Back
Poster Session C
Systemic lupus erythematosus (SLE)
Session: (1440–1485) SLE – Diagnosis, Manifestations, and Outcomes Poster II: Manifestations
1476: Anti-Neutrophil Extracellular Traps (NET) Antibodies and Their Association with Disease Activity and Clinical Phenotypes in Systemic Lupus Erythematosus
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- RA
Rosa Arvizu-Rivera, MD
Instituto Nacional de Ciencias Medicas y Nutricion Salvador Zubiran
Tlalpan, Federal District, Mexico
Abstract Poster Presenter(s)
Rosa Arvizu-Rivera1, jiram torres-Ruiz2, Alfredo Pérez-Fragoso2, Beatriz Alcalá-Carmona3, Miroslava Nuñez-Aguirre4, Ana Sofía Vargas-Castro4, Abdiel Absalón-Aguilar3, Jaquelin Lira-Luna4 and Diana Gómez-Martín2, 1Instituto Nacional de Ciencias Medicas y Nutricion Salvador Zubiran, Ciudad de México, Mexico, 2INCMNSZ, Ciudad de México, Mexico, 3Department of Immunology and Rheumatology, Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán, Ciudad de México, Mexico, 4Instituto Nacional de Ciencias Medicas y Nutricion "Salvador Zubiran", Ciudad de México, Mexico
Background/Purpose: Enhanced netosis has been acknowledged as pathogenic in Systemic Lupus Erythematosus (SLE). The presence of antibodies against neutrophil extracellular traps (anti-NETs) in patients with SLE might contribute to deficient degradation of NETs in these patients. Additionally, anti-NET antibodies can bind to NETs and form immune complexes and increase NET formation by neutrophils. Previously, the presence of antibodies against components of NETs has been associated with proteinuria, activity index in lupus nephritis and increased SLEDAI. However, there is scarce information about the prevalence of anti-NET antibodies and their correlation with clinical characteristics of SLE patients.
We aimed to analyze the prevalence of IgG anti-NET antibodies and their association with disease activity and clinical features in patients with SLE.
Methods: We included patients older than 18 years old who fulfilled the ACR/SLICC 2012 classification criteria for SLE. Exclusion criteria included pregnancy, overlap syndrome, malignancy, and recent COVID-19 infection. NETs were quantified ex vivo and IgG anti-NETs were detected using ELISA as previously described. Twenty-three healthy controls were included to establish the cut-off point for anti-NETs, resulting in a cut-off point of 0.076 AU (OD). Correlations between non parametric variables were performed using Spearman's rho.
Results: A total of 87 patients with SLE were included. The majority were women (88%) with a median age of 31.13 years. Their main clinical features as depicted in Table 1. Median levels of anti-NET antibodies were 0.30 OD, and 31 patients (35.6%) were considered to have anti-NET antibodies positivity. Patients were divided according to their clinical manifestations and analyzed for anti-NET antibodies positivity; results are shown in Table 2. Besides, we analyzed correlations between anti-NET antibodies levels and levels of SLEDAI, C3, C4, absolute lymphocyte count and anti-dsDNA (Table 3). A statistically significant positive correlation between anti-NET antibodies with SLEDAI (r=0.245) and anti-dsDNA antibodies (r=0.290) was found.
Conclusion: IgG anti-NET antibodies were found in approximately one third of SLE patients, Higher prevalence of antibody positivity was found in SLE patients with serological activity, serositis and lupus nephritis. Increased levels of anti-NET antibodies correlated with increased SLEDAI and anti-dsDNA titers. To our knowledge, this is the first description of the association between IgG anti-NET and clinical features of SLE. Their characterization might allow us to address their role as potential novel biomarkers.
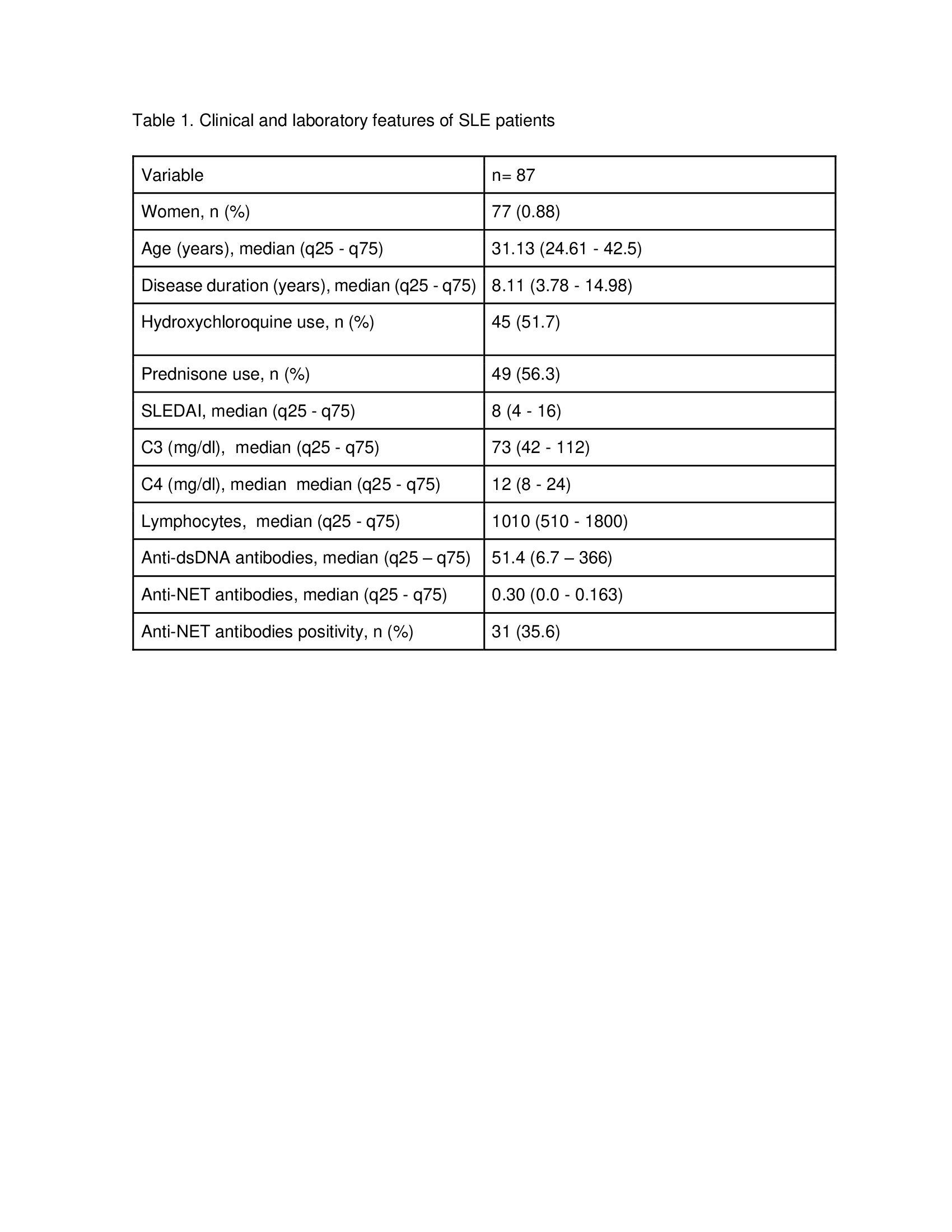 Table 1. Clinical and laboratory features of SLE patients
Table 1. Clinical and laboratory features of SLE patients
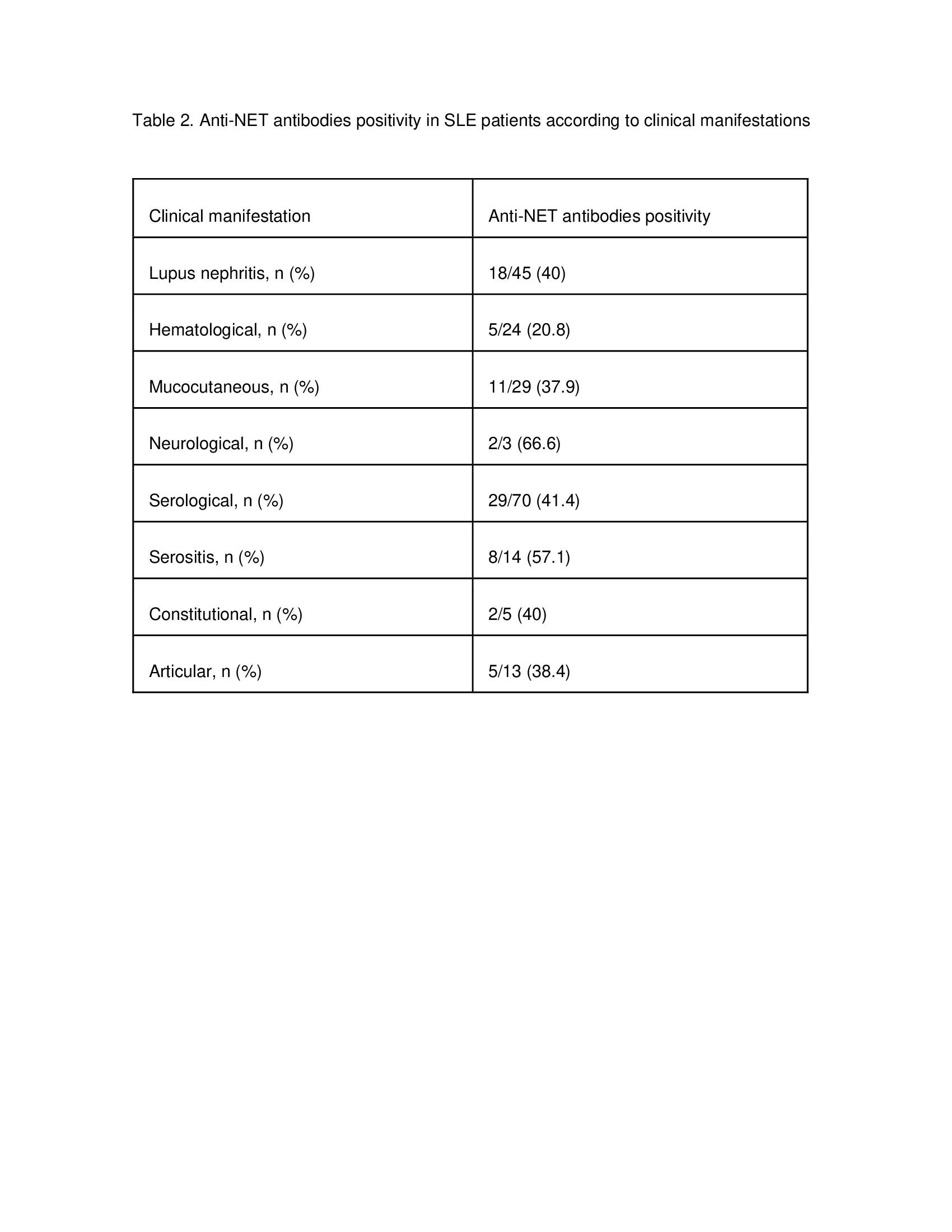 Table 2. Anti-NET antibodies positivity in SLE patients according to clinical manifestations
Table 2. Anti-NET antibodies positivity in SLE patients according to clinical manifestations
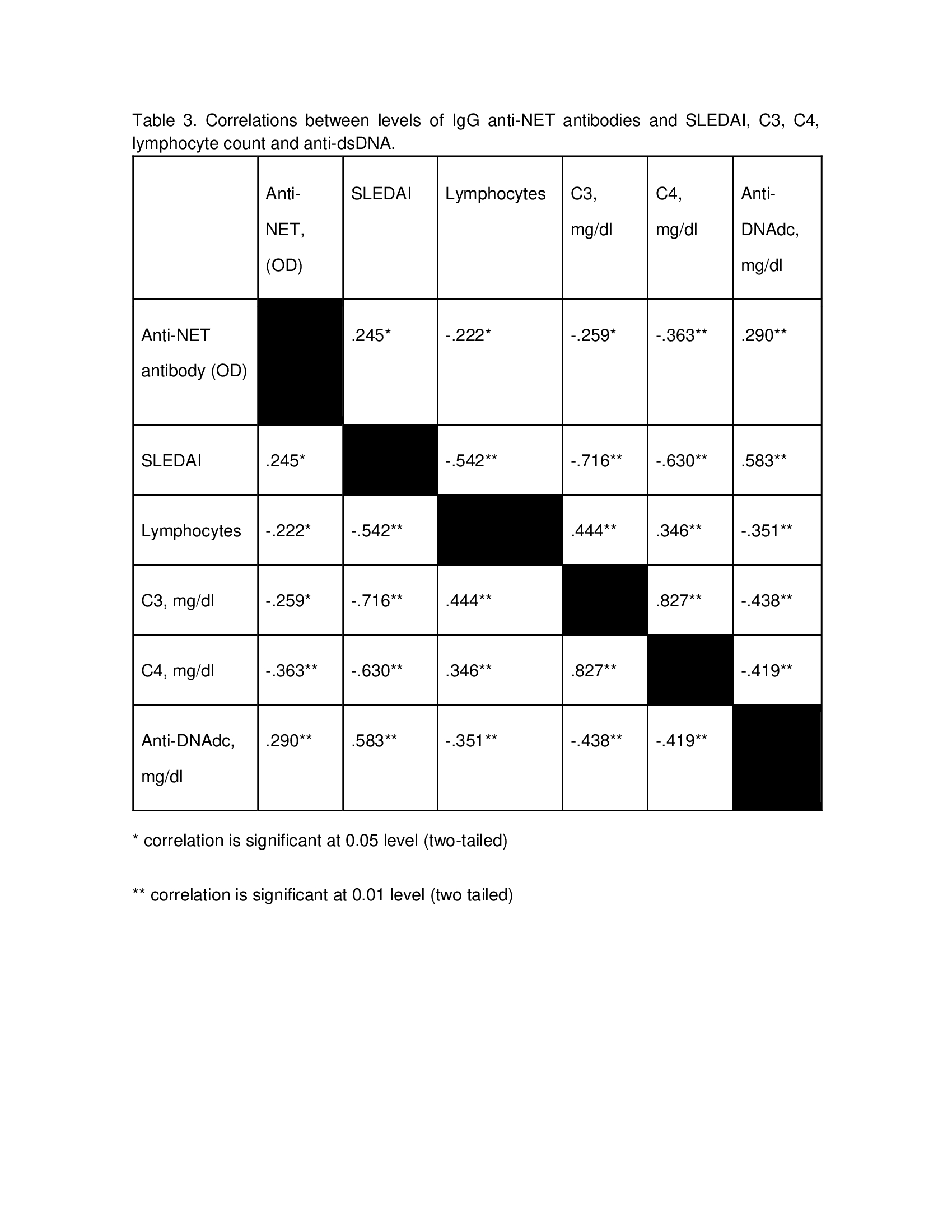 Table 3. Correlations between levels of IgG anti-NET antibodies and SLEDAI, C3, C4, lymphocyte count and anti-dsDNA.
Table 3. Correlations between levels of IgG anti-NET antibodies and SLEDAI, C3, C4, lymphocyte count and anti-dsDNA.
Disclosures: R. Arvizu-Rivera, None; j. torres-Ruiz, None; A. Pérez-Fragoso, None; B. Alcalá-Carmona, None; M. Nuñez-Aguirre, None; A. Vargas-Castro, None; A. Absalón-Aguilar, None; J. Lira-Luna, None; D. Gómez-Martín, None.
Background/Purpose: Enhanced netosis has been acknowledged as pathogenic in Systemic Lupus Erythematosus (SLE). The presence of antibodies against neutrophil extracellular traps (anti-NETs) in patients with SLE might contribute to deficient degradation of NETs in these patients. Additionally, anti-NET antibodies can bind to NETs and form immune complexes and increase NET formation by neutrophils. Previously, the presence of antibodies against components of NETs has been associated with proteinuria, activity index in lupus nephritis and increased SLEDAI. However, there is scarce information about the prevalence of anti-NET antibodies and their correlation with clinical characteristics of SLE patients.
We aimed to analyze the prevalence of IgG anti-NET antibodies and their association with disease activity and clinical features in patients with SLE.
Methods: We included patients older than 18 years old who fulfilled the ACR/SLICC 2012 classification criteria for SLE. Exclusion criteria included pregnancy, overlap syndrome, malignancy, and recent COVID-19 infection. NETs were quantified ex vivo and IgG anti-NETs were detected using ELISA as previously described. Twenty-three healthy controls were included to establish the cut-off point for anti-NETs, resulting in a cut-off point of 0.076 AU (OD). Correlations between non parametric variables were performed using Spearman's rho.
Results: A total of 87 patients with SLE were included. The majority were women (88%) with a median age of 31.13 years. Their main clinical features as depicted in Table 1. Median levels of anti-NET antibodies were 0.30 OD, and 31 patients (35.6%) were considered to have anti-NET antibodies positivity. Patients were divided according to their clinical manifestations and analyzed for anti-NET antibodies positivity; results are shown in Table 2. Besides, we analyzed correlations between anti-NET antibodies levels and levels of SLEDAI, C3, C4, absolute lymphocyte count and anti-dsDNA (Table 3). A statistically significant positive correlation between anti-NET antibodies with SLEDAI (r=0.245) and anti-dsDNA antibodies (r=0.290) was found.
Conclusion: IgG anti-NET antibodies were found in approximately one third of SLE patients, Higher prevalence of antibody positivity was found in SLE patients with serological activity, serositis and lupus nephritis. Increased levels of anti-NET antibodies correlated with increased SLEDAI and anti-dsDNA titers. To our knowledge, this is the first description of the association between IgG anti-NET and clinical features of SLE. Their characterization might allow us to address their role as potential novel biomarkers.
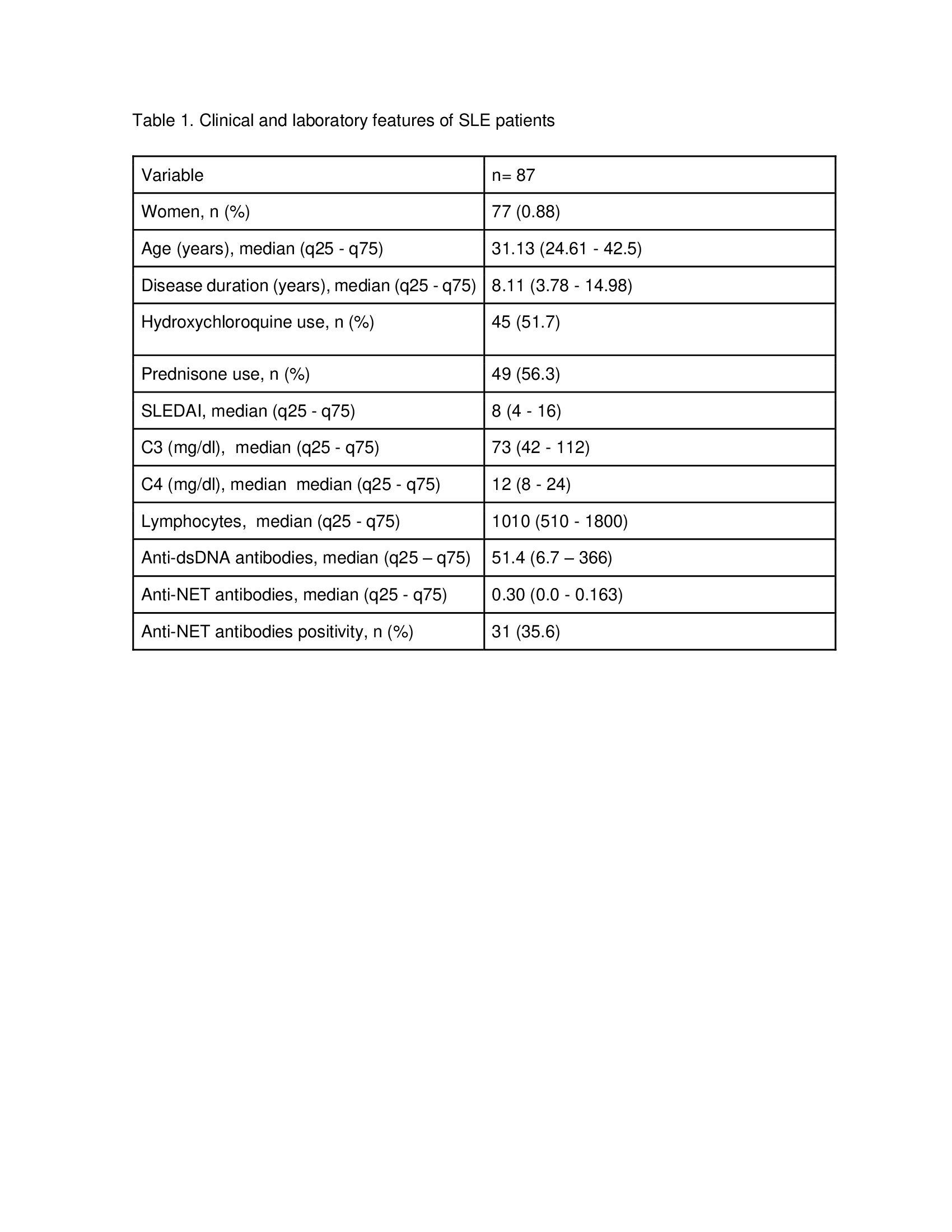 Table 1. Clinical and laboratory features of SLE patients
Table 1. Clinical and laboratory features of SLE patients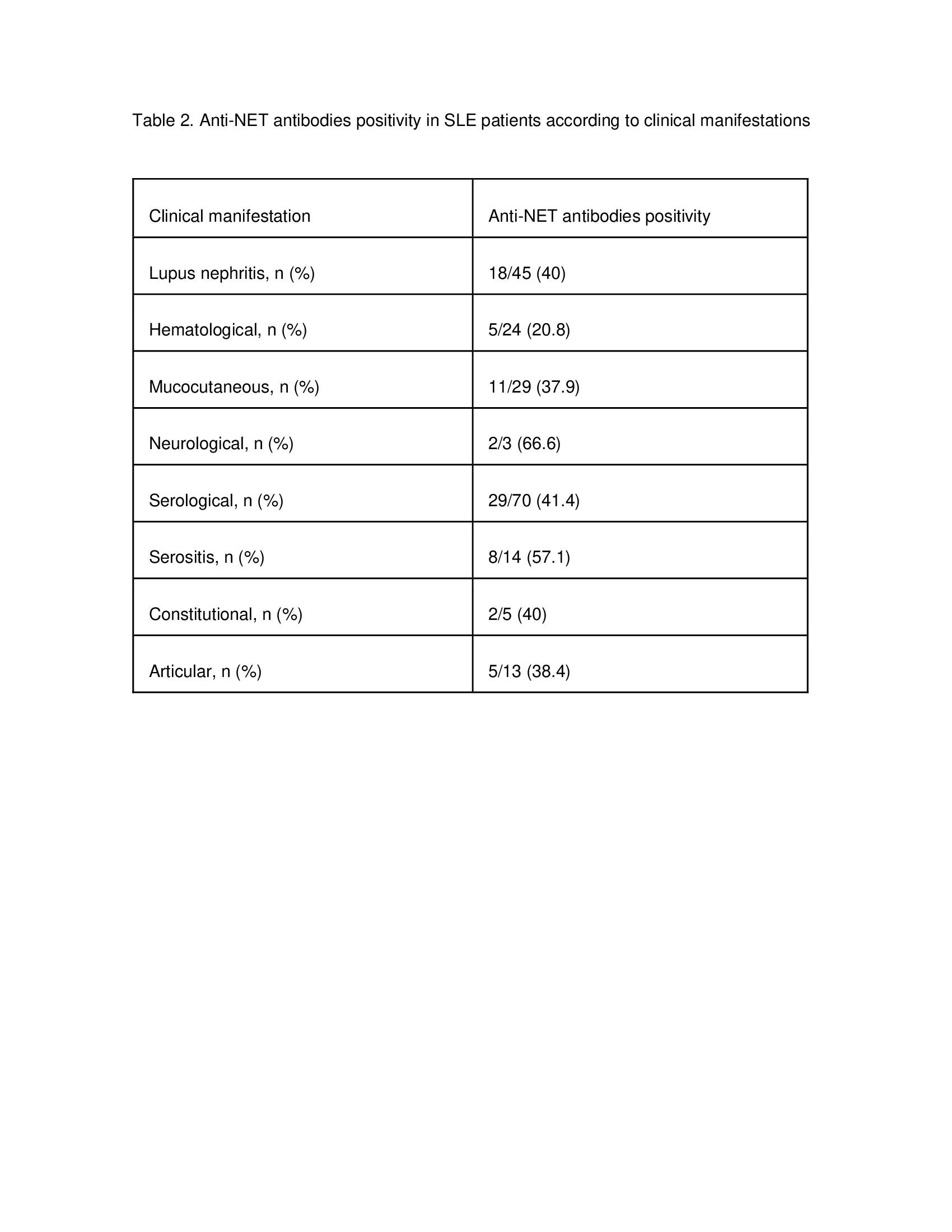 Table 2. Anti-NET antibodies positivity in SLE patients according to clinical manifestations
Table 2. Anti-NET antibodies positivity in SLE patients according to clinical manifestations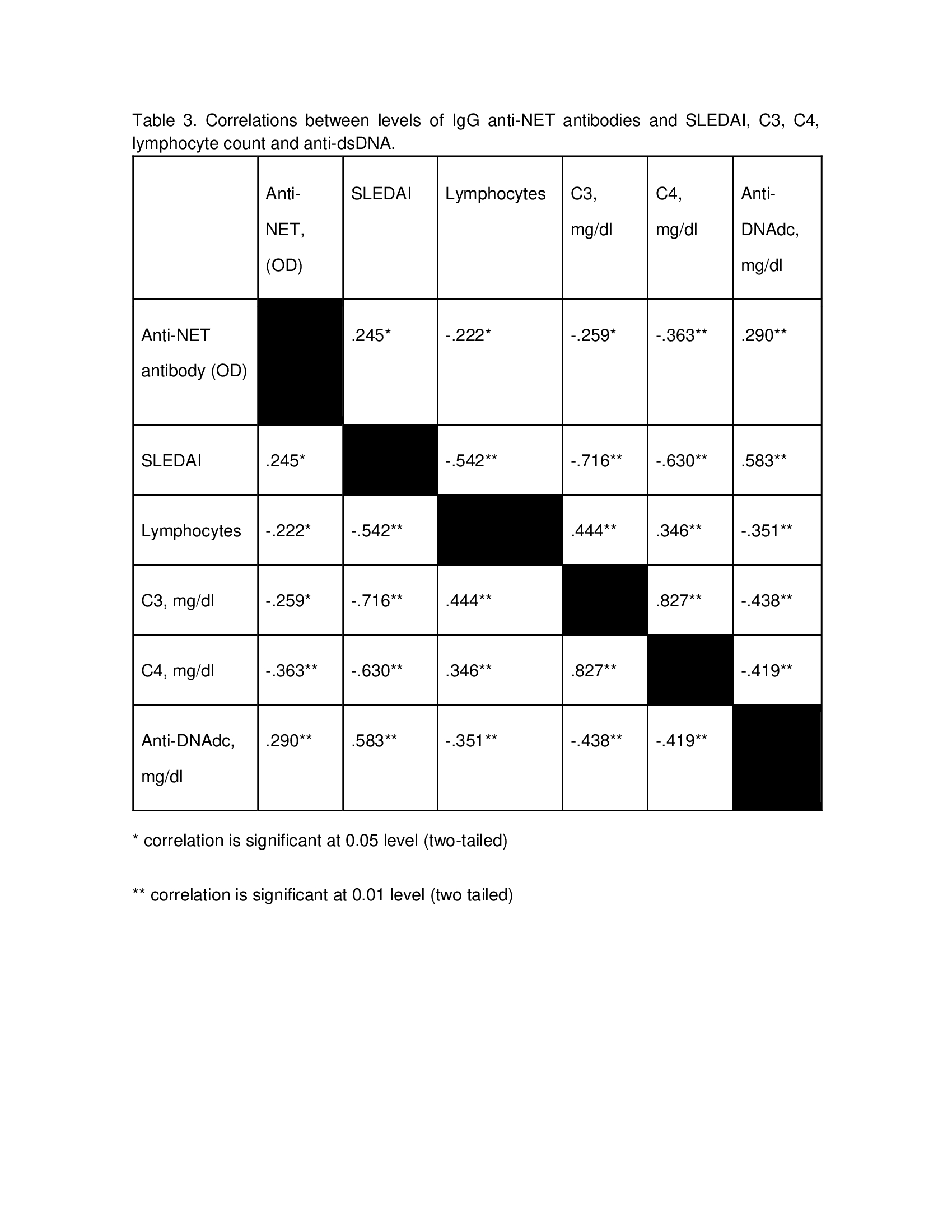 Table 3. Correlations between levels of IgG anti-NET antibodies and SLEDAI, C3, C4, lymphocyte count and anti-dsDNA.
Table 3. Correlations between levels of IgG anti-NET antibodies and SLEDAI, C3, C4, lymphocyte count and anti-dsDNA.Disclosures: R. Arvizu-Rivera, None; j. torres-Ruiz, None; A. Pérez-Fragoso, None; B. Alcalá-Carmona, None; M. Nuñez-Aguirre, None; A. Vargas-Castro, None; A. Absalón-Aguilar, None; J. Lira-Luna, None; D. Gómez-Martín, None.

