Back
Poster Session D
Epidemiology, health policy and outcomes
Session: (1750–1786) Epidemiology and Public Health Poster III
1770: Prevalence and Incidence of Depression in Patients with Rheumatoid Arthritis: A Systematic Review
Monday, November 14, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- GR
Griffin Reed, MD
Rhode island hospital
Providence, RI, United States
Abstract Poster Presenter(s)
John E Oghene1, Griffin Reed2, Ian Saldanha3, Pooja Reddy4, Ahmed Elshazly5, Yuvaraj Singh6 and Deepan Dalal7, 1Hospital of the University of Pennsylvania, Philadelphia, PA, 2Rhode island hospital, Brown University Warren Alpert School of Medicine, Providence, RI, 3Brown University School of Public Health, Providence, RI, 4Rhode island hospital, Brown University Warren Alpert School of Medicine, Seekonk, MA, 5Westerly Hospital, Yale New Haven Health, Westerly, RI, 6Saint Vincent Hospital, Worcester, MA, 7Brown University School of Medicine, Providence, RI
Background/Purpose: Depression is a common co-morbidity that has been shown to worsen symptoms such as pain, fatigue, decreased functional status, decreased disease remission, and response to therapy, and increases health care expenses by approximately 7% compared to non-depressed patients with rheumatoid arthritis. While the rates of depression have been reported in several epidemiologic studies, to calculate a more robust determination of the incidence and prevalence rates, we conducted a systematic review of all clinical trials and observational studies. This will help inform clinicians on appropriate screening and treatment of depression in patients with RA.
Methods: We searched Medline, Embase, Web of Science Core Collection, CINAHL, PsycInfo, and the Cochrane Central Register of Controlled Trials (CENTRAL) for cross-sectional or longitudinal studies that reported the incidence or prevalence of depression in patients with RA. All searches were run on June 18-19, 2020. Outcomes of interest were incidence or prevalence of any depression or moderate-to-severe depression according to any scale or specifically the most common scales: Hospital Anxiety and Depression Scale (HADS), Self-rating Depression Scale (SDS), Beck Depression Inventory (BDI), Patient Health Questionnaire (PHQ-9), Center for Epidemiological Studies Depression Scale (CESD), International Classification of Diseases (ICD) codes, or Diagnostic and Statistical Manual (DSM) criteria. For each outcome, we summarized the median and interquartile range (IQR) of the estimates across studies.
Results: Our search yielded 10,257 unique records, of which we screened 1,202 full-text articles. We included 154 studies that enrolled 905,154 patients with RA between 1979 and 2019. Studies were conducted all over the world but were most frequently in the U.S. (n=49 studies), U.K. (n=12), Canada (n=6), and Germany (n=6). Most studies (151/154; 98%) were in the outpatient setting. Most studies (120/154; 80%) were cross-sectional or reported on baseline disease prevalence only. Additionally, 34 longitudinal studies with follow-up durations of 0.5 to 10 years reported the incidence of depression. The prevalent outcome of any depression was reported by 137 studies, with a median prevalence of 26.5% [IQR 14.7%, 42.0%] and a median incidence over 0.5 to 4.6 years of 12.1% [IQR 7.6%, 17.8%] (Table 1). The outcome of moderate-to-severe depression was reported by 45 studies, with a median prevalence of 22.6% [IQR 14.2%, 30.5%] and an incidence over 2 years of 8.0% (one study).
Conclusion: Our data revealed a high prevalence and incidence of depression in patients with RA. Estimates of the prevalence of depression varied based on the depression scale used, however, these estimates are two to three times higher than in the general population. In clinical practice, early recognition and effective management of depression in patients with RA may improve their adherence to RA treatment plans and prolong disease remission. Ultimately, for rheumatologists to optimize the outcomes of their patients with RA, ensuring the adequate treatment of a patient's depression may be an important new responsibility.
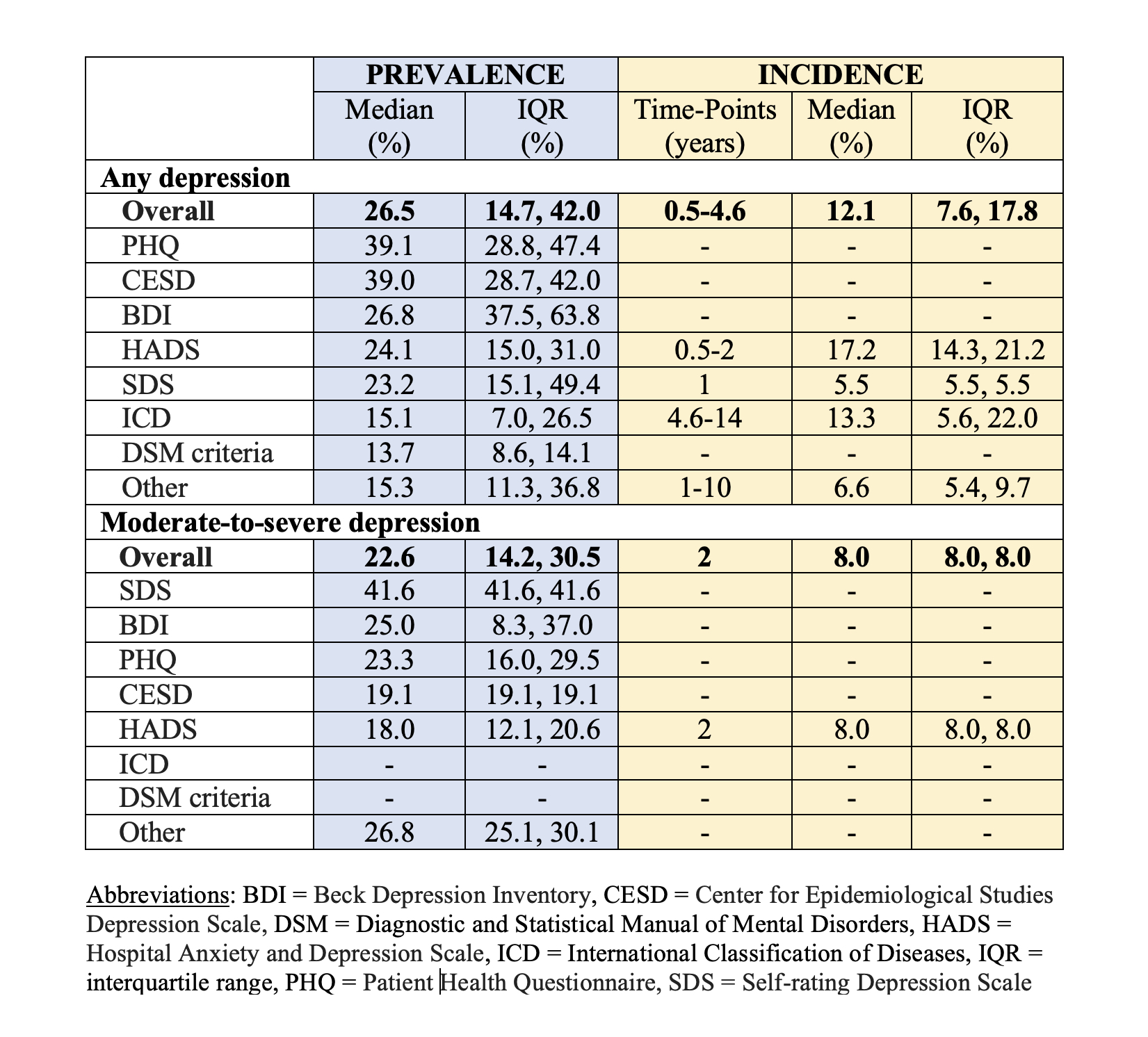 Table 1: Median and interquartile ranges of estimates of prevalence and incidence of any depression and moderate-to-severe depression across included studies of patients with rheumatoid arthritis.
Table 1: Median and interquartile ranges of estimates of prevalence and incidence of any depression and moderate-to-severe depression across included studies of patients with rheumatoid arthritis.
Disclosures: J. Oghene, None; G. Reed, None; I. Saldanha, None; P. Reddy, None; A. Elshazly, None; Y. Singh, None; D. Dalal, None.
Background/Purpose: Depression is a common co-morbidity that has been shown to worsen symptoms such as pain, fatigue, decreased functional status, decreased disease remission, and response to therapy, and increases health care expenses by approximately 7% compared to non-depressed patients with rheumatoid arthritis. While the rates of depression have been reported in several epidemiologic studies, to calculate a more robust determination of the incidence and prevalence rates, we conducted a systematic review of all clinical trials and observational studies. This will help inform clinicians on appropriate screening and treatment of depression in patients with RA.
Methods: We searched Medline, Embase, Web of Science Core Collection, CINAHL, PsycInfo, and the Cochrane Central Register of Controlled Trials (CENTRAL) for cross-sectional or longitudinal studies that reported the incidence or prevalence of depression in patients with RA. All searches were run on June 18-19, 2020. Outcomes of interest were incidence or prevalence of any depression or moderate-to-severe depression according to any scale or specifically the most common scales: Hospital Anxiety and Depression Scale (HADS), Self-rating Depression Scale (SDS), Beck Depression Inventory (BDI), Patient Health Questionnaire (PHQ-9), Center for Epidemiological Studies Depression Scale (CESD), International Classification of Diseases (ICD) codes, or Diagnostic and Statistical Manual (DSM) criteria. For each outcome, we summarized the median and interquartile range (IQR) of the estimates across studies.
Results: Our search yielded 10,257 unique records, of which we screened 1,202 full-text articles. We included 154 studies that enrolled 905,154 patients with RA between 1979 and 2019. Studies were conducted all over the world but were most frequently in the U.S. (n=49 studies), U.K. (n=12), Canada (n=6), and Germany (n=6). Most studies (151/154; 98%) were in the outpatient setting. Most studies (120/154; 80%) were cross-sectional or reported on baseline disease prevalence only. Additionally, 34 longitudinal studies with follow-up durations of 0.5 to 10 years reported the incidence of depression. The prevalent outcome of any depression was reported by 137 studies, with a median prevalence of 26.5% [IQR 14.7%, 42.0%] and a median incidence over 0.5 to 4.6 years of 12.1% [IQR 7.6%, 17.8%] (Table 1). The outcome of moderate-to-severe depression was reported by 45 studies, with a median prevalence of 22.6% [IQR 14.2%, 30.5%] and an incidence over 2 years of 8.0% (one study).
Conclusion: Our data revealed a high prevalence and incidence of depression in patients with RA. Estimates of the prevalence of depression varied based on the depression scale used, however, these estimates are two to three times higher than in the general population. In clinical practice, early recognition and effective management of depression in patients with RA may improve their adherence to RA treatment plans and prolong disease remission. Ultimately, for rheumatologists to optimize the outcomes of their patients with RA, ensuring the adequate treatment of a patient's depression may be an important new responsibility.
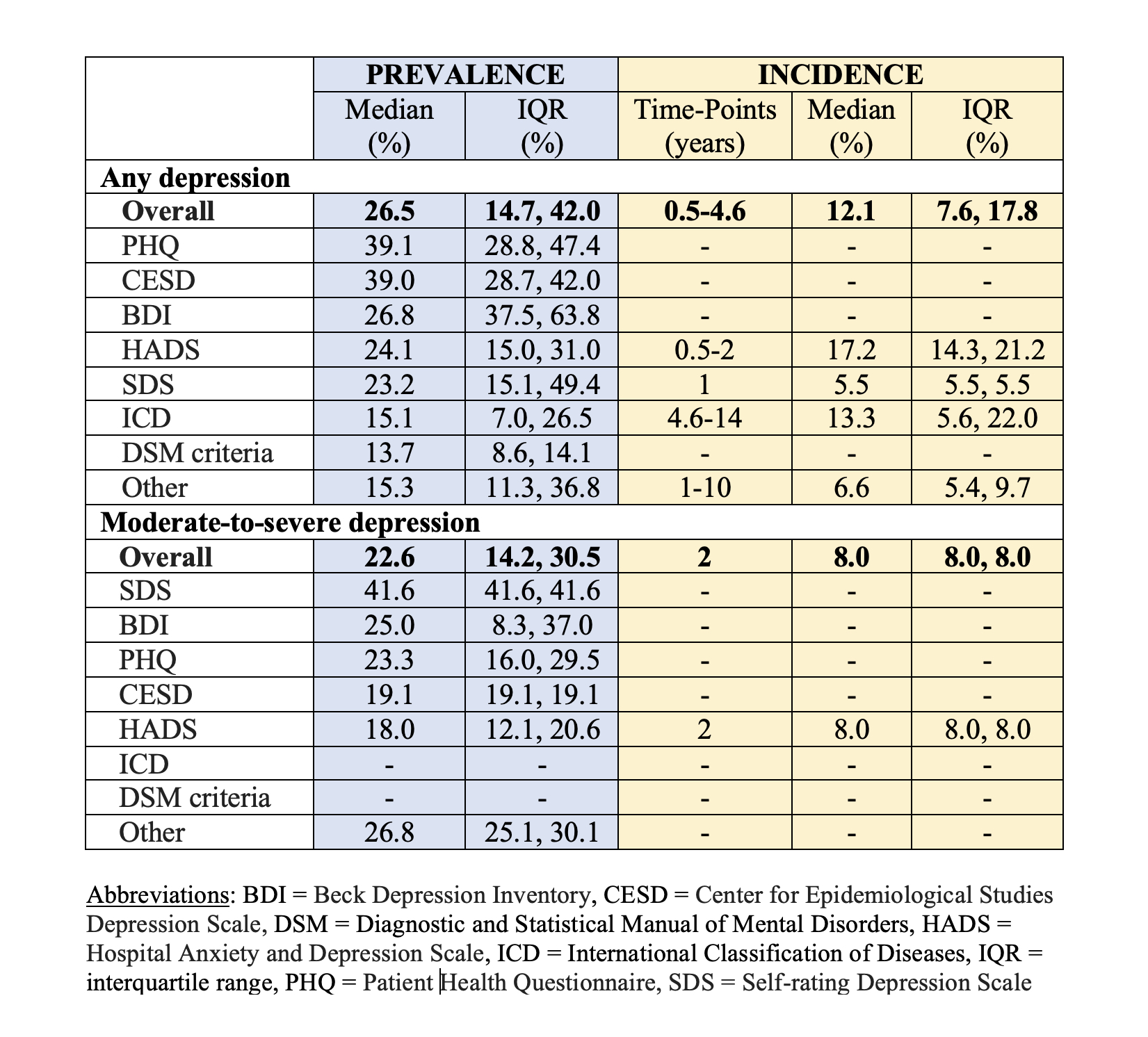 Table 1: Median and interquartile ranges of estimates of prevalence and incidence of any depression and moderate-to-severe depression across included studies of patients with rheumatoid arthritis.
Table 1: Median and interquartile ranges of estimates of prevalence and incidence of any depression and moderate-to-severe depression across included studies of patients with rheumatoid arthritis.Disclosures: J. Oghene, None; G. Reed, None; I. Saldanha, None; P. Reddy, None; A. Elshazly, None; Y. Singh, None; D. Dalal, None.

