Back
Poster Session A
Diversity, inclusion and racial disparities
Session: (0085–0122) Healthcare Disparities in Rheumatology Poster
0109: The Impact of Marginalization on Health Outcomes in Childhood-onset Systemic Lupus Erythematosus
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- IM
Ibrahim Mohamed, BSc
The Hospital for Sick Children
Brampton, ON, Canada
Abstract Poster Presenter(s)
Ibrahim Mohamed1, Hardil Bhatt2, Paris Moaf3, Lawrence Ng3, Dragana Ostojic-Aitkens3, Bryan Maguire3, Deborah Levy4, Linda Hiraki5, Alene Toulany6, Chelsea DeCoste7 and Andrea Knight8, 1The Hospital for Sick Children, Neurosciences and Mental Health, Research Institute, ON, Canada 3Institute of Biomedical Engineering, University of Toronto, Brampton, ON, Canada, 2Temerty Faculty of Medicine, Toronto, ON, Canada, 3The Hospital for Sick Children, Toronto, ON, Canada, 4Division of Rheumatology, The Hospital for Sick Children; Child Health Evaluative Services, SickKids Research Institute; Department of Paediatrics, University of Toronto, Toronto, ON, Canada, 5The Hospital for Sick Children, Division of Rheumatology, Department of Paediatrics, University of Toronto, Genetics and Genome Biology, SickKids Research Institute, Toronto, ON, Canada, 6The Hospital for Sick Children, Division of Adolescent Medicine, Department of Paediatrics, University of Toronto,, Toronto, ON, Canada, 7IWK Health Centre, Halifax, NS, Canada, 8The Hospital for Sick Children, Division of Rheumatology, Department of Paediatrics, University of Toronto, Toronto, ON, Canada
Background/Purpose: Adolescents with childhood-onset systemic lupus erythematosus (cSLE) face challenges in managing their disease and mental health. There is increasing evidence that community-level social and economic factors contribute to disparities in health outcomes for marginalized groups, beyond individual-level indicators like income or education. Yet there is limited information on the effects of these community-level factors in cSLE. We sought to investigate the relationship between neighbourhood area-level marginalization and health outcomes in children and adolescents with cSLE.
Methods: We conducted a retrospective cohort study of patients 9-18 years old with cSLE meeting System Lupus International Collaborating Clinics (SLICC) or American College of Rheumatology (ACR) SLE classification criteria and followed in the Lupus Clinic at SickKids between July 2018 and July 2020. The postal codes of patients were linked to the Ontario Marginalization (ON-Marg) Index, a measure derived from the Canadian census to capture health disparities at the area-level. The primary exposures were the four dimensions of the ON-Marg Index: ethnic concentration (concentration of new immigrants and visible minority persons); material deprivation (measure of income, education, single-parent households); residential instability (rates of housing and family instability); and dependency (reflects the population workforce eligibility). Health outcomes included the presence of: i) active disease (adjusted mean SLEDAI score >4) during the study period, ii) disease damage (SLICC/ACR Damage Index score >0) at the latest study visit, and iii) a comorbid psychiatric diagnosis (mood and/or anxiety disorder). We performed univariate and multivariable logistic regression analyses to determine if area-level marginalization was associated with the outcomes, adjusting for age, sex, disease duration, major organ involvement (nephritis and/or central nervous system disease), and glucocorticoid use. Estimates with a p< 0.05 were considered statistically significant.
Results: A total of 184 pediatric patients were included in the study; 29% had active disease, 16% had disease damage, and 18% had a comorbid mood and/or anxiety diagnosis (Table 1). Notably, 61% of patients lived in areas with the highest quintile for ethnic concentration and 46% of patients lived in areas with the lowest quintile for dependency (Figure 1). Those living in areas with higher ethnic concentrations had lower odds of a comorbid psychiatric diagnosis in unadjusted analysis (OR 0.67, 95% CI 0.48-0.94, p=0.021). In adjusted analysis, there were associations between ethnic concentration and lower comorbid psychiatric diagnosis (OR 0.66, 95% CI 0.42-1.04, p=0.073), and dependency with lower active disease (OR 0.56, 95% 0.30-1.04, p=0.066), though not statistically significant (Table 2).
Conclusion: In this sample of patients with cSLE, we found associations between the factors of community-level ethnic concentration and dependency with disease and mental health outcomes. Future studies should explore the patient, provider, and system-level factors influencing medical and psychiatric care among marginalized groups.
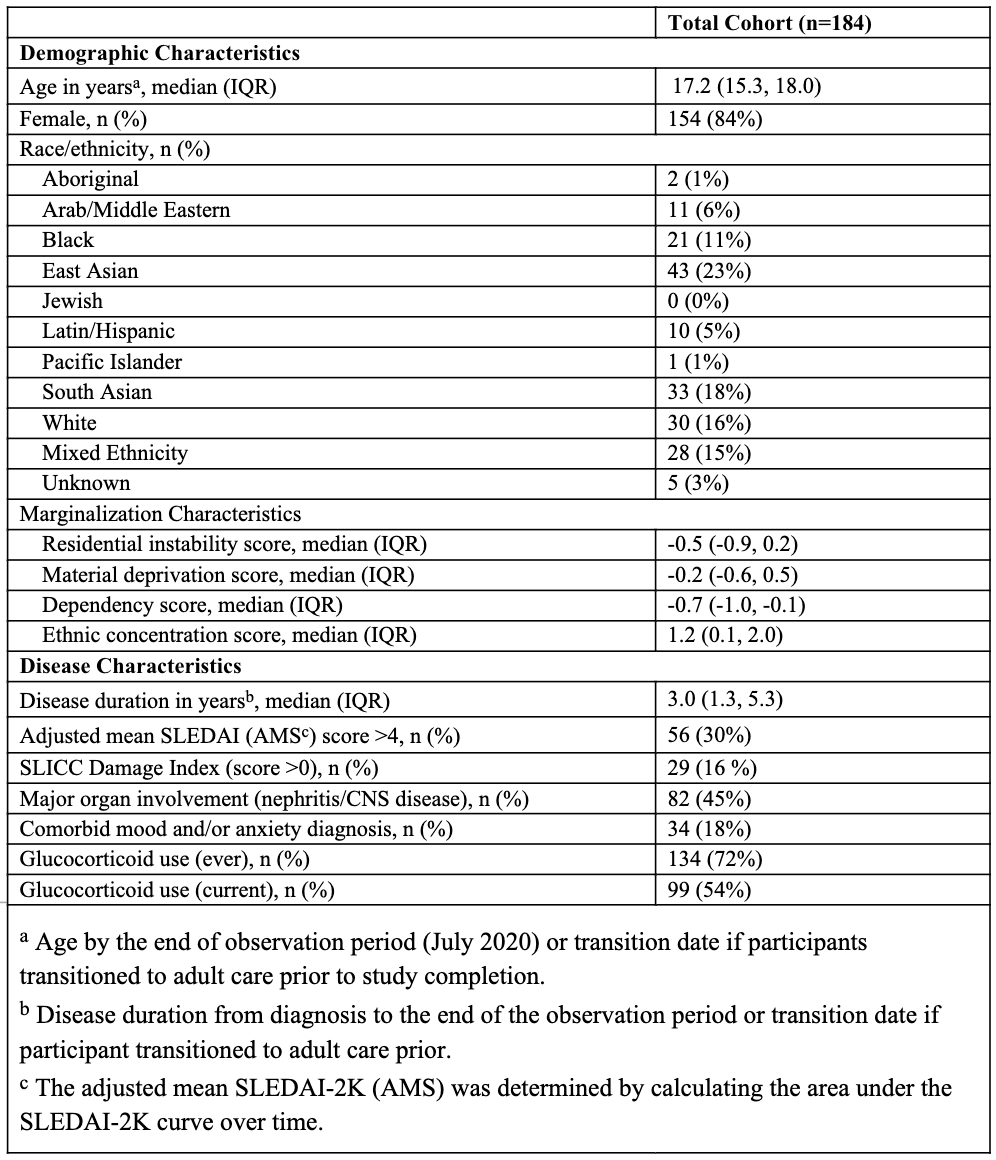 Table 1. Demographics and Disease Characteristics in Children and Adolescent Patients with cSLE.
Table 1. Demographics and Disease Characteristics in Children and Adolescent Patients with cSLE.
.jpeg) Figure 1. Quintile distribution of the Ontario Marginalization Index dimensions in the cSLE cohort (n=184).
Figure 1. Quintile distribution of the Ontario Marginalization Index dimensions in the cSLE cohort (n=184).
.jpeg) Table 2. Results of the adjusted logistic regression analyses for marginalization on the medical and psychiatric outcomes of interest.
Table 2. Results of the adjusted logistic regression analyses for marginalization on the medical and psychiatric outcomes of interest.
Disclosures: I. Mohamed, None; H. Bhatt, None; P. Moaf, None; L. Ng, None; D. Ostojic-Aitkens, None; B. Maguire, None; D. Levy, None; L. Hiraki, None; A. Toulany, None; C. DeCoste, None; A. Knight, None.
Background/Purpose: Adolescents with childhood-onset systemic lupus erythematosus (cSLE) face challenges in managing their disease and mental health. There is increasing evidence that community-level social and economic factors contribute to disparities in health outcomes for marginalized groups, beyond individual-level indicators like income or education. Yet there is limited information on the effects of these community-level factors in cSLE. We sought to investigate the relationship between neighbourhood area-level marginalization and health outcomes in children and adolescents with cSLE.
Methods: We conducted a retrospective cohort study of patients 9-18 years old with cSLE meeting System Lupus International Collaborating Clinics (SLICC) or American College of Rheumatology (ACR) SLE classification criteria and followed in the Lupus Clinic at SickKids between July 2018 and July 2020. The postal codes of patients were linked to the Ontario Marginalization (ON-Marg) Index, a measure derived from the Canadian census to capture health disparities at the area-level. The primary exposures were the four dimensions of the ON-Marg Index: ethnic concentration (concentration of new immigrants and visible minority persons); material deprivation (measure of income, education, single-parent households); residential instability (rates of housing and family instability); and dependency (reflects the population workforce eligibility). Health outcomes included the presence of: i) active disease (adjusted mean SLEDAI score >4) during the study period, ii) disease damage (SLICC/ACR Damage Index score >0) at the latest study visit, and iii) a comorbid psychiatric diagnosis (mood and/or anxiety disorder). We performed univariate and multivariable logistic regression analyses to determine if area-level marginalization was associated with the outcomes, adjusting for age, sex, disease duration, major organ involvement (nephritis and/or central nervous system disease), and glucocorticoid use. Estimates with a p< 0.05 were considered statistically significant.
Results: A total of 184 pediatric patients were included in the study; 29% had active disease, 16% had disease damage, and 18% had a comorbid mood and/or anxiety diagnosis (Table 1). Notably, 61% of patients lived in areas with the highest quintile for ethnic concentration and 46% of patients lived in areas with the lowest quintile for dependency (Figure 1). Those living in areas with higher ethnic concentrations had lower odds of a comorbid psychiatric diagnosis in unadjusted analysis (OR 0.67, 95% CI 0.48-0.94, p=0.021). In adjusted analysis, there were associations between ethnic concentration and lower comorbid psychiatric diagnosis (OR 0.66, 95% CI 0.42-1.04, p=0.073), and dependency with lower active disease (OR 0.56, 95% 0.30-1.04, p=0.066), though not statistically significant (Table 2).
Conclusion: In this sample of patients with cSLE, we found associations between the factors of community-level ethnic concentration and dependency with disease and mental health outcomes. Future studies should explore the patient, provider, and system-level factors influencing medical and psychiatric care among marginalized groups.
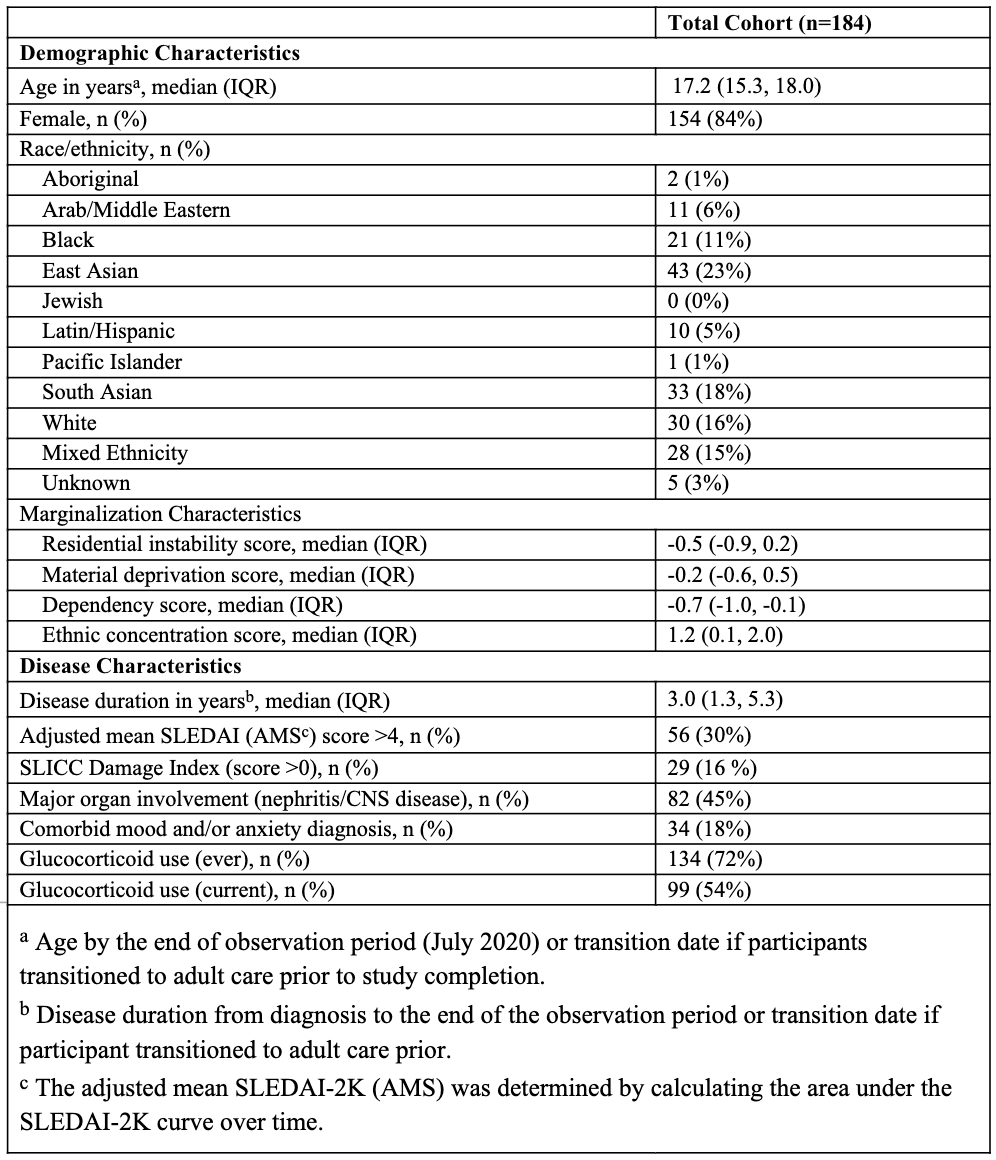 Table 1. Demographics and Disease Characteristics in Children and Adolescent Patients with cSLE.
Table 1. Demographics and Disease Characteristics in Children and Adolescent Patients with cSLE..jpeg) Figure 1. Quintile distribution of the Ontario Marginalization Index dimensions in the cSLE cohort (n=184).
Figure 1. Quintile distribution of the Ontario Marginalization Index dimensions in the cSLE cohort (n=184). .jpeg) Table 2. Results of the adjusted logistic regression analyses for marginalization on the medical and psychiatric outcomes of interest.
Table 2. Results of the adjusted logistic regression analyses for marginalization on the medical and psychiatric outcomes of interest. Disclosures: I. Mohamed, None; H. Bhatt, None; P. Moaf, None; L. Ng, None; D. Ostojic-Aitkens, None; B. Maguire, None; D. Levy, None; L. Hiraki, None; A. Toulany, None; C. DeCoste, None; A. Knight, None.

