Back
Poster Session C
Rheumatoid arthritis (RA)
Session: (1387–1416) RA – Diagnosis, Manifestations, and Outcomes Poster III
1414: 2022 Revision of the ACR/EULAR Remission Criteria for Rheumatoid Arthritis
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall

Paul Studenic, MD, PhD
Medical University of Vienna
Vienna, Austria
Abstract Poster Presenter(s)
Paul Studenic1, Daniel Aletaha2, Maarten de Wit3, Tanja Stamm4, Farideh Alasti5, Diane Lacaille6, Josef Smolen1 and David Felson7, 1Medical University of Vienna, Vienna, Austria, 2Medical University Vienna, Wien, Austria, 3Patient research partner, Amsterdam, Netherlands, 4Medical University of Vienna, CeMSIIS - Center for Medical Statistics, Informatics, and Intelligent Systems, Section for Outcomes Research, Wien, Austria, 5Medical University of Vienna, Department of Internal Medicine 3, Division of Rheumatology, Vienna, Austria, 6Arthritis Research Canada, University of British Columbia, Vancouver, BC, Canada, 7Boston University, Boston, MA
Background/Purpose: More than 10 years ago ACR and EULAR endorsed provisional criteria to define remission in RA, both Boolean and index-based. However, the agreement between these two sets of criteria was moderate, especially if patient global assessment (PGA) was >1 (0-10). Recent studies indicated that a higher threshold for the PGA improved this agreement. We aimed to externally validate a revision of the Boolean remission criteria using a higher PGA threshold and to validate the provisionally endorsed index-based criteria.
Methods: Data from 4 randomized trials of biologic disease modifying antirheumatic drugs (bDMARDs) vs. methotrexate (MTX) or placebo were analyzed. We tested a higher proposed PGA (Visual Analogue Scale; 0-10) threshold of 2 (Boolean 2.0) vs. the original threshold of 1 (Boolean 1.0). We analyzed agreement between the Boolean and index-based criteria (SDAI, CDAI). We further examined how fulfilling each remission definition at 6 months predicted good physical function (HAQ < =0.5) and radiographic non-progression (predictive validity) at one year. A Boolean definition without the PGA (BooleanX) was also assessed.
Results: Data from 2048 trial participants, 1101 with early (disease duration ≤2years) and 947 with established RA were included. The proportion of participants in remission at 6 months increased when using Boolean2.0 compared to Boolean1.0 from 14.8% to 20.6% in early RA and 4.2% to 6.0% in established RA (Figure 1). Agreement between Boolean2.0 and the SDAI or CDAI remission criteria was better than for Boolean1.0, particularly in early disease (Table 1). Boolean2.0, SDAI and CDAI remission criteria had similar positive likelihood (LR+) ratios to predict radiographic non-progression and a HAQ of ≤0.5 (Table 2). The proportion of participants achieving both good radiographic and functional outcomes, were similar for all remission definitions, from 57 to 60% (Boolean1.0, 2.0, SDAI and CDAI: 58.6%, 57.3%, 59.2% and 60.4%), except for BooleanX (50.8%).
Conclusion: Using the Boolean2.0 definition increases the agreement with index-based remission criteria and classifies more patients as reaching remission than Boolean 1.0. Boolean2.0, SDAI and CDAI but not definitions of remission without patient global assessment coincide with a good predictive value for both radiographic and functional outcomes.
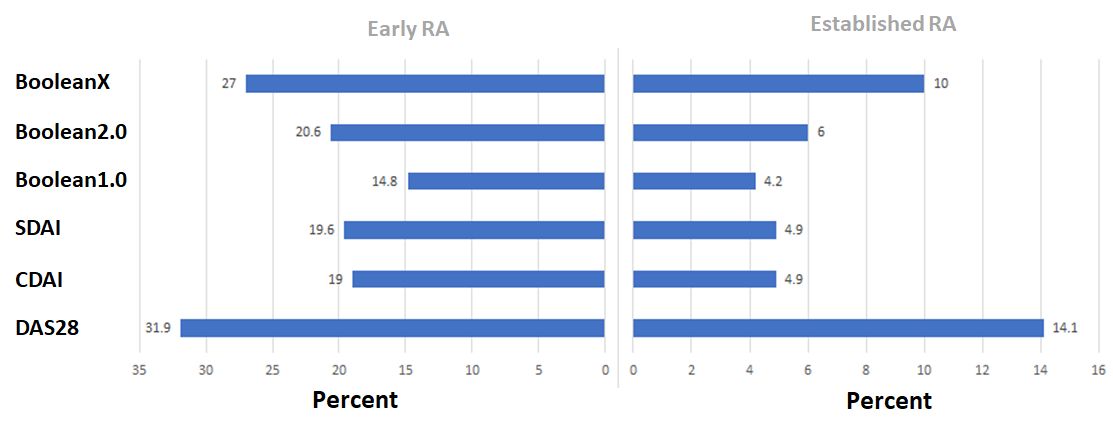 Figure 1: Rates of remission by modified Boolean classifications, using a PGA threshold of 1.0 (“Boolean”), 2.0 or omitting the PGA completely (BooleanX) as well as for the SDAI, CDAI and DAS28 definition. Rates at 6 months in % of total, separately depicted for early RA patients on the left and for established RA on the right.
Figure 1: Rates of remission by modified Boolean classifications, using a PGA threshold of 1.0 (“Boolean”), 2.0 or omitting the PGA completely (BooleanX) as well as for the SDAI, CDAI and DAS28 definition. Rates at 6 months in % of total, separately depicted for early RA patients on the left and for established RA on the right.
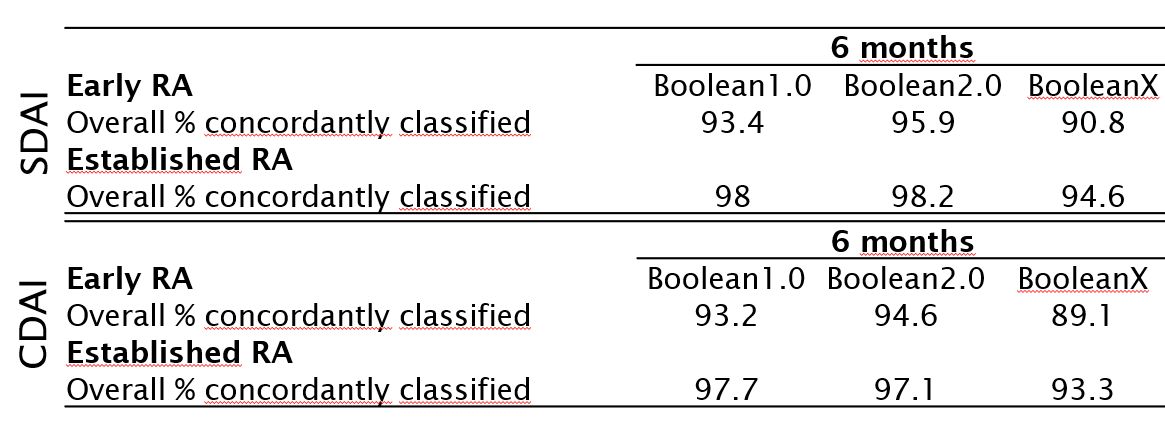 Table 1: Agreement Rates (% concordantly classified) between different modified Boolean remission definitions with the index-based remission definitions. Provided for 6 months. Upper table: Agreement with SDAI remission, lower table with CDAI remission.
Table 1: Agreement Rates (% concordantly classified) between different modified Boolean remission definitions with the index-based remission definitions. Provided for 6 months. Upper table: Agreement with SDAI remission, lower table with CDAI remission.
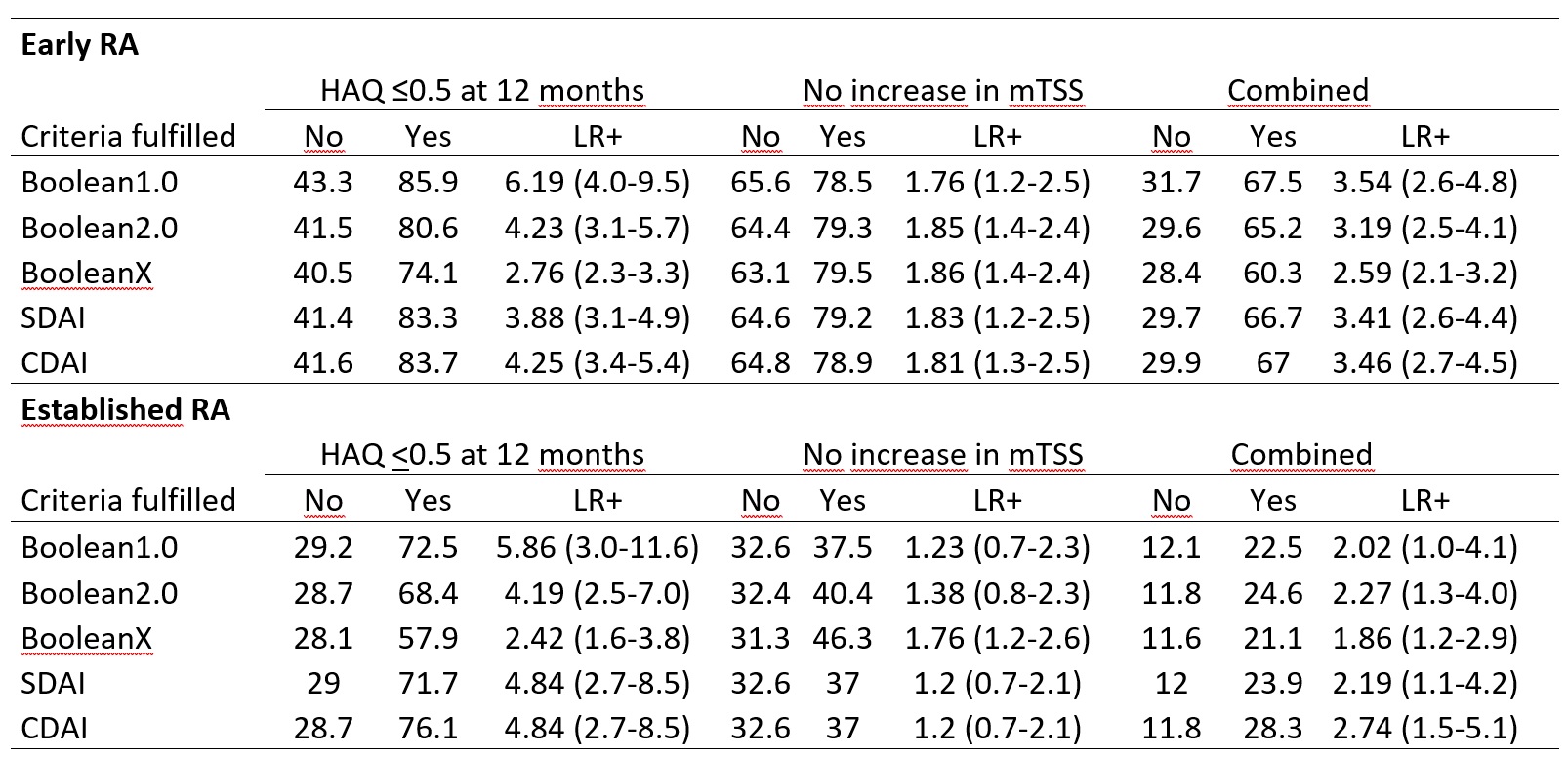 Table 2: Percent of patients with a HAQ≤0.5, no increase in modified total Sharp Score (mTSS) / no radiographic progression, or both combined among those either fulfilling, or not fulfilling, the respective remission definition (Boolean1.0, Boolean2.0, BooleanX, SDAI-based, CDAI based definitions). Positive Likelihood ratios (LR+) for reaching the respective outcome at 12 months if remission is achieved at 6 months.
Table 2: Percent of patients with a HAQ≤0.5, no increase in modified total Sharp Score (mTSS) / no radiographic progression, or both combined among those either fulfilling, or not fulfilling, the respective remission definition (Boolean1.0, Boolean2.0, BooleanX, SDAI-based, CDAI based definitions). Positive Likelihood ratios (LR+) for reaching the respective outcome at 12 months if remission is achieved at 6 months.
Disclosures: P. Studenic, AbbVie/Abbott; D. Aletaha, Novartis, SoBi, Sanofi, Amgen, Lilly, Merck, Pfizer, Roche, Sandoz, Janssen, AbbVie; M. de Wit, Stiching Tools, Celgene, Eli Lilly, Pfizer, UCB; T. Stamm, AbbVie/Abbott, Roche, Sanofi Genzyme, Takeda, Novartis; F. Alasti, None; D. Lacaille, None; J. Smolen, AbbVie, AstraZeneca, Eli Lilly, Novartis, Amgen, Bristol Myers Squibb, Galapagos-Gilead, Janssen, Merck-Sharp-Dohme, Novartis-Sandoz, Pfizer, Roche-Chugai, Samsung, UCB; D. Felson, None.
Background/Purpose: More than 10 years ago ACR and EULAR endorsed provisional criteria to define remission in RA, both Boolean and index-based. However, the agreement between these two sets of criteria was moderate, especially if patient global assessment (PGA) was >1 (0-10). Recent studies indicated that a higher threshold for the PGA improved this agreement. We aimed to externally validate a revision of the Boolean remission criteria using a higher PGA threshold and to validate the provisionally endorsed index-based criteria.
Methods: Data from 4 randomized trials of biologic disease modifying antirheumatic drugs (bDMARDs) vs. methotrexate (MTX) or placebo were analyzed. We tested a higher proposed PGA (Visual Analogue Scale; 0-10) threshold of 2 (Boolean 2.0) vs. the original threshold of 1 (Boolean 1.0). We analyzed agreement between the Boolean and index-based criteria (SDAI, CDAI). We further examined how fulfilling each remission definition at 6 months predicted good physical function (HAQ < =0.5) and radiographic non-progression (predictive validity) at one year. A Boolean definition without the PGA (BooleanX) was also assessed.
Results: Data from 2048 trial participants, 1101 with early (disease duration ≤2years) and 947 with established RA were included. The proportion of participants in remission at 6 months increased when using Boolean2.0 compared to Boolean1.0 from 14.8% to 20.6% in early RA and 4.2% to 6.0% in established RA (Figure 1). Agreement between Boolean2.0 and the SDAI or CDAI remission criteria was better than for Boolean1.0, particularly in early disease (Table 1). Boolean2.0, SDAI and CDAI remission criteria had similar positive likelihood (LR+) ratios to predict radiographic non-progression and a HAQ of ≤0.5 (Table 2). The proportion of participants achieving both good radiographic and functional outcomes, were similar for all remission definitions, from 57 to 60% (Boolean1.0, 2.0, SDAI and CDAI: 58.6%, 57.3%, 59.2% and 60.4%), except for BooleanX (50.8%).
Conclusion: Using the Boolean2.0 definition increases the agreement with index-based remission criteria and classifies more patients as reaching remission than Boolean 1.0. Boolean2.0, SDAI and CDAI but not definitions of remission without patient global assessment coincide with a good predictive value for both radiographic and functional outcomes.
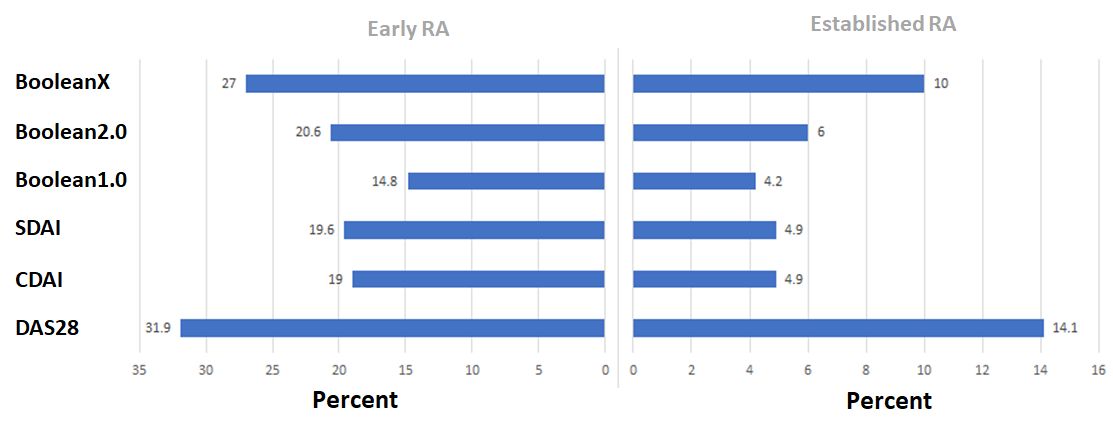 Figure 1: Rates of remission by modified Boolean classifications, using a PGA threshold of 1.0 (“Boolean”), 2.0 or omitting the PGA completely (BooleanX) as well as for the SDAI, CDAI and DAS28 definition. Rates at 6 months in % of total, separately depicted for early RA patients on the left and for established RA on the right.
Figure 1: Rates of remission by modified Boolean classifications, using a PGA threshold of 1.0 (“Boolean”), 2.0 or omitting the PGA completely (BooleanX) as well as for the SDAI, CDAI and DAS28 definition. Rates at 6 months in % of total, separately depicted for early RA patients on the left and for established RA on the right.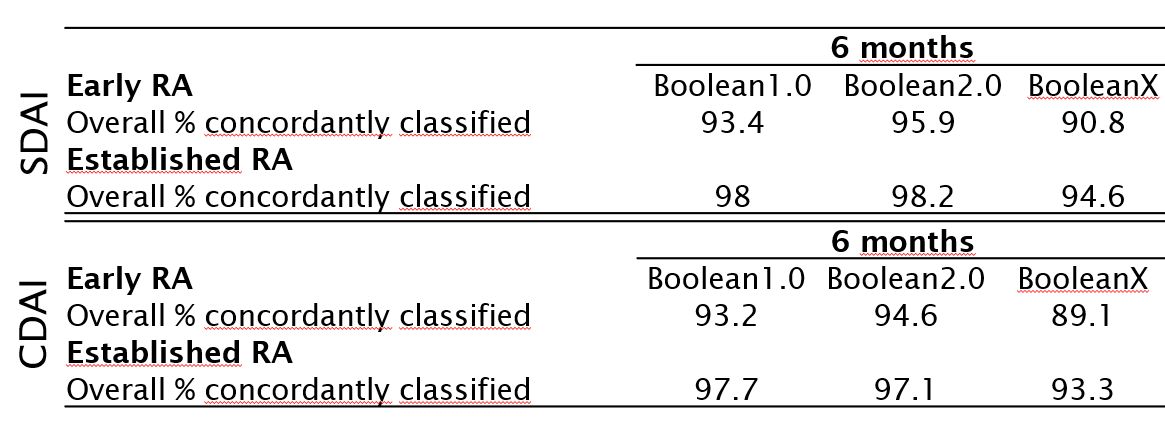 Table 1: Agreement Rates (% concordantly classified) between different modified Boolean remission definitions with the index-based remission definitions. Provided for 6 months. Upper table: Agreement with SDAI remission, lower table with CDAI remission.
Table 1: Agreement Rates (% concordantly classified) between different modified Boolean remission definitions with the index-based remission definitions. Provided for 6 months. Upper table: Agreement with SDAI remission, lower table with CDAI remission.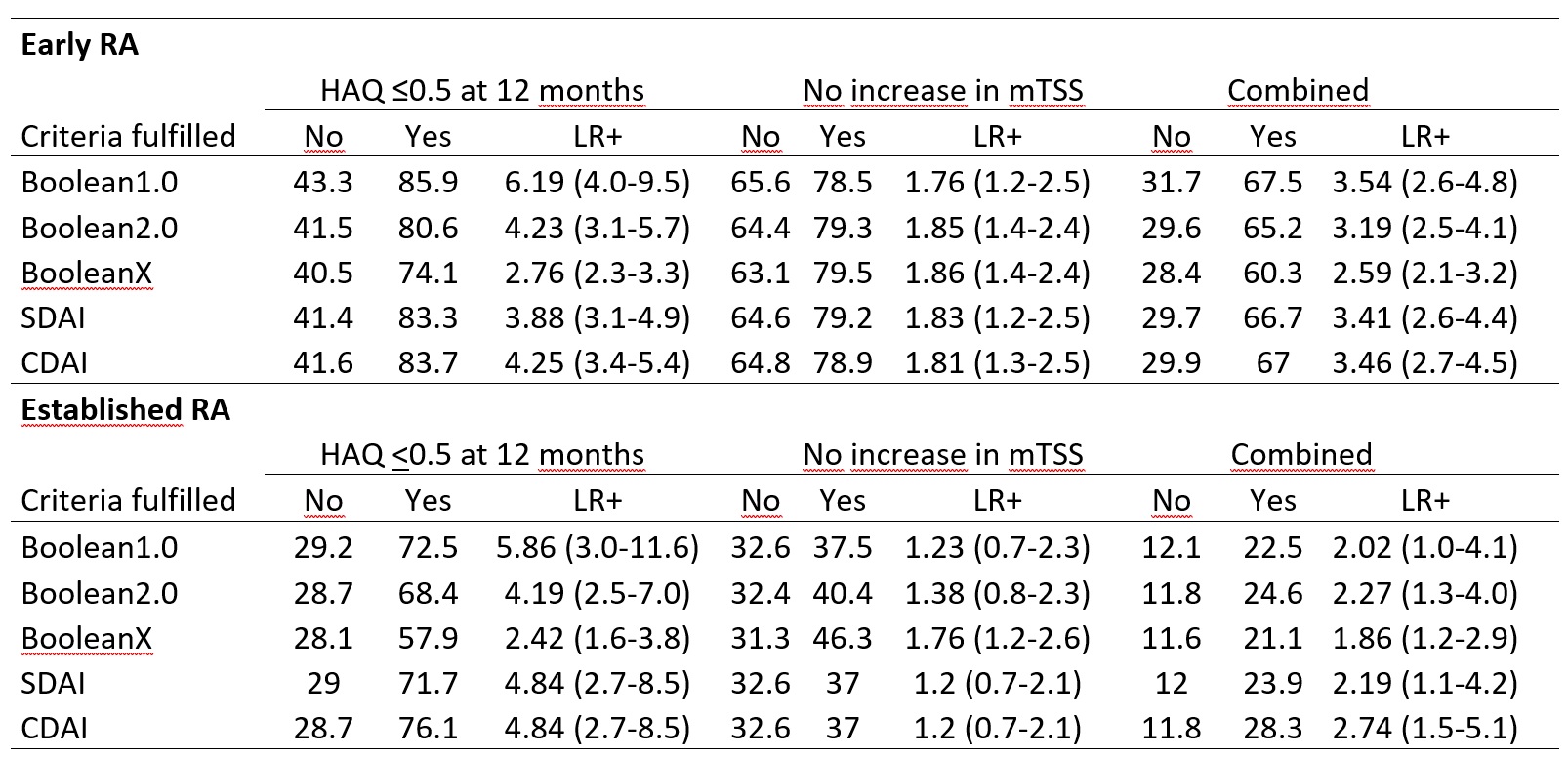 Table 2: Percent of patients with a HAQ≤0.5, no increase in modified total Sharp Score (mTSS) / no radiographic progression, or both combined among those either fulfilling, or not fulfilling, the respective remission definition (Boolean1.0, Boolean2.0, BooleanX, SDAI-based, CDAI based definitions). Positive Likelihood ratios (LR+) for reaching the respective outcome at 12 months if remission is achieved at 6 months.
Table 2: Percent of patients with a HAQ≤0.5, no increase in modified total Sharp Score (mTSS) / no radiographic progression, or both combined among those either fulfilling, or not fulfilling, the respective remission definition (Boolean1.0, Boolean2.0, BooleanX, SDAI-based, CDAI based definitions). Positive Likelihood ratios (LR+) for reaching the respective outcome at 12 months if remission is achieved at 6 months.Disclosures: P. Studenic, AbbVie/Abbott; D. Aletaha, Novartis, SoBi, Sanofi, Amgen, Lilly, Merck, Pfizer, Roche, Sandoz, Janssen, AbbVie; M. de Wit, Stiching Tools, Celgene, Eli Lilly, Pfizer, UCB; T. Stamm, AbbVie/Abbott, Roche, Sanofi Genzyme, Takeda, Novartis; F. Alasti, None; D. Lacaille, None; J. Smolen, AbbVie, AstraZeneca, Eli Lilly, Novartis, Amgen, Bristol Myers Squibb, Galapagos-Gilead, Janssen, Merck-Sharp-Dohme, Novartis-Sandoz, Pfizer, Roche-Chugai, Samsung, UCB; D. Felson, None.

