Back
Poster Session D
Myopathic rheumatic diseases (polymyositis, dermatomyositis, inclusion body myositis)
Session: (1856–1887) Muscle Biology, Myositis and Myopathies Poster II
1864: Hepatitis B Exposure and Infection in Idiopathic Inflammatory Myopathies: Prevalence, Presentation, and Treatment Response
Monday, November 14, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- AV
Ana Valle, MD, MHS
Montefiore Medical Center
New York, NY, United States
Abstract Poster Presenter(s)
Ana Valle1, Xianhong Xie2 and Shereen Mahmood3, 1Montefiore Medical Center, New York, NY, 2Department of Epidemiology & Population Health/Albert Einstein College of Medicine, Bronx, NY, 3Albert Einstein College of Medicine/Montefiore Medical Center, New York, NY
Background/Purpose: Hepatitis B (HBV) screening in patients with autoimmune conditions is vital prior to the initiation of immunosuppressive therapy given the risk of HBV reactivation. Most studies have evaluated rheumatoid arthritis patients and generalized their findings to other rheumatic diseases. Yet, little is known about the prevalence of HBV exposure and infection in patients with idiopathic inflammatory myopathies (IIM). Moreover, extra-hepatic manifestations of HBV infections include myopathy and cutaneous findings which mimic IIM. Our aim was to describe the prevalence of HBV exposure, infection, and prophylaxis in patients with IIM and to compare myositis disease course, organ involvement, and treatment response between IIM patients with and without HBV.
Methods: A registry was created of Montefiore Medical Center patients that met 2017 EULAR/ACR classification criteria for IIM. Demographics, IIM type, antibodies, clinical manifestations, comorbidities, and treatment history were documented. HBV core antibody, surface antigen, viral load, and prescribed HBV antivirals were noted. Medication failure was defined by rheumatologist, discontinuation due to adverse effects, or medication change within 3 months. Medication control was defined by documented clinical improvement. Statistical analyses included descriptive statistics of patients with HBV, two-sample t-tests, Chi-square tests, and Fisher’s exact tests.
Results: Of 152 patients, 119 (78%) had been screened for HBV (Figure 1). Of those screened, 32 (27%) had the HBV core antibody. Mean screening date was 21 months after the IIM diagnosis. Most IIM patients with HBV core antibody had cleared the infection, but one had evidence of chronic infection based on a persistently elevated viral load. Of the 31 patients with a positive core antibody and without a viral load, one was HBV surface antigen positive. This individual was not on antiviral therapy. Fifteen patients were treated with HBV antiviral therapy, most of whom were in anticipation of or during Rituximab treatment. Yet only 8/11 (73%) patients treated with Rituximab received prophylactic antiviral therapy.
Patients with HBV had a higher frequency of myositis-associated antibodies in comparison to patients without HBV. Patients with HBV were more likely reach IIM remission with IVIG in comparison to patients without HBV (43.8% vs 11.5%, p < 0.01). This difference persisted even when patients who had HBV core antibody positivity after IVIG exposure were removed (40.7% vs 11.5%, p < 0.01). There were no differences in demographics, myositis types, presentation, or comorbidities between the two groups (Figure 2).
Conclusion: Current and past HBV infections are common among IIM patients, even outside of an endemic geographical region. Despite the risk of HBV reactivation with immunosuppression, screening does not occur consistently. Similarly, not all IIM patients at high risk of HBV reactivation receive prophylaxis. It is imperative for providers to familiarize themselves with the most recent ACR guidelines regarding HBV exposure, infection, and prophylaxis in order to minimize the risk of HBV reactivation. Furthermore, IVIG treatment in IIM patients with HBV warrants further investigation.
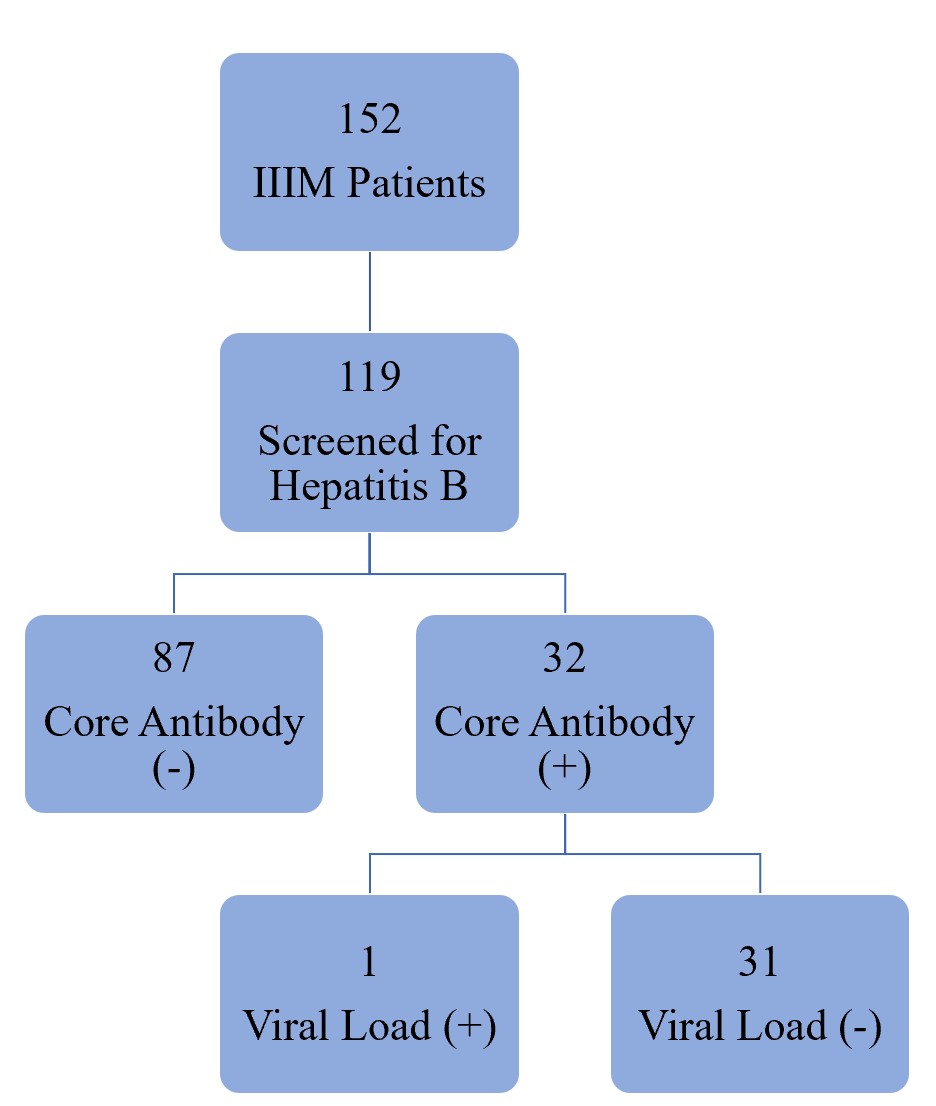 Figure 1. Distribution of active and past HBV infections in IIM patients.
Figure 1. Distribution of active and past HBV infections in IIM patients.
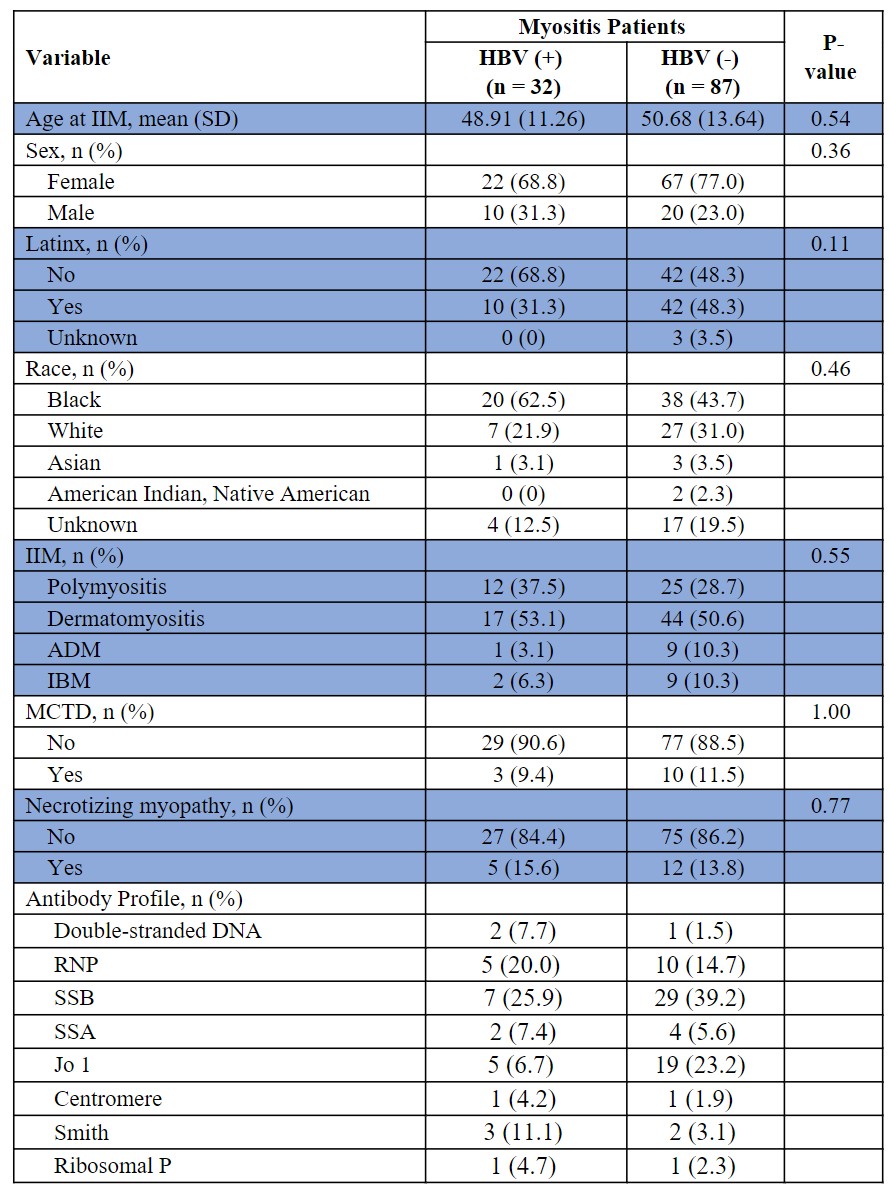 Figure 2. Comparison of demographics, myositis subtypes and antibodies between IIM patients with and without Hepatitis B. Where HBV (+) = Hepatitis B core antibody positive, HBV (-) = Hepatitis B core antibody negative, ADM = amyotrophic dermatomyositis, MCTD = mixed connective tissue disease, IBM = inclusion body myositis, ILD = interstitial lung disease.
Figure 2. Comparison of demographics, myositis subtypes and antibodies between IIM patients with and without Hepatitis B. Where HBV (+) = Hepatitis B core antibody positive, HBV (-) = Hepatitis B core antibody negative, ADM = amyotrophic dermatomyositis, MCTD = mixed connective tissue disease, IBM = inclusion body myositis, ILD = interstitial lung disease.
Disclosures: A. Valle, None; X. Xie, None; S. Mahmood, None.
Background/Purpose: Hepatitis B (HBV) screening in patients with autoimmune conditions is vital prior to the initiation of immunosuppressive therapy given the risk of HBV reactivation. Most studies have evaluated rheumatoid arthritis patients and generalized their findings to other rheumatic diseases. Yet, little is known about the prevalence of HBV exposure and infection in patients with idiopathic inflammatory myopathies (IIM). Moreover, extra-hepatic manifestations of HBV infections include myopathy and cutaneous findings which mimic IIM. Our aim was to describe the prevalence of HBV exposure, infection, and prophylaxis in patients with IIM and to compare myositis disease course, organ involvement, and treatment response between IIM patients with and without HBV.
Methods: A registry was created of Montefiore Medical Center patients that met 2017 EULAR/ACR classification criteria for IIM. Demographics, IIM type, antibodies, clinical manifestations, comorbidities, and treatment history were documented. HBV core antibody, surface antigen, viral load, and prescribed HBV antivirals were noted. Medication failure was defined by rheumatologist, discontinuation due to adverse effects, or medication change within 3 months. Medication control was defined by documented clinical improvement. Statistical analyses included descriptive statistics of patients with HBV, two-sample t-tests, Chi-square tests, and Fisher’s exact tests.
Results: Of 152 patients, 119 (78%) had been screened for HBV (Figure 1). Of those screened, 32 (27%) had the HBV core antibody. Mean screening date was 21 months after the IIM diagnosis. Most IIM patients with HBV core antibody had cleared the infection, but one had evidence of chronic infection based on a persistently elevated viral load. Of the 31 patients with a positive core antibody and without a viral load, one was HBV surface antigen positive. This individual was not on antiviral therapy. Fifteen patients were treated with HBV antiviral therapy, most of whom were in anticipation of or during Rituximab treatment. Yet only 8/11 (73%) patients treated with Rituximab received prophylactic antiviral therapy.
Patients with HBV had a higher frequency of myositis-associated antibodies in comparison to patients without HBV. Patients with HBV were more likely reach IIM remission with IVIG in comparison to patients without HBV (43.8% vs 11.5%, p < 0.01). This difference persisted even when patients who had HBV core antibody positivity after IVIG exposure were removed (40.7% vs 11.5%, p < 0.01). There were no differences in demographics, myositis types, presentation, or comorbidities between the two groups (Figure 2).
Conclusion: Current and past HBV infections are common among IIM patients, even outside of an endemic geographical region. Despite the risk of HBV reactivation with immunosuppression, screening does not occur consistently. Similarly, not all IIM patients at high risk of HBV reactivation receive prophylaxis. It is imperative for providers to familiarize themselves with the most recent ACR guidelines regarding HBV exposure, infection, and prophylaxis in order to minimize the risk of HBV reactivation. Furthermore, IVIG treatment in IIM patients with HBV warrants further investigation.
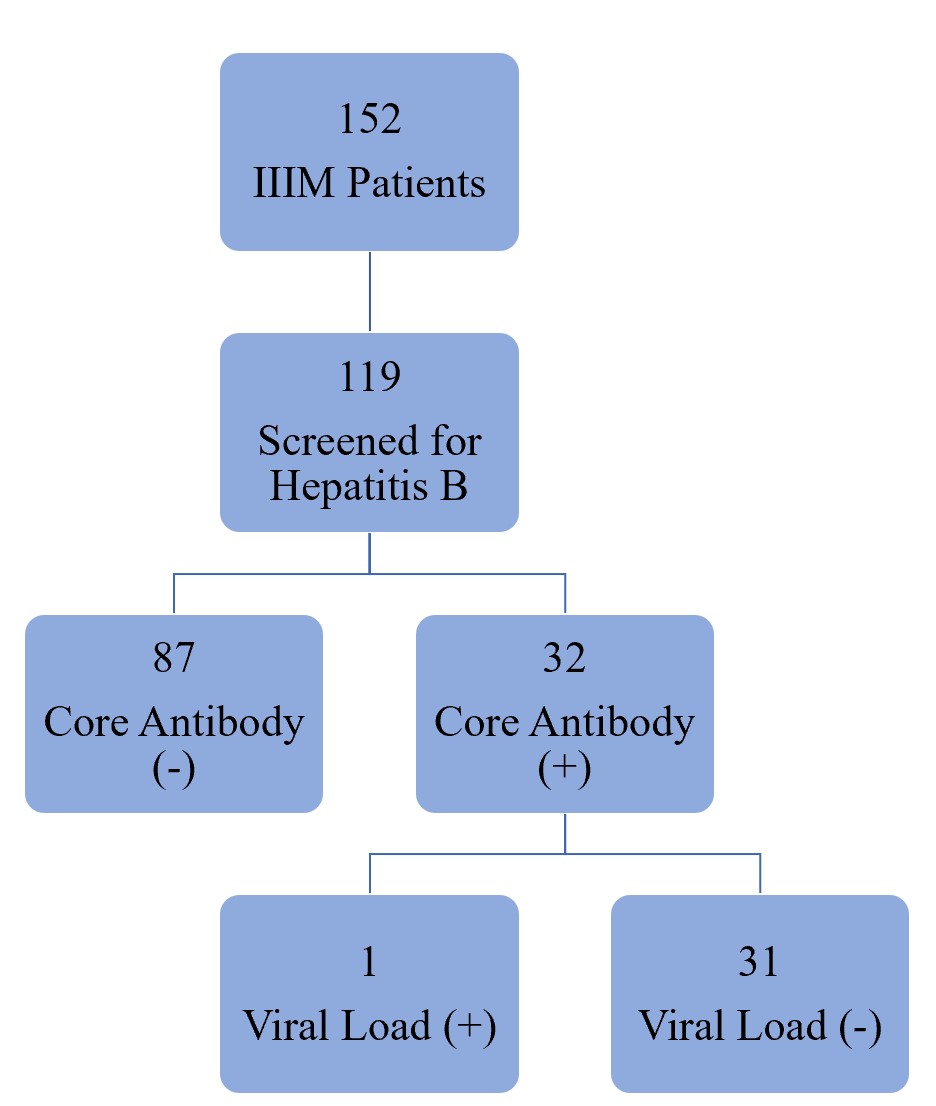 Figure 1. Distribution of active and past HBV infections in IIM patients.
Figure 1. Distribution of active and past HBV infections in IIM patients. 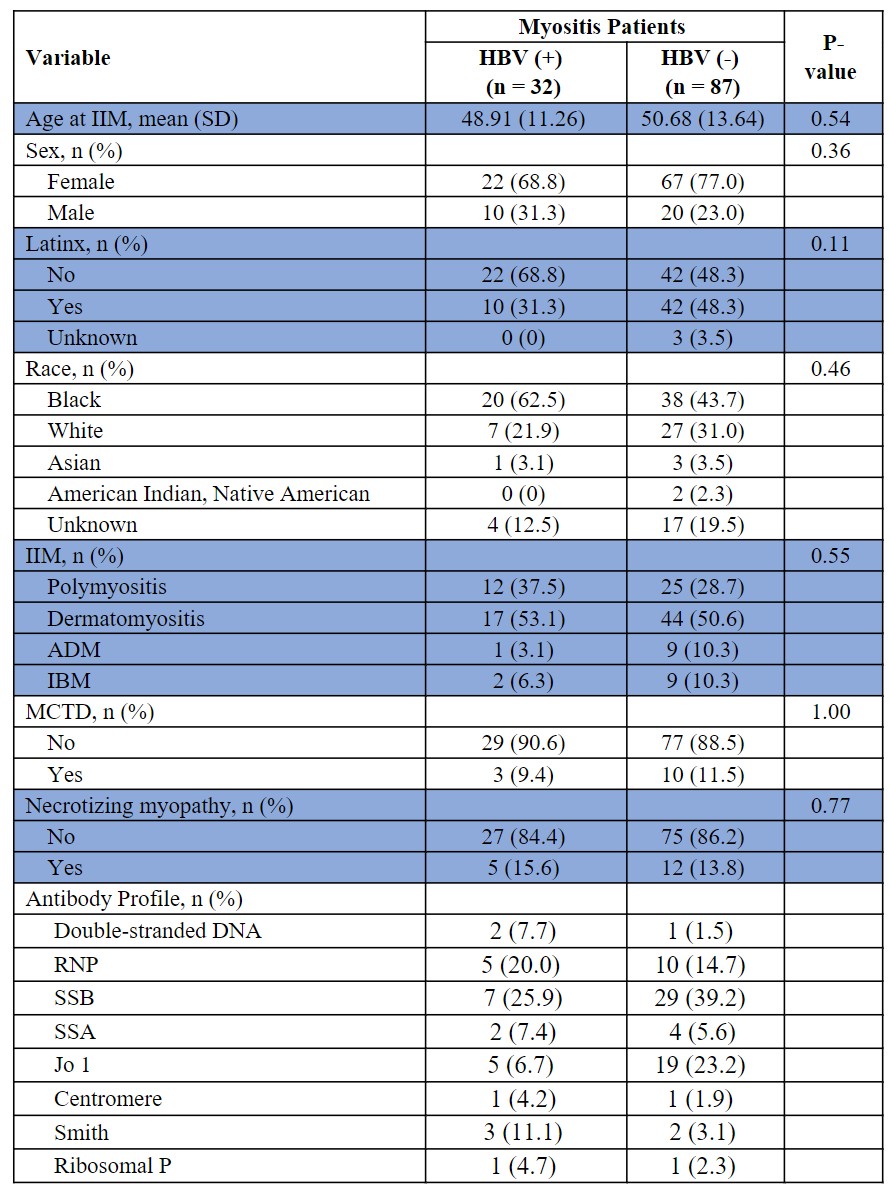 Figure 2. Comparison of demographics, myositis subtypes and antibodies between IIM patients with and without Hepatitis B. Where HBV (+) = Hepatitis B core antibody positive, HBV (-) = Hepatitis B core antibody negative, ADM = amyotrophic dermatomyositis, MCTD = mixed connective tissue disease, IBM = inclusion body myositis, ILD = interstitial lung disease.
Figure 2. Comparison of demographics, myositis subtypes and antibodies between IIM patients with and without Hepatitis B. Where HBV (+) = Hepatitis B core antibody positive, HBV (-) = Hepatitis B core antibody negative, ADM = amyotrophic dermatomyositis, MCTD = mixed connective tissue disease, IBM = inclusion body myositis, ILD = interstitial lung disease. Disclosures: A. Valle, None; X. Xie, None; S. Mahmood, None.

