Back
Abstract Session
Systemic lupus erythematosus (SLE)
Session: Abstracts: SLE – Treatment (1651–1656)
1652: Long-term Safety and Efficacy of Anifrolumab in Adult Patients with Systemic Lupus Erythematosus: A Multicenter, Randomized, Double-blind, Placebo-controlled 3-year TULIP Extension Study
Monday, November 14, 2022
9:15 AM – 9:25 AM Eastern Time
Location: Room 113
- KK
Kenneth C. Kalunian, MD, FACR
UC San Diego
La Jolla, CA, United States
Presenting Author(s)
Kenneth C. Kalunian1, Richard A. Furie2, Eric F. Morand3, Ian N. Bruce4, Susan Manzi5, Yoshiya Tanaka6, Kevin Winthrop7, Gabriel Abreu8, Ihor Hupka9, Lijin Zhang10, Shanti Werther11, Micki Hultquist12, Raj Tummala10 and Catharina Lindholm11, 1UC San Diego, La Jolla, CA, 2Northwell Health, Great Neck, NY, 3Monash University, Melbourne, Australia, 4The University of Manchester, Manchester, United Kingdom, 5Allegheny Health Network, Pittsburgh, PA, 6University of Occupational and Environmental Health, Kitakyusyu Fukuoka, Japan, 7Oregon Health & Science University, Portland, OR, 8AstraZeneca, Mölndal, Sweden, 9AstraZeneca, Warsaw, Poland, 10AstraZeneca, Gaithersburg, MD, 11AstraZeneca, Gothenburg, Sweden, 12AstraZeneca, Bethesda, MD
Background/Purpose: Anifrolumab is a fully human IgG1 κ monoclonal antibody that binds to the type I IFN receptor and inhibits type I IFN signaling.1 In the phase 3, randomized, double-blind, placebo-controlled TULIP-1 (NCT02446912)2 and TULIP-2 (NCT02446899)3 trials, demonstration of a favorable benefit–risk profile led to approval of anifrolumab in several countries for patients with moderate to severe SLE receiving standard therapy. Thus, understanding long-term safety and efficacy is essential. Described here are long-term safety and efficacy results of anifrolumab 300 mg vs placebo in patients who completed one year in a phase 3 TULIP trial, plus up to 3 years of participation in the TULIP long-term extension (LTE) study (NCT02794285).
Methods: Eligible patients completed TULIP-1 or TULIP-2 through Week 52 and met all LTE eligibility criteria. In addition to standard therapy, adults received intravenous anifrolumab 300 mg or placebo every 4 weeks for up to 39 doses in the blinded LTE study. Rates of adverse events (AEs), serious AEs (SAEs) including deaths, AEs leading to discontinuation (DAEs), AEs of special interest (AESIs) and laboratory variables were evaluated. Event rates were adjusted for exposure (EAIR) and standardized per 100 patient years. Safety data for patients randomized to anifrolumab 300 mg in the TULIP trials and continuing in the LTE, and those randomized to placebo in all 3 studies, were summarized by descriptive statistics. Exploratory efficacy outcomes included SLEDAI-2K.
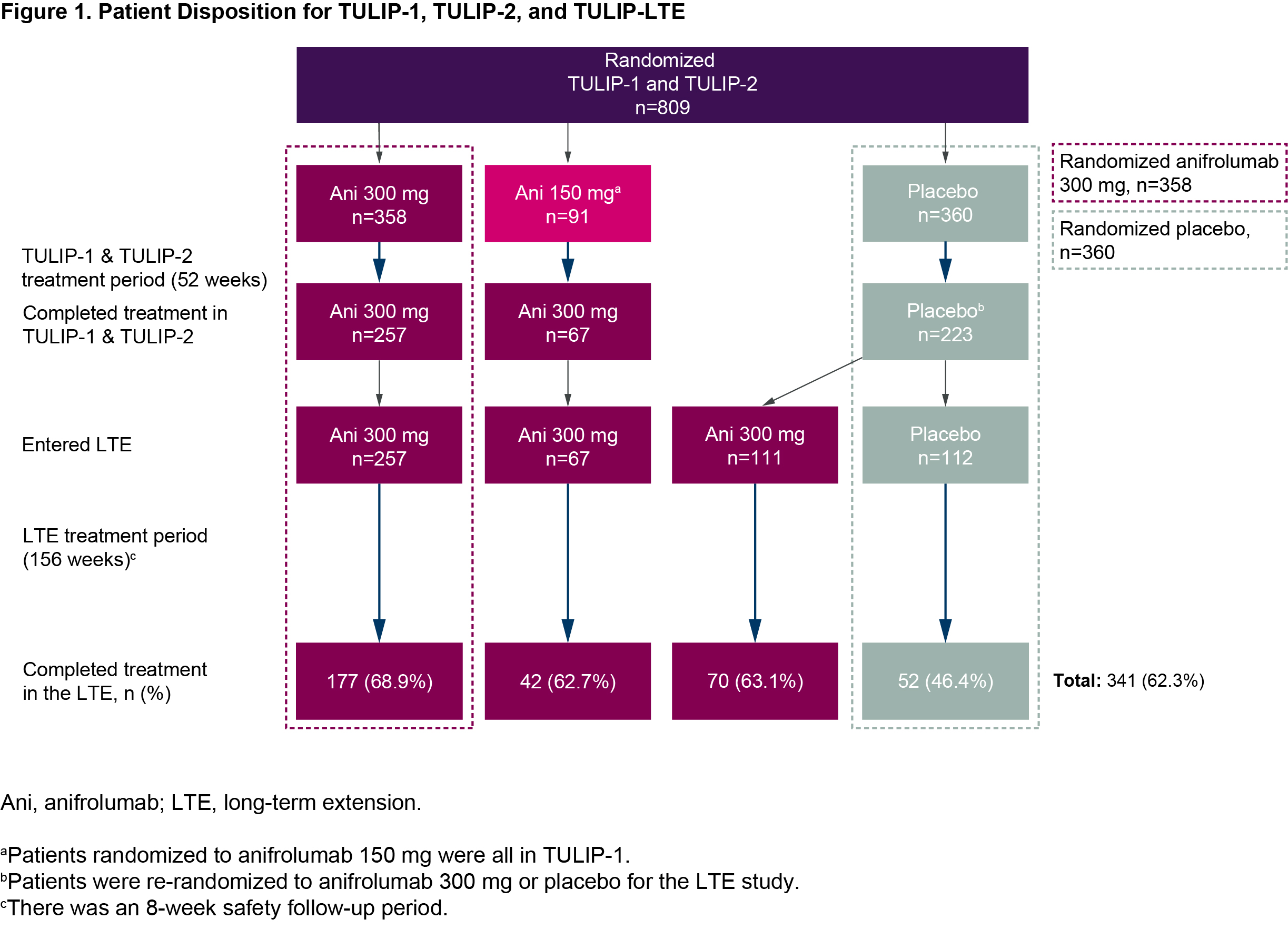
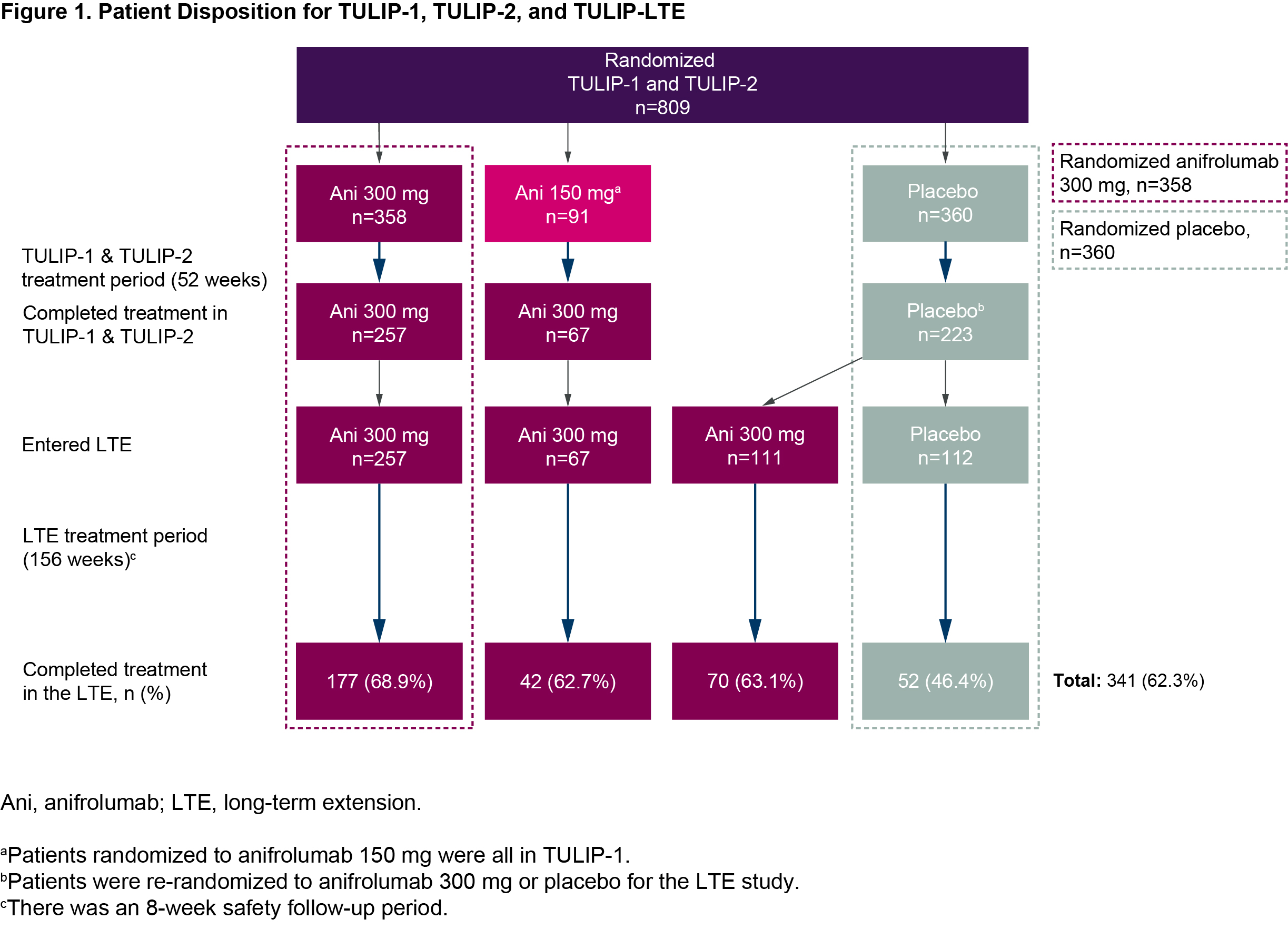
Results: Of 662 patients who completed treatment and the Week 52 visit of TULIP-1 or TULIP-2, 547 enrolled and received at least one treatment dose in the LTE (Figure 1). Along with 257 patients who continued anifrolumab 300 mg, 67 patients transitioned from anifrolumab 150 mg to 300 mg. The 223 patients who received placebo in TULIP-1 or TULIP-2 were re-randomized 1:1 to anifrolumab 300 mg (111 patients) or placebo (112 patients) in the LTE. Treatment was completed by 341 (62%) patients (69% anifrolumab 300 mg, 46% placebo). Frequency and rate of any AEs during the LTE were similar between patients treated with anifrolumab 300 mg or placebo through TULIP-1 and TULIP-2 (Table). EAIRs per 100 patient years of any SAEs, including deaths, were 8.5 for anifrolumab and 11.2 for placebo. EAIRs per 100 patient years were generally similar between groups (anifrolumab vs placebo) for DAEs (2.5 vs 3.2), and for AESI of serious infections (3.7 vs 3.6) and herpes zoster (3.4 vs 2.8). There were no cases of active tuberculosis or anaphylaxis. Rates of malignancy were low, and EAIRs similar, in both groups. Patients who received anifrolumab 300 mg had greater mean improvement in SLEDAI-2K with continued improvement over time (Figure 2).
Conclusion: The favorable benefit–risk profile for anifrolumab compared with placebo in patients with moderate to severe SLE receiving standard therapy was maintained throughout the 3-year LTE of the TULIP trials.
References:
1. Riggs JM. Lupus Sci Med. 2018;5:e000261.
2. Furie RA. Lancet Rheumatol. 2019;1:e208-e19.
3. Morand EF. N Engl J Med. 2020;382:211-21.
.jpg)
.jpg)
Disclosures: K. Kalunian, AstraZeneca; R. Furie, AstraZeneca, Biogen; E. Morand, AbbVie, Amgen, AstraZeneca, Biogen, BristolMyersSquibb, Eli Lilly, Genentech, GlaxoSmithKline, Janssen, Novartis, Servier, UCB, EMD Soreno; I. Bruce, AstraZeneca, GlaxoSmithKline, Janssen, Eli Lilly, UCB; S. Manzi, AstraZeneca, Abbvie, Cugene, GlaxoSmithKline, Lilly, Lupus Foundation of America, UCB Advisory Board; Y. Tanaka, Behringer Ingelheim, Eli Lilly, Abbvie, Gilead, AstraZeneca, Bristol-Myers, Chugai, Daiichi-Sankyo, Eisai, Pfizer, Mitsubishi-Tanabe, GlaxoSmithKline, Asahi-Kasei; K. Winthrop, Pfizer, BMS, Abbvie, UCB, Eli Lilly, Galapagos, GlaxoSmithKline, Roche, Gilead, Regeneron, Sanofi, AstraZeneca, Novartis; G. Abreu, AstraZeneca; I. Hupka, AstraZeneca; L. Zhang, AstraZeneca; S. Werther, AstraZeneca; M. Hultquist, AstraZeneca; R. Tummala, AstraZeneca; C. Lindholm, AstraZeneca.
Background/Purpose: Anifrolumab is a fully human IgG1 κ monoclonal antibody that binds to the type I IFN receptor and inhibits type I IFN signaling.1 In the phase 3, randomized, double-blind, placebo-controlled TULIP-1 (NCT02446912)2 and TULIP-2 (NCT02446899)3 trials, demonstration of a favorable benefit–risk profile led to approval of anifrolumab in several countries for patients with moderate to severe SLE receiving standard therapy. Thus, understanding long-term safety and efficacy is essential. Described here are long-term safety and efficacy results of anifrolumab 300 mg vs placebo in patients who completed one year in a phase 3 TULIP trial, plus up to 3 years of participation in the TULIP long-term extension (LTE) study (NCT02794285).
Methods: Eligible patients completed TULIP-1 or TULIP-2 through Week 52 and met all LTE eligibility criteria. In addition to standard therapy, adults received intravenous anifrolumab 300 mg or placebo every 4 weeks for up to 39 doses in the blinded LTE study. Rates of adverse events (AEs), serious AEs (SAEs) including deaths, AEs leading to discontinuation (DAEs), AEs of special interest (AESIs) and laboratory variables were evaluated. Event rates were adjusted for exposure (EAIR) and standardized per 100 patient years. Safety data for patients randomized to anifrolumab 300 mg in the TULIP trials and continuing in the LTE, and those randomized to placebo in all 3 studies, were summarized by descriptive statistics. Exploratory efficacy outcomes included SLEDAI-2K.
Results: Of 662 patients who completed treatment and the Week 52 visit of TULIP-1 or TULIP-2, 547 enrolled and received at least one treatment dose in the LTE (Figure 1). Along with 257 patients who continued anifrolumab 300 mg, 67 patients transitioned from anifrolumab 150 mg to 300 mg. The 223 patients who received placebo in TULIP-1 or TULIP-2 were re-randomized 1:1 to anifrolumab 300 mg (111 patients) or placebo (112 patients) in the LTE. Treatment was completed by 341 (62%) patients (69% anifrolumab 300 mg, 46% placebo). Frequency and rate of any AEs during the LTE were similar between patients treated with anifrolumab 300 mg or placebo through TULIP-1 and TULIP-2 (Table). EAIRs per 100 patient years of any SAEs, including deaths, were 8.5 for anifrolumab and 11.2 for placebo. EAIRs per 100 patient years were generally similar between groups (anifrolumab vs placebo) for DAEs (2.5 vs 3.2), and for AESI of serious infections (3.7 vs 3.6) and herpes zoster (3.4 vs 2.8). There were no cases of active tuberculosis or anaphylaxis. Rates of malignancy were low, and EAIRs similar, in both groups. Patients who received anifrolumab 300 mg had greater mean improvement in SLEDAI-2K with continued improvement over time (Figure 2).
Conclusion: The favorable benefit–risk profile for anifrolumab compared with placebo in patients with moderate to severe SLE receiving standard therapy was maintained throughout the 3-year LTE of the TULIP trials.
References:
1. Riggs JM. Lupus Sci Med. 2018;5:e000261.
2. Furie RA. Lancet Rheumatol. 2019;1:e208-e19.
3. Morand EF. N Engl J Med. 2020;382:211-21.
.jpg)
.jpg)
Disclosures: K. Kalunian, AstraZeneca; R. Furie, AstraZeneca, Biogen; E. Morand, AbbVie, Amgen, AstraZeneca, Biogen, BristolMyersSquibb, Eli Lilly, Genentech, GlaxoSmithKline, Janssen, Novartis, Servier, UCB, EMD Soreno; I. Bruce, AstraZeneca, GlaxoSmithKline, Janssen, Eli Lilly, UCB; S. Manzi, AstraZeneca, Abbvie, Cugene, GlaxoSmithKline, Lilly, Lupus Foundation of America, UCB Advisory Board; Y. Tanaka, Behringer Ingelheim, Eli Lilly, Abbvie, Gilead, AstraZeneca, Bristol-Myers, Chugai, Daiichi-Sankyo, Eisai, Pfizer, Mitsubishi-Tanabe, GlaxoSmithKline, Asahi-Kasei; K. Winthrop, Pfizer, BMS, Abbvie, UCB, Eli Lilly, Galapagos, GlaxoSmithKline, Roche, Gilead, Regeneron, Sanofi, AstraZeneca, Novartis; G. Abreu, AstraZeneca; I. Hupka, AstraZeneca; L. Zhang, AstraZeneca; S. Werther, AstraZeneca; M. Hultquist, AstraZeneca; R. Tummala, AstraZeneca; C. Lindholm, AstraZeneca.

