Back
Poster Session C
Vasculitis
Session: (1543–1578) Vasculitis – Non-ANCA-Associated and Related Disorders Poster II
1576: Clinical Presentation and Outcome of Patients with Chronic Abdominal Periaortitis
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- UG
Umar Ghaffar, MBBS
Mayo Clinic
Rochester, MN, United States
Abstract Poster Presenter(s)
Umar Ghaffar1, Hannah Langenfeld2, Cynthia Crowson3, Tanaz Kermani4, Michelle Burke1, Boyd Viers1, Aaron Potretzke1, Haraldur Bjarnason1, Kenneth J. Warrington1 and Matthew J. Koster1, 1Mayo Clinic, Rochester, MN, 2Department of Quantitative Health Sciences, Mayo Clinic, Rochester, MN, 3Mayo Clinic, Eyota, MN, 4University of California Los Angeles, West Hills, CA
Background/Purpose: To evaluate the presentation features and outcomes of patients with chronic abdominal periaortitis in a large referral cohort.
Methods: Using a proprietary medical text search algorithm, all patients from 1/1/1996 to 12/31/2019 with mention of 'periaortitis,' 'periaortic soft tissue,' or 'retroperitoneal fibrosis' in the medical chart were screened. Patients with radiographic confirmation of infra-renal abdominal aorta (irAbAo) periaortitis were included. Cases with soft tissue thickening elsewhere were excluded unless they had concomitant irAbAo periaortitis. Patients were further characterized based on presence/absence of aneurysm and associated conditions (Table 1). Cox models were used to examine associations between patient characteristics and outcomes.
Results: 2,507 charts were manually reviewed and 495 patients were identified: 326 (66%) male, 403 (81%) white and 70% (307/436) current or former smokers (Table 2). Mean (SD) age at diagnosis was 57.4 (11.7) years. Most common features at presentation included abdominal pain (44%), back pain (40%), renal insufficiency (36%). End-stage renal disease (ESRD) was present in 52 (12%) at diagnosis. Ureteral stents were placed in 236 (48%): unilateral (n=93), bilateral (n=143). Percutaneous nephrostomy tubes were used in 50 patients, 20 due to stent failure or pain. Treatments utilized are listed in Table 2. Prednisone was given in 346 (70%); 79 as monotherapy. The most common steroid-sparing treatments included tamoxifen, methotrexate, and mycophenolate. At last visit, 160 patients were still on prednisone, 57 on tamoxifen and 129 on other immunosuppressive medication. Repeat imaging was available in 455 patients which showed resolution of periaortic thickening in 40 (9%), improvement in 261 (57%), no change in 103 (23%), and worsening in 51 (11%). Of 212 patients with stents and follow-up data, 141 had successful permanent removal. Of patients with nephrostomy tubes, 33 had permanent removal. Compared to baseline, renal function stage at last follow up was improved in 39%, worse in 19% and stayed the same in 42%. Only one patient without ESRD at baseline developed ESRD by last follow-up. Of those with non-aneurysmal irAbAo periaortitis at baseline, only 8% developed aneurysm after presentation. For patients with aneurysm at diagnosis, 14 had intervention, 2 had AbAo rupture. No evaluated factors were associated with likelihood of ureteral stent removal. Factors significantly associated with prednisone discontinuation and radiographic resolution are listed in Table 3.
Conclusion: In this large cohort of patients with chronic abdominal periaortitis, over half had radiographic improvement but resolution was uncommon. Older age at diagnosis and presence of secondary cause were associated with increased likelihood of resolution. Smokers had two times lower likelihood of radiographic resolution. Two-thirds were able to achieve permanent ureteral stent extraction. Among patients without baseline aneurysm, subsequent development is rare. Treatment regimens were variable. Prospective studies are needed to determine which medications led to optimal outcomes.
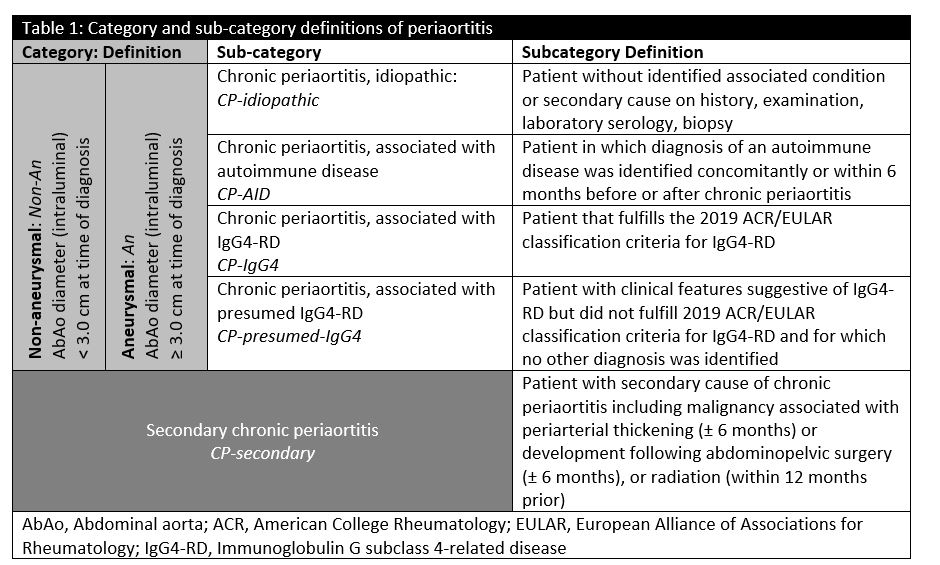 Table 1: Category and sub-category definitions of periaortitis
Table 1: Category and sub-category definitions of periaortitis
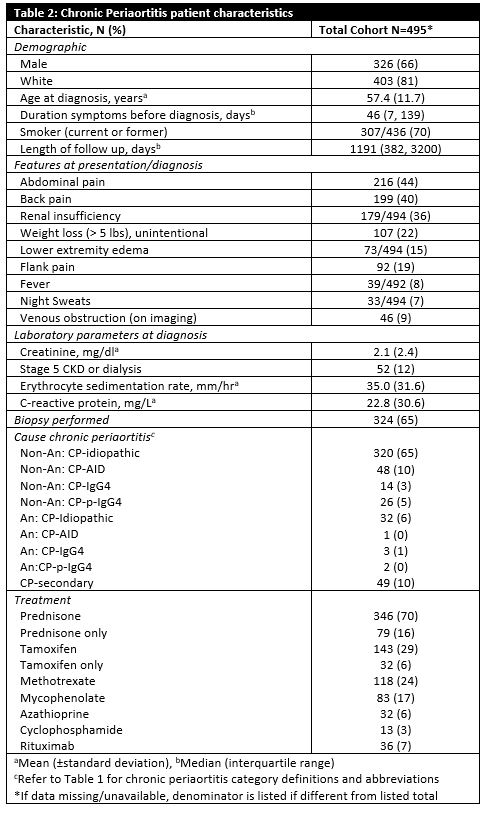 Table 2: Chronic Periaortitis patient characteristics
Table 2: Chronic Periaortitis patient characteristics
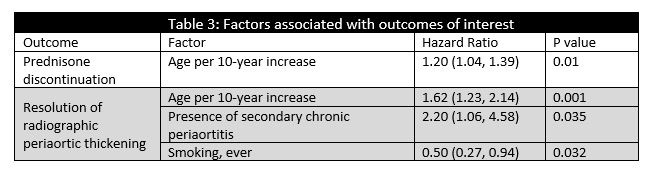 Table 3: Factors associated with outcomes of interest
Table 3: Factors associated with outcomes of interest
Disclosures: U. Ghaffar, None; H. Langenfeld, None; C. Crowson, None; T. Kermani, None; M. Burke, None; B. Viers, None; A. Potretzke, None; H. Bjarnason, None; K. Warrington, Eli Lilly, GlaxoSmithKlein(GSK), Kiniksa, Chemocentryx; M. Koster, None.
Background/Purpose: To evaluate the presentation features and outcomes of patients with chronic abdominal periaortitis in a large referral cohort.
Methods: Using a proprietary medical text search algorithm, all patients from 1/1/1996 to 12/31/2019 with mention of 'periaortitis,' 'periaortic soft tissue,' or 'retroperitoneal fibrosis' in the medical chart were screened. Patients with radiographic confirmation of infra-renal abdominal aorta (irAbAo) periaortitis were included. Cases with soft tissue thickening elsewhere were excluded unless they had concomitant irAbAo periaortitis. Patients were further characterized based on presence/absence of aneurysm and associated conditions (Table 1). Cox models were used to examine associations between patient characteristics and outcomes.
Results: 2,507 charts were manually reviewed and 495 patients were identified: 326 (66%) male, 403 (81%) white and 70% (307/436) current or former smokers (Table 2). Mean (SD) age at diagnosis was 57.4 (11.7) years. Most common features at presentation included abdominal pain (44%), back pain (40%), renal insufficiency (36%). End-stage renal disease (ESRD) was present in 52 (12%) at diagnosis. Ureteral stents were placed in 236 (48%): unilateral (n=93), bilateral (n=143). Percutaneous nephrostomy tubes were used in 50 patients, 20 due to stent failure or pain. Treatments utilized are listed in Table 2. Prednisone was given in 346 (70%); 79 as monotherapy. The most common steroid-sparing treatments included tamoxifen, methotrexate, and mycophenolate. At last visit, 160 patients were still on prednisone, 57 on tamoxifen and 129 on other immunosuppressive medication. Repeat imaging was available in 455 patients which showed resolution of periaortic thickening in 40 (9%), improvement in 261 (57%), no change in 103 (23%), and worsening in 51 (11%). Of 212 patients with stents and follow-up data, 141 had successful permanent removal. Of patients with nephrostomy tubes, 33 had permanent removal. Compared to baseline, renal function stage at last follow up was improved in 39%, worse in 19% and stayed the same in 42%. Only one patient without ESRD at baseline developed ESRD by last follow-up. Of those with non-aneurysmal irAbAo periaortitis at baseline, only 8% developed aneurysm after presentation. For patients with aneurysm at diagnosis, 14 had intervention, 2 had AbAo rupture. No evaluated factors were associated with likelihood of ureteral stent removal. Factors significantly associated with prednisone discontinuation and radiographic resolution are listed in Table 3.
Conclusion: In this large cohort of patients with chronic abdominal periaortitis, over half had radiographic improvement but resolution was uncommon. Older age at diagnosis and presence of secondary cause were associated with increased likelihood of resolution. Smokers had two times lower likelihood of radiographic resolution. Two-thirds were able to achieve permanent ureteral stent extraction. Among patients without baseline aneurysm, subsequent development is rare. Treatment regimens were variable. Prospective studies are needed to determine which medications led to optimal outcomes.
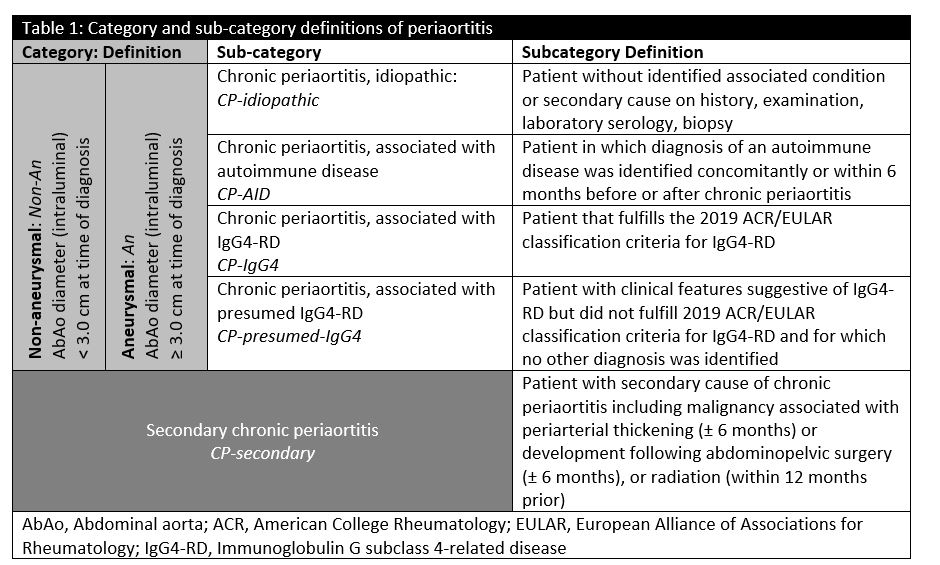 Table 1: Category and sub-category definitions of periaortitis
Table 1: Category and sub-category definitions of periaortitis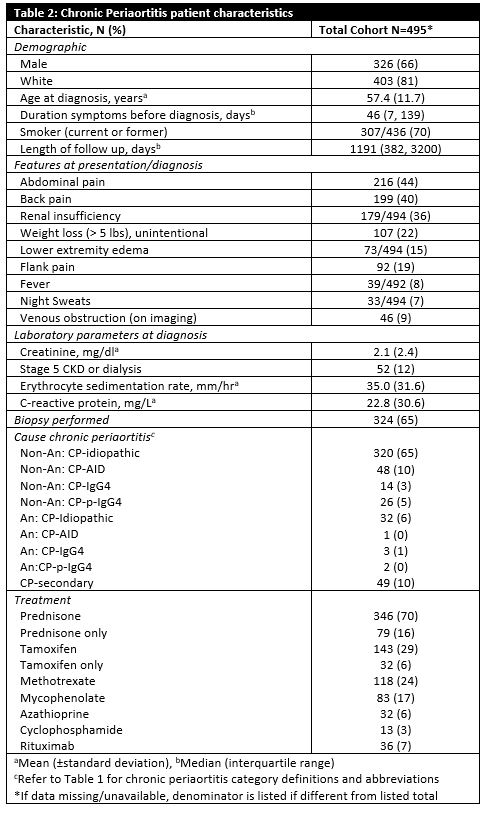 Table 2: Chronic Periaortitis patient characteristics
Table 2: Chronic Periaortitis patient characteristics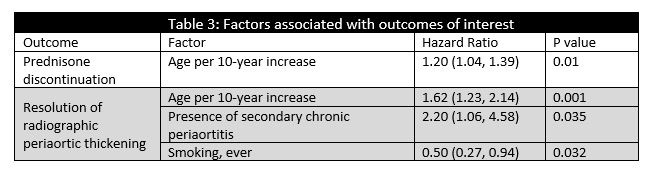 Table 3: Factors associated with outcomes of interest
Table 3: Factors associated with outcomes of interestDisclosures: U. Ghaffar, None; H. Langenfeld, None; C. Crowson, None; T. Kermani, None; M. Burke, None; B. Viers, None; A. Potretzke, None; H. Bjarnason, None; K. Warrington, Eli Lilly, GlaxoSmithKlein(GSK), Kiniksa, Chemocentryx; M. Koster, None.

