Back
Poster Session B
Antiphospholipid Syndrome
Session: (0671–0694) Antiphospholipid Syndrome Poster
0685: The Association of Antiphospholipid Antibodies with Previous SARS-CoV-2 Infection Among Elective Knee Replacement Patients
Sunday, November 13, 2022
9:00 AM – 10:30 AM Eastern Time
Location: Virtual Poster Hall

Lisa Mandl, MD, MPH
Hospital for Special Surgery
New York, NY, United States
Abstract Poster Presenter(s)
Lisa Mandl, Medha Barbhaiya, Robyn Lipschultz, Benjamin Swett, Myriam Lin, Agnes Cororaton, Dongmei Sun, Kethy Jules-elysee, Doruk Erkan and Friedrich Boettner, Hospital for Special Surgery, New York, NY
Background/Purpose: Acute SARS-CoV-2 infection has been associated with antiphospholipid antibodies (aPL), though it is unclear if aPL contribute to the hypercoagulability seen with COVID19, or if these aPL persist. We evaluated patients undergoing elective total knee replacement (TKR), a procedure with known risks of thrombosis, and compared aPL positivity in those with and without previous SARS-CoV-2 infection.
Methods: We recruited patients with osteoarthritis undergoing TKR at a single center between 10/2020 and 10/2021. Patients were screened for previous SARS-CoV-2 infection with a serum nucleocapsid IgG, and a cohort was assembled matching SARS-CoV-2 IgG +ve patients on age (+/- 5 years), gender, and body mass index (BMI kg/m2 ≤ 35 vs. > 35) with SARS-CoV-2 IgG -ve patients without self-reported COVID19. aPL (lupus anticoagulant [LA], anticardiolipin antibodies [aCL] IgG/M/A, and anti-β2-glycoprotein-I [aβ2GPI] IgG/M/A] were performed pre-operatively on all subjects, and 6 weeks later in the SARS-CoV-2 IgG +ve cases.
Results: 156 subjects enrolled, (73 cases:73 controls), average age 63.2 years (SD 8.0), 53.4% women, BMI 31.9 kg/m2 (SD 6.0), 78.8% Caucasian. 46/73 (63%) SARS-CoV-2 IgG +ve cases reported COVID19 symptoms; time between COVID19 symptoms and TKR was 243.3 days, (range: 17 – 597). 21% of both groups were positive for at least one aPL; the most common aPL type/isotype was aCL IgM (11% in SARS-CoV-2 +ve and 15% in SARS CoV-2 -ve). Other aPL types/isotypes ranged between 1-3% in both groups. 58/73 (80%) SARS-CoV-2 +ve cases had 6-week follow-up; of the 12 aPL-positive/SARS-CoV-2 +ve cases re-assessed at 6 weeks, 6/12 (50%) had disappearance of aPL (See Table). Among SARS-CoV-2 IgG +ve cases, a higher proportion of those reporting ≥ 5 COVID19 symptoms at time of clinical infection had any positive aPL both pre-operatively (40% vs 29%) and at 6 weeks (50% vs 31%). There was one deep vein thrombosis in a SARS-CoV-2 IgG +ve case. There were no differences in pain or function at 6 weeks between the 6 SARS-CoV-2 IgG +ve cases who were +ve for aPL at baseline and remained +ve at 6 weeks, and those who became negative for aCL.
Conclusion: Regardless of previous SARS-CoV-2 infection, approximately one-fifth of patients undergoing elective TKR for osteoarthritis had positive aPL, mostly low level (20-39U) aCL IgM. Half of SARS-CoV-2 nucleocapsid IgG +ve /aPL-positive subjects became aPL negative at 6-weeks, and aCL status was not associated with pain or function at 6 weeks. These data contribute to our understanding of aCL prevalence, and suggest SARS-CoV-2 nucleocapsid IgG may not be associated with increased incidence of aCL.
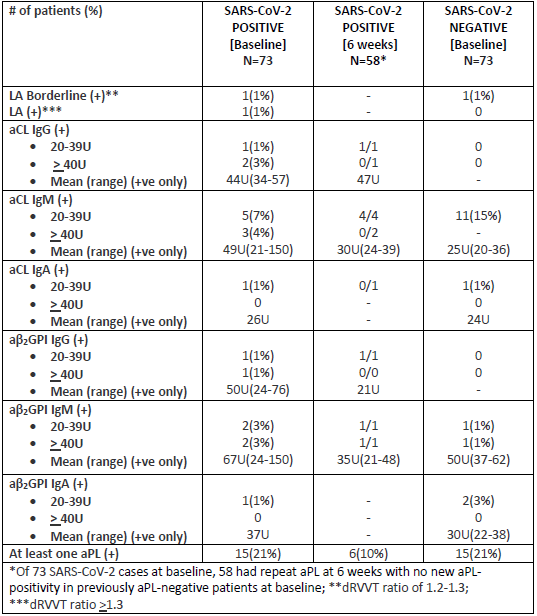 Table 1
Table 1
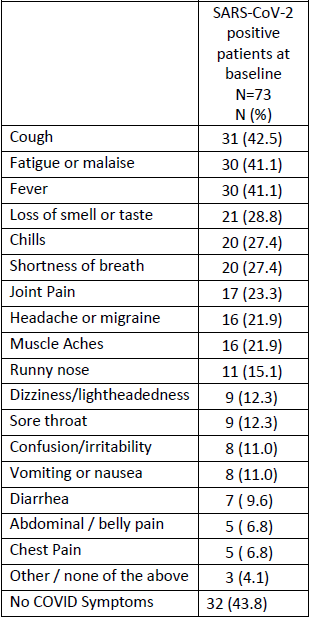 Table 2
Table 2
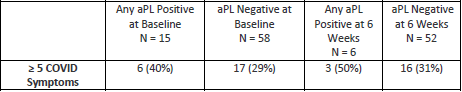 Table 3
Table 3
Disclosures: L. Mandl, Pfizer; M. Barbhaiya, None; R. Lipschultz, None; B. Swett, None; M. Lin, None; A. Cororaton, None; D. Sun, None; K. Jules-elysee, None; D. Erkan, None; F. Boettner, Smith and Nephew, Ortho Development.
Background/Purpose: Acute SARS-CoV-2 infection has been associated with antiphospholipid antibodies (aPL), though it is unclear if aPL contribute to the hypercoagulability seen with COVID19, or if these aPL persist. We evaluated patients undergoing elective total knee replacement (TKR), a procedure with known risks of thrombosis, and compared aPL positivity in those with and without previous SARS-CoV-2 infection.
Methods: We recruited patients with osteoarthritis undergoing TKR at a single center between 10/2020 and 10/2021. Patients were screened for previous SARS-CoV-2 infection with a serum nucleocapsid IgG, and a cohort was assembled matching SARS-CoV-2 IgG +ve patients on age (+/- 5 years), gender, and body mass index (BMI kg/m2 ≤ 35 vs. > 35) with SARS-CoV-2 IgG -ve patients without self-reported COVID19. aPL (lupus anticoagulant [LA], anticardiolipin antibodies [aCL] IgG/M/A, and anti-β2-glycoprotein-I [aβ2GPI] IgG/M/A] were performed pre-operatively on all subjects, and 6 weeks later in the SARS-CoV-2 IgG +ve cases.
Results: 156 subjects enrolled, (73 cases:73 controls), average age 63.2 years (SD 8.0), 53.4% women, BMI 31.9 kg/m2 (SD 6.0), 78.8% Caucasian. 46/73 (63%) SARS-CoV-2 IgG +ve cases reported COVID19 symptoms; time between COVID19 symptoms and TKR was 243.3 days, (range: 17 – 597). 21% of both groups were positive for at least one aPL; the most common aPL type/isotype was aCL IgM (11% in SARS-CoV-2 +ve and 15% in SARS CoV-2 -ve). Other aPL types/isotypes ranged between 1-3% in both groups. 58/73 (80%) SARS-CoV-2 +ve cases had 6-week follow-up; of the 12 aPL-positive/SARS-CoV-2 +ve cases re-assessed at 6 weeks, 6/12 (50%) had disappearance of aPL (See Table). Among SARS-CoV-2 IgG +ve cases, a higher proportion of those reporting ≥ 5 COVID19 symptoms at time of clinical infection had any positive aPL both pre-operatively (40% vs 29%) and at 6 weeks (50% vs 31%). There was one deep vein thrombosis in a SARS-CoV-2 IgG +ve case. There were no differences in pain or function at 6 weeks between the 6 SARS-CoV-2 IgG +ve cases who were +ve for aPL at baseline and remained +ve at 6 weeks, and those who became negative for aCL.
Conclusion: Regardless of previous SARS-CoV-2 infection, approximately one-fifth of patients undergoing elective TKR for osteoarthritis had positive aPL, mostly low level (20-39U) aCL IgM. Half of SARS-CoV-2 nucleocapsid IgG +ve /aPL-positive subjects became aPL negative at 6-weeks, and aCL status was not associated with pain or function at 6 weeks. These data contribute to our understanding of aCL prevalence, and suggest SARS-CoV-2 nucleocapsid IgG may not be associated with increased incidence of aCL.
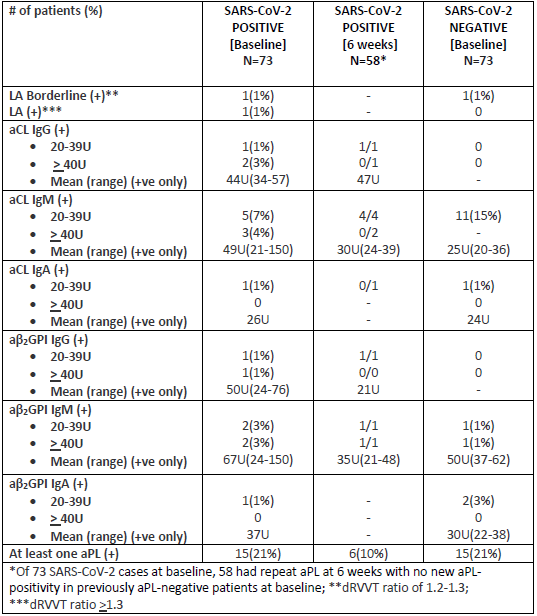 Table 1
Table 1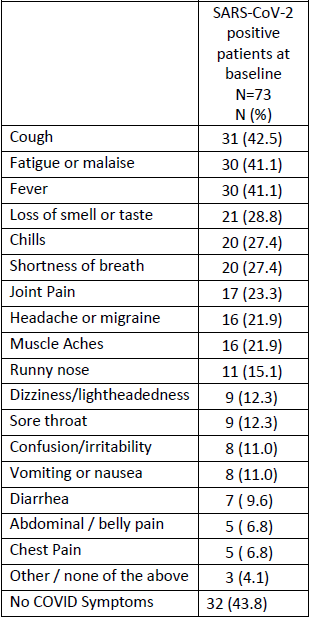 Table 2
Table 2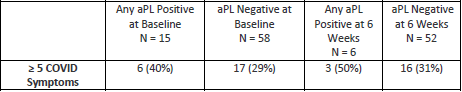 Table 3
Table 3Disclosures: L. Mandl, Pfizer; M. Barbhaiya, None; R. Lipschultz, None; B. Swett, None; M. Lin, None; A. Cororaton, None; D. Sun, None; K. Jules-elysee, None; D. Erkan, None; F. Boettner, Smith and Nephew, Ortho Development.

