Back
Poster Session B
Rheumatoid arthritis (RA)
Session: (0883–0912) RA – Diagnosis, Manifestations, and Outcomes Poster II
0891: Rheumatoid Arthritis and the Rheumatic Disease Comorbidity Index (RDCI): Its Impact on Disease Activity
Sunday, November 13, 2022
9:00 AM – 10:30 AM Eastern Time
Location: Virtual Poster Hall
- RA
Renad Ahmed, -None-
king abdulaziz university
Jeddah, Saudi Arabia
Abstract Poster Presenter(s)
Sultana Abdulaziz1, Suzan Attar2, Renad Ahmed2, Hamza Fida2, Omar Bokhary2, Anas Alyazidi2 and Abdulelah Abumohssin2, 1King Fahad Hospital, Jeddah, Saudi Arabia, 2King Abdulaziz University, Jeddah, Saudi Arabia
Background/Purpose: Comorbid conditions in the setting of rheumatoid arthritis (RA) play an important role in predicting disease activity and functional impairment (1). Application of a specific comorbidity index in a clinical setting could be useful in identifying patients with a poor prognosis (2). The rheumatic disease comorbidity index (RDCI) is a scoring system developed specifically for RA patients that is used to assess their total burden of comorbidity (2). The application of RDCI has not yet been well documented in published literature, and the clinical presentations and comorbidities of RA patients have not been adequately described in the local region. Our study aims to assess the relationship between comorbidity and disease activity of RA by use of the RDCI.
Methods: Between 2019 and 2021, medical records and clinical data from the latest rheumatology clinic visit of consecutive RA outpatients above 18 years of age were reviewed in a two-center retrospective study. Data retrieved included demographics, clinical presentation, inflammatory markers, comorbid conditions, and medications. RDCI was calculated for each patient, and disease activity was assessed using disease activity score 28 (DAS28), clinical Disease Activity Index (CDAI) and Simplified Disease Activity Index (SDAI) scores. The degree of functional impairment was documented using the health assessment questionnaire (HAQ).
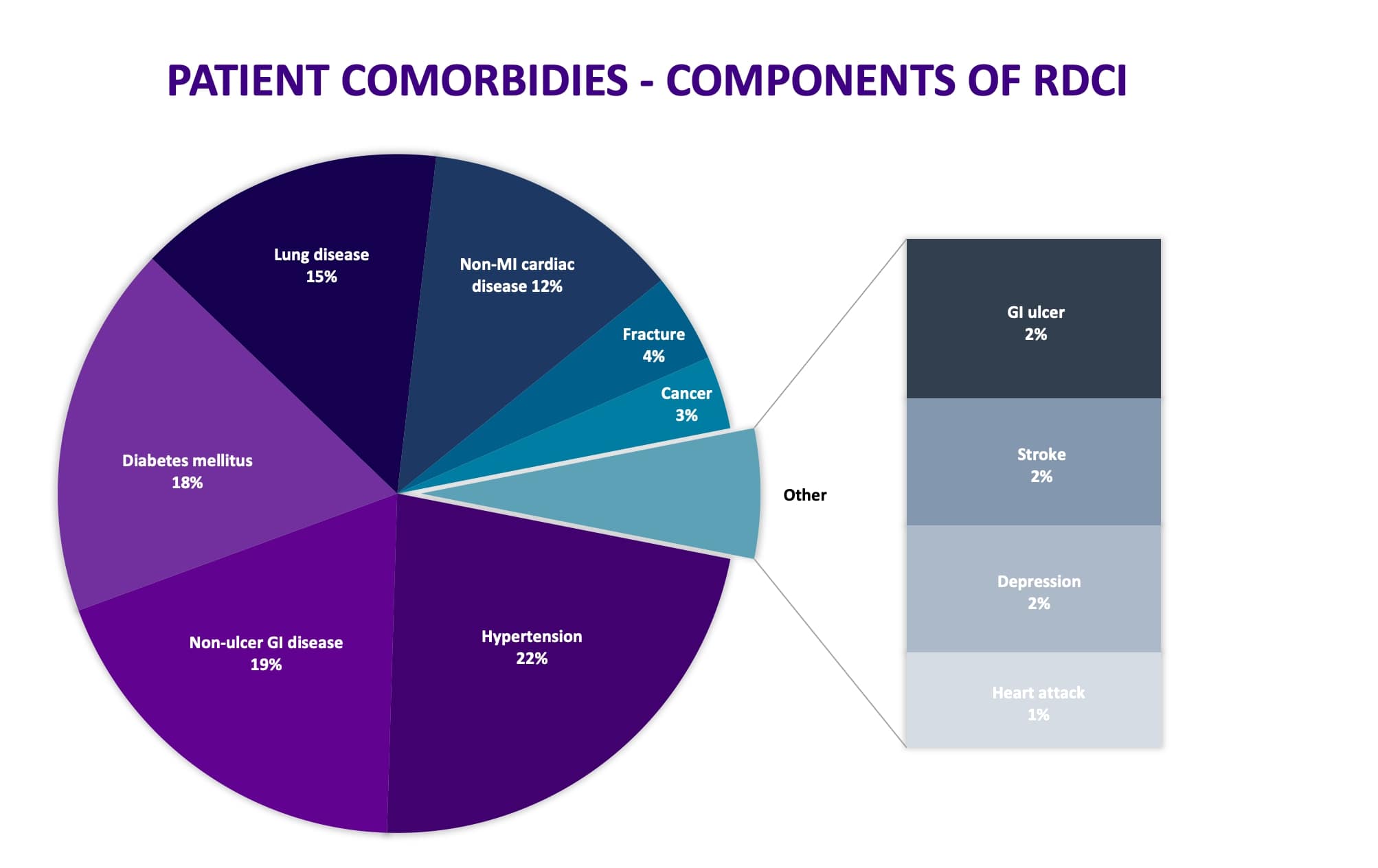
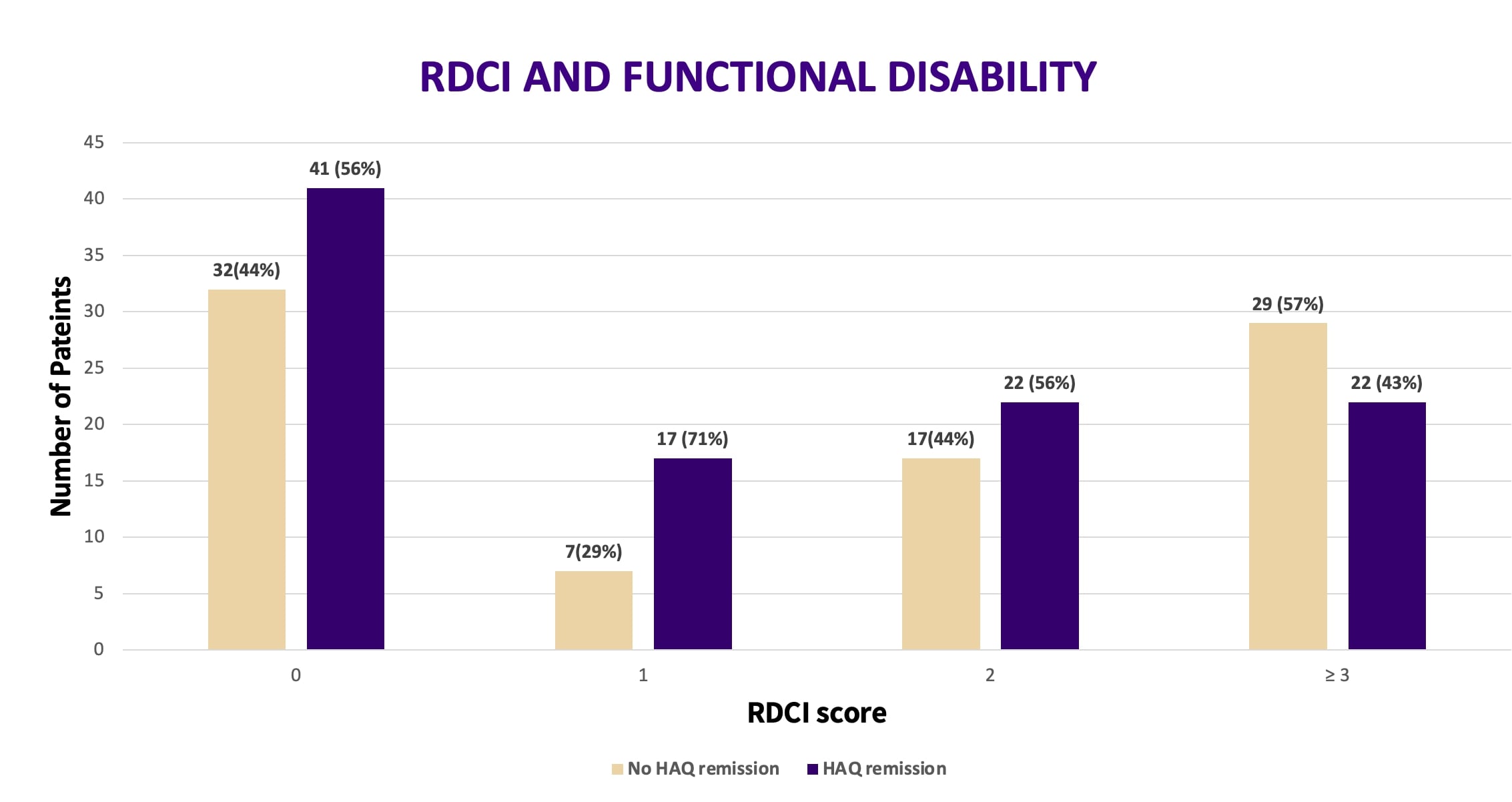
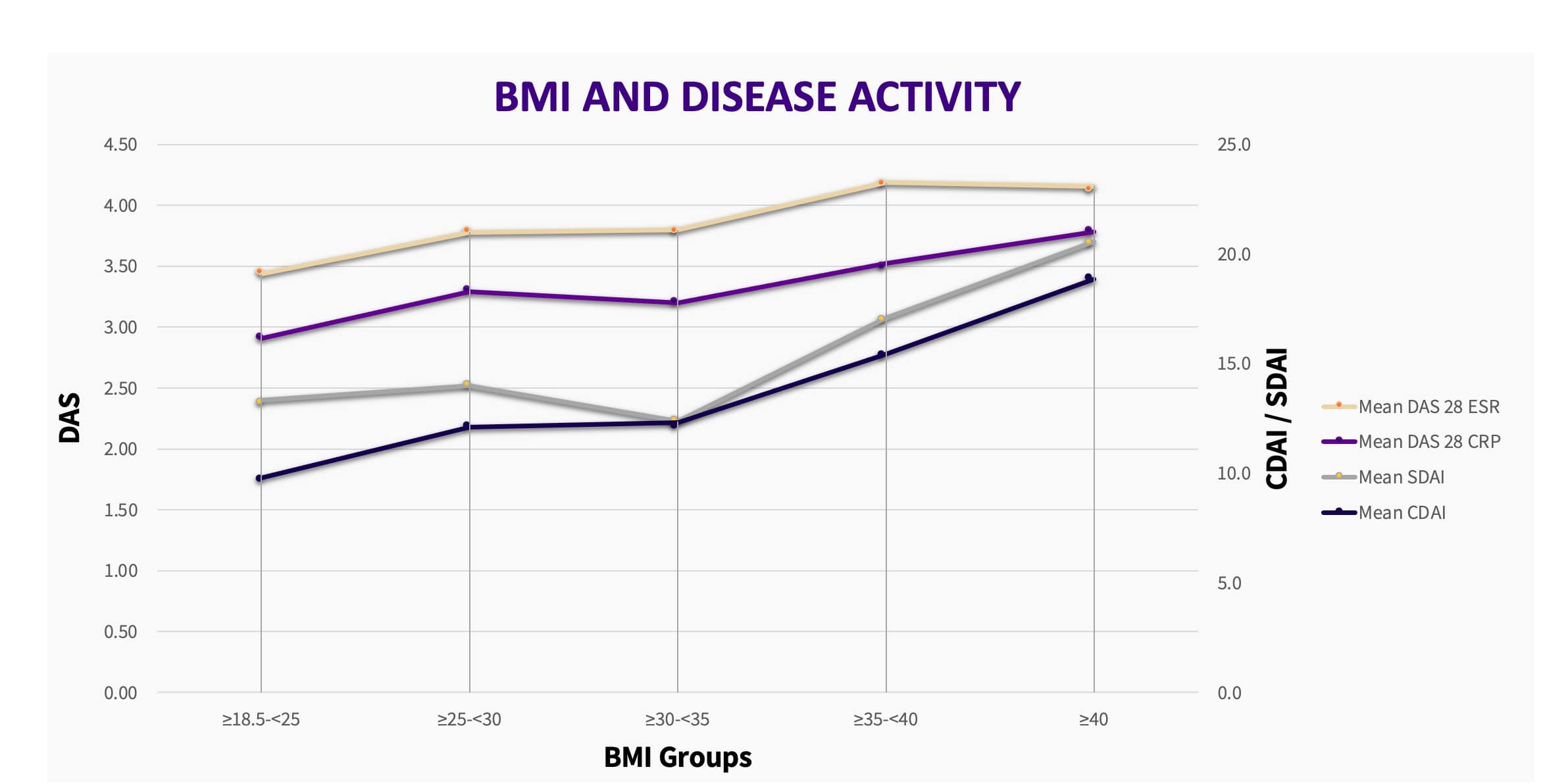
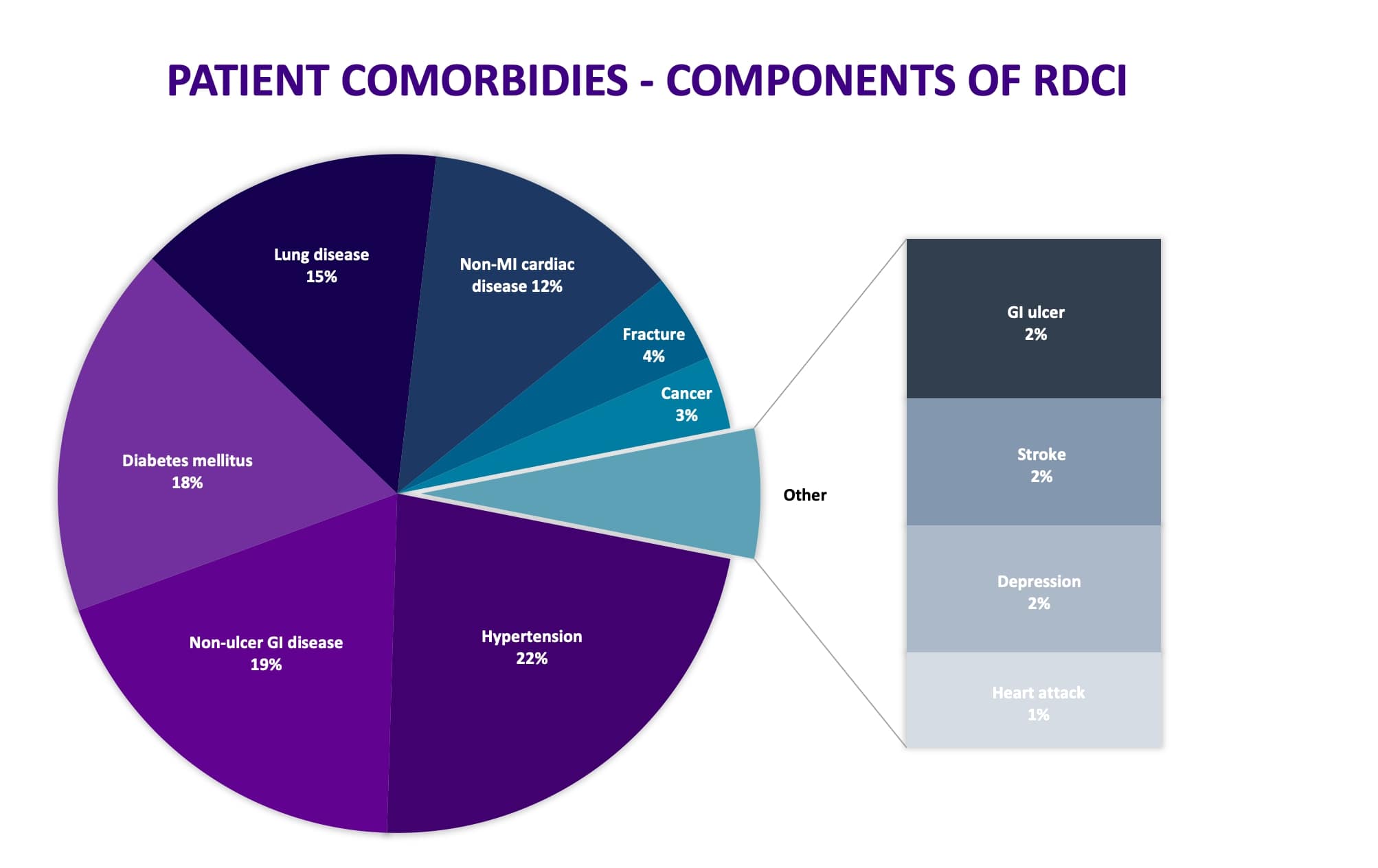
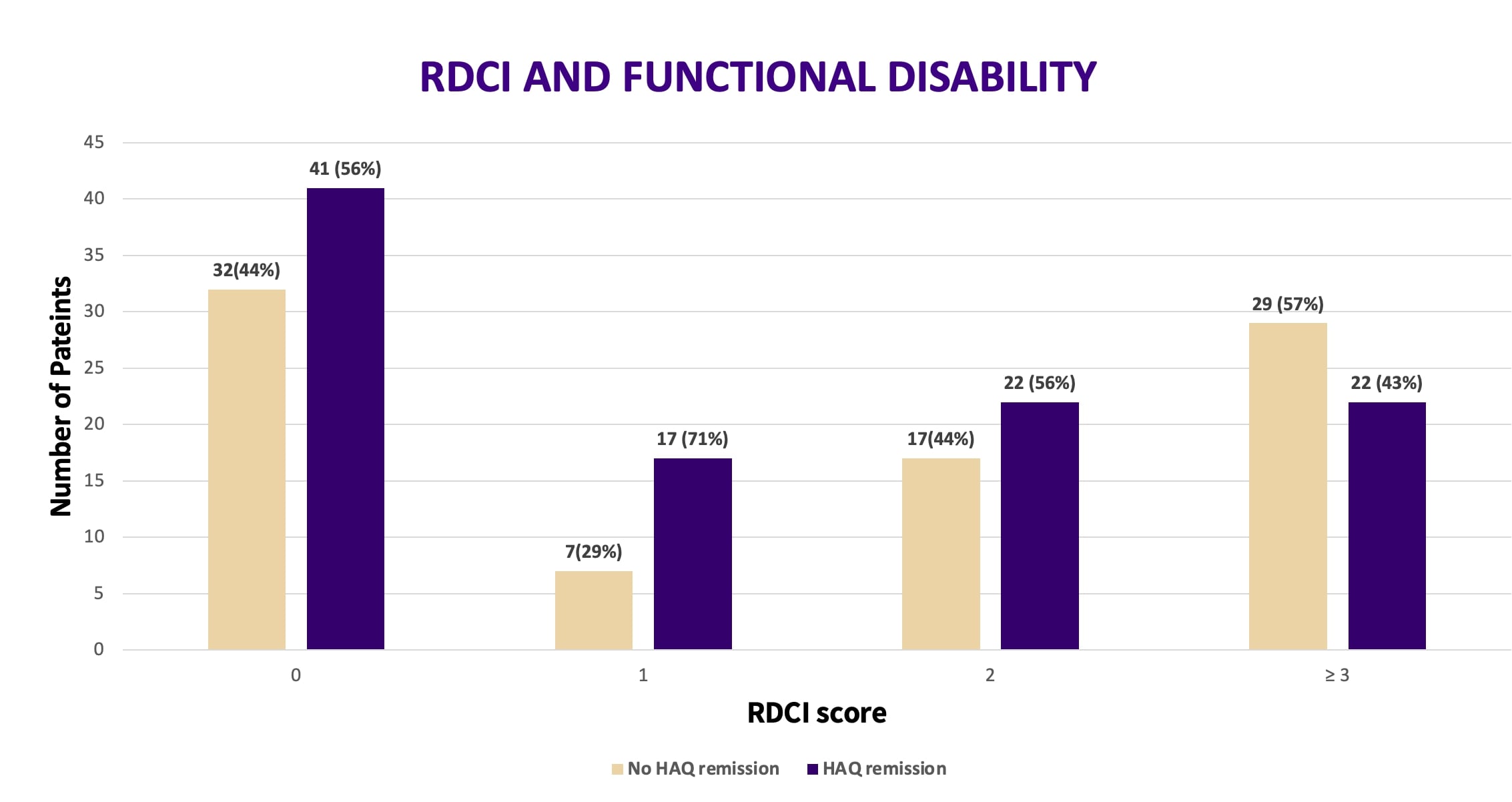
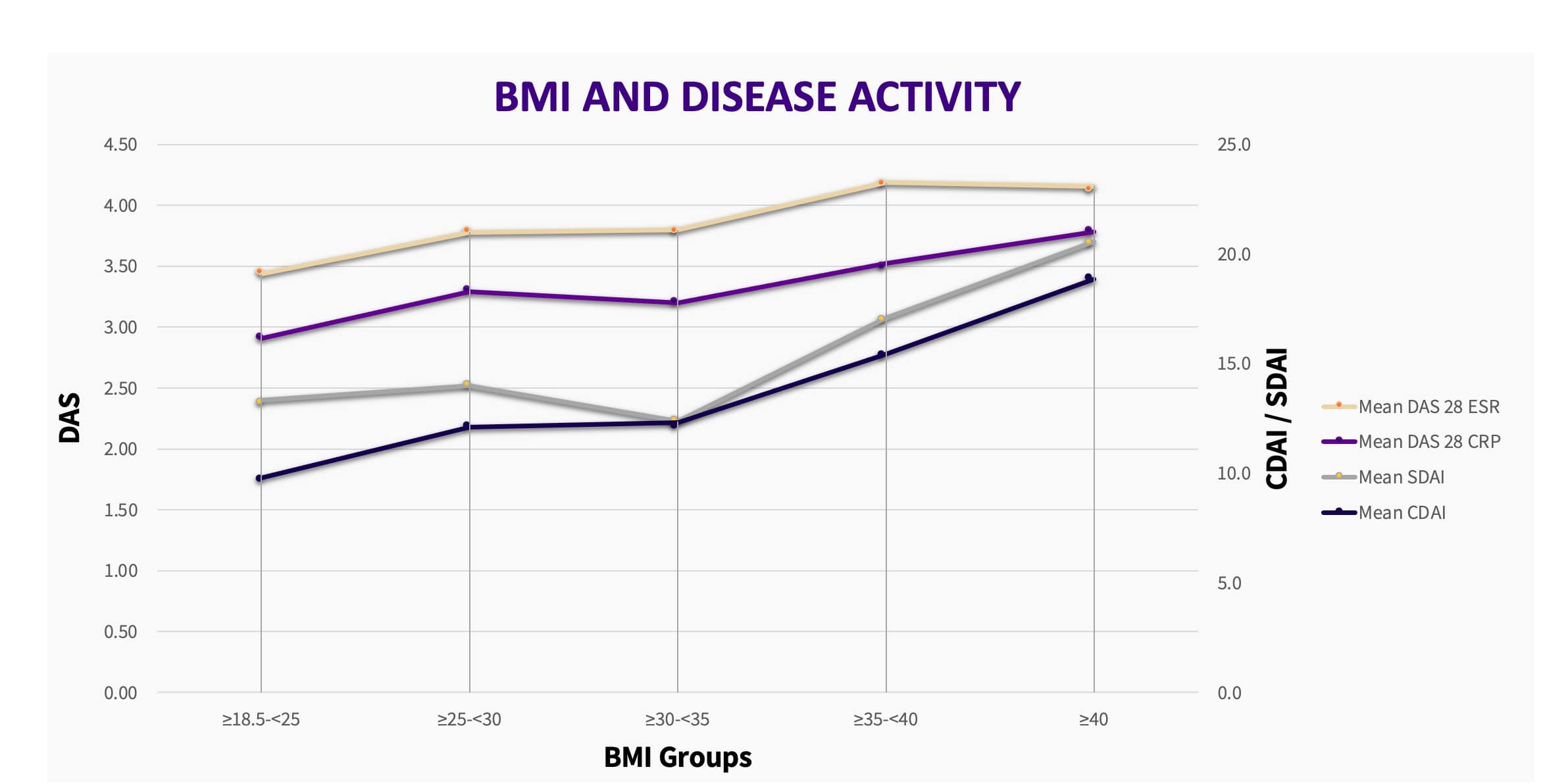
Results: 195 patients were included in this study. Most of the study population was female, with a mean age of 55 years, and an average body mass index (BMI) of 31. The most prevalent comorbidity was hypertension (29.7%). A large portion of patients had an RDCI score of zero (38.5%) with the second largest group scoring 3 or higher (22.1%). The mean DAS 28 CRP score was 3.34 (± 1.2), with 49.3% of patients achieving a good EULAR response, while the mean CDAI score was 13.8 ± 10.3 with only 19 (9.9%) patients achieving the same response. Patients with a higher RDCI score were older (p < 0.001) with a longer duration of disease (p < 0.001) and significantly higher HAQ scores (p = 0.012). However, no association between RDCI scores and disease activity was found. Independent predictors of a good clinical response were decreasing BMI and the use of tumor necrosis factor-inhibiting medications.
Conclusion: Although a direct relationship between RDCI score and disease activity could not be established, it did have a significant impact on functional impairment. We recommend that routine calculation of RDCI scores could prove useful in identifying multimorbid RA patients with a poor prognosis and help in fine adjustment of treatment goals to restore quality of life.
Disclosures: S. Abdulaziz, None; S. Attar, None; R. Ahmed, None; H. Fida, None; O. Bokhary, None; A. Alyazidi, None; A. Abumohssin, None.
Background/Purpose: Comorbid conditions in the setting of rheumatoid arthritis (RA) play an important role in predicting disease activity and functional impairment (1). Application of a specific comorbidity index in a clinical setting could be useful in identifying patients with a poor prognosis (2). The rheumatic disease comorbidity index (RDCI) is a scoring system developed specifically for RA patients that is used to assess their total burden of comorbidity (2). The application of RDCI has not yet been well documented in published literature, and the clinical presentations and comorbidities of RA patients have not been adequately described in the local region. Our study aims to assess the relationship between comorbidity and disease activity of RA by use of the RDCI.
Methods: Between 2019 and 2021, medical records and clinical data from the latest rheumatology clinic visit of consecutive RA outpatients above 18 years of age were reviewed in a two-center retrospective study. Data retrieved included demographics, clinical presentation, inflammatory markers, comorbid conditions, and medications. RDCI was calculated for each patient, and disease activity was assessed using disease activity score 28 (DAS28), clinical Disease Activity Index (CDAI) and Simplified Disease Activity Index (SDAI) scores. The degree of functional impairment was documented using the health assessment questionnaire (HAQ).
Results: 195 patients were included in this study. Most of the study population was female, with a mean age of 55 years, and an average body mass index (BMI) of 31. The most prevalent comorbidity was hypertension (29.7%). A large portion of patients had an RDCI score of zero (38.5%) with the second largest group scoring 3 or higher (22.1%). The mean DAS 28 CRP score was 3.34 (± 1.2), with 49.3% of patients achieving a good EULAR response, while the mean CDAI score was 13.8 ± 10.3 with only 19 (9.9%) patients achieving the same response. Patients with a higher RDCI score were older (p < 0.001) with a longer duration of disease (p < 0.001) and significantly higher HAQ scores (p = 0.012). However, no association between RDCI scores and disease activity was found. Independent predictors of a good clinical response were decreasing BMI and the use of tumor necrosis factor-inhibiting medications.
Conclusion: Although a direct relationship between RDCI score and disease activity could not be established, it did have a significant impact on functional impairment. We recommend that routine calculation of RDCI scores could prove useful in identifying multimorbid RA patients with a poor prognosis and help in fine adjustment of treatment goals to restore quality of life.
Disclosures: S. Abdulaziz, None; S. Attar, None; R. Ahmed, None; H. Fida, None; O. Bokhary, None; A. Alyazidi, None; A. Abumohssin, None.

