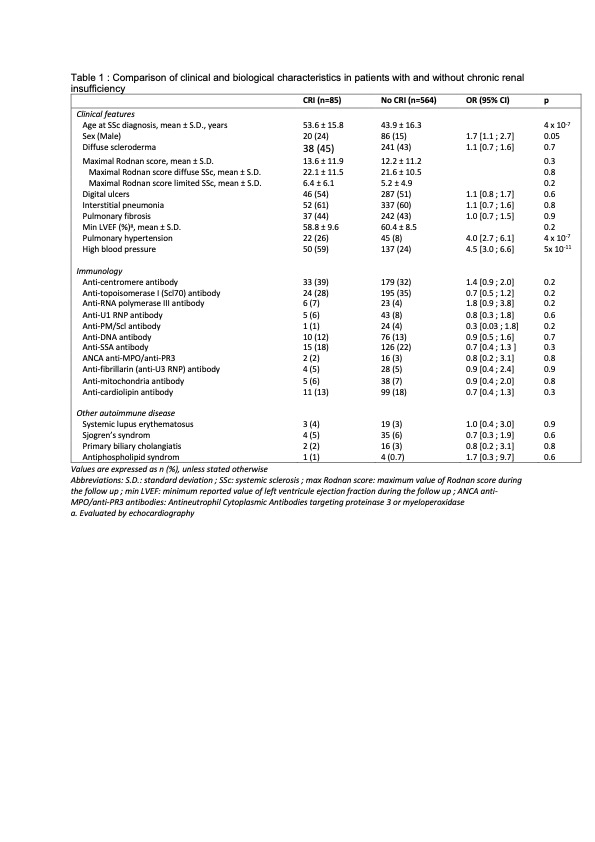
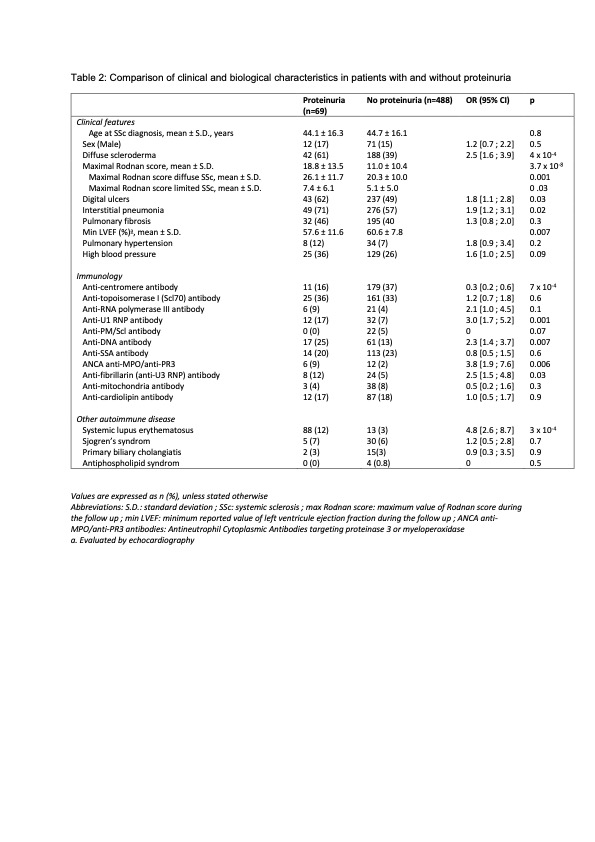
Chronic renal failure was significantly associated with age, high blood pressure (OR 4.5, 95% CI [3.0 ; 6.6], p < 0.05), pulmonary hypertension (OR 4.0, 95% CI [2.7 ; 6.1], p < 0.05) and digital ulcers (OR 1.8, 95% CI [1.1 ; 2.8], p < 0.05) (Table 1). Among patients with no history of renal crisis, chronic renal failure occurred more often in those with anti-centromere antibodies (OR 2.3, 95% CI [1.4 ; 3.8], p < 0.05). Proteinuria was significantly more frequent in patients with interstitial lung disease (OR 1.9, 95% CI [1.2 ; 3.1], p< 0.05) and diffuse SSc (OR 2.5, 95% CI [1.6 ; 3.9], p< 0.05), and in the presence of anti-DNA, ANCA anti-MPO or anti-PR3, anti-RNP and anti-fibrillarin antibodies (Table 2). The onset of proteinuria was also linked to the severity of skin involvement.
Conclusion: Chronic renal failure and proteinuria occur mostly in the absence of a scleroderma renal crisis. Better knowledge and understanding of the underlying mechanisms of renal disease in SSc should allow for improved screening and treatment.
Disclosures: G. Becel, None; B. Dunogue, None; B. Chaigne, None; B. Thoreau, None; A. Regent, None; A. Karras, Roche, Gilead, Amgen; B. Terrier, AstraZeneca, GlaxoSmithKline, Bristol-Myers Squibb(BMS), Eli Lilly, LFB, Boehinger Ingelheim, Vifor Pharma, Pfizer, Roche; L. Mouthon, Boehringer-Ingelheim, LFB.
Background/Purpose: Scleroderma renal crisis has extensively been described over the past decades because of its severity. The use of angiotensin-converting enzyme inhibitors has clearly improved its outcome. However, few data are available on chronic renal impairment in systemic sclerosis (SSc). The aim of this study is to describe the different types of renal involvement observed in SSc in order to establish their frequency and to identify potential predictive factors.
Methods: Clinical and biological data from patients with systemic sclerosis (SSc) cared for in our Internal Medicine Department between 01/01/1989 and 12/31/2020 were retrospectively analyzed. Diagnosis was based on the 2013 ACR/EULAR Classification Criteria for SSc. At least two measurements of serum creatinine during follow up assessments were required for inclusion in this study. Patients who presented a renal crisis, chronic renal failure (glomerular filtration rate CKD-EPI < 60 mL/min/1.73 m2) or proteinuria (at least one sample proteinuria value > 0.5 g/g among the available values) during their follow-up were identified.
Results: 649 patients including 106 males (16%) were included in this study; 6% of them developed a renal crisis, 13% a chronic renal failure and 11% a proteinuria. Chronic renal failure and proteinuria occurred without renal crisis in about 70% of cases.
Chronic renal failure was significantly associated with age, high blood pressure (OR 4.5, 95% CI [3.0 ; 6.6], p < 0.05), pulmonary hypertension (OR 4.0, 95% CI [2.7 ; 6.1], p < 0.05) and digital ulcers (OR 1.8, 95% CI [1.1 ; 2.8], p < 0.05) (Table 1). Among patients with no history of renal crisis, chronic renal failure occurred more often in those with anti-centromere antibodies (OR 2.3, 95% CI [1.4 ; 3.8], p < 0.05). Proteinuria was significantly more frequent in patients with interstitial lung disease (OR 1.9, 95% CI [1.2 ; 3.1], p< 0.05) and diffuse SSc (OR 2.5, 95% CI [1.6 ; 3.9], p< 0.05), and in the presence of anti-DNA, ANCA anti-MPO or anti-PR3, anti-RNP and anti-fibrillarin antibodies (Table 2). The onset of proteinuria was also linked to the severity of skin involvement.
Conclusion: Chronic renal failure and proteinuria occur mostly in the absence of a scleroderma renal crisis. Better knowledge and understanding of the underlying mechanisms of renal disease in SSc should allow for improved screening and treatment.
Disclosures: G. Becel, None; B. Dunogue, None; B. Chaigne, None; B. Thoreau, None; A. Regent, None; A. Karras, Roche, Gilead, Amgen; B. Terrier, AstraZeneca, GlaxoSmithKline, Bristol-Myers Squibb(BMS), Eli Lilly, LFB, Boehinger Ingelheim, Vifor Pharma, Pfizer, Roche; L. Mouthon, Boehringer-Ingelheim, LFB.

