Back
Poster Session A
Myopathic rheumatic diseases (polymyositis, dermatomyositis, inclusion body myositis)
Session: (0150–0180) Muscle Biology, Myositis and Myopathies Poster I
0156: Impact of Polymyositis and Dermatomyositis in Patients Admitted with Congestive Heart Failure: An Insight from the National Database
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- BB
Brinda Basida, MD
Brown university/ Rhode Island Hospital
East Greenwich, RI, United States
Abstract Poster Presenter(s)
Brinda Basida1, Sanket Basida2, Jasleen Kaur3, Urja Nagadia2, mahmoud mansour2, Palak Shah4 and Monil Majmundar5, 1DMC/Sinai Grace Hospital, Detroit, MI, 2University of Missouri, Columbia, MO, 3DMC/WSU, Saginaw, MI, 4Metropolitan Hospital Center, New York Medical College, New York, NY, 5University of Kansas Medical Center, Kansas City, KS
Background/Purpose: Polymyositis (PM) and Dermatomyositis (DM) are systemic autoimmune diseases of inflammatory infiltrates in skeletal muscle resulting in chronic muscle weakness. Systemic involvement of the lungs, esophagus, and heart is seen in patients with PM/DM. Cardiac complications in these patients have been demonstrated as a poor prognostic factor in previous studies. Most patients and physicians ignore these cardiac complications due to the lack of symptoms in the early stages. [1] Our study aims to analyze the impact of PM/DM on the in-hospital outcomes of patients with Congestive Heart Failure (CHF).
Methods: All adult hospitalized patients from January 2016 to December 2019 in the nationwide inpatient sample (NIS) were captured. The study population included all patients with a primary diagnosis of CHF using ICD-10 codes (International Classification of Diseases, tenth edition). We then identified patients with a secondary diagnosis of PM or DM. The CHF population was divided into patients with PM/DM (study) and without PM/DM (control). We used Wilcoxon rank sum test for comparing continuous variables and Chi-square tests for categorical variables. For univariate and multivariate analysis, we performed univariate and multivariate logistic regression models respectively. The primary outcome was mortality rates and secondary outcomes were morbidity rates and healthcare utilization.
Results: The sample size included 4,815,134 patients admitted for CHF, of which 99.95% did not have underlying PM/DM, while 0.05% did. 70.69% of patients in the study group were female and were relatively younger, with a mean age of 66 years vs. 71 years in the control group (p< 0.001). There was a higher mortality rate (4.47%) in those with PM/DM compared to those without it (2.65%) (adjusted OR=2.01, p< 0.003). There was a higher incidence of Cardiogenic shock in the study group. Still, the rate of Acute respiratory failure and need for mechanical ventilation were not statistically different between the two groups. The adjusted mean total hospitalization charge was $14,275 higher (p< 0.04), and the adjusted mean length of stay was 1.03 days higher (< 0.002) in group 2 compared to group 1.
Conclusion: Polymyositis/Dermatomyositis increases mortality by two-fold in CHF patients. It is also associated with increased cost and length of hospital stay, thus increasing the burden on patients and healthcare. Since there is no testing apart from the auxiliary examinations that are excellent in sensitivity and specificity to determine cardiac complications in its early stages, it is vital to pay more attention to the cardiac examination in PM/DM.
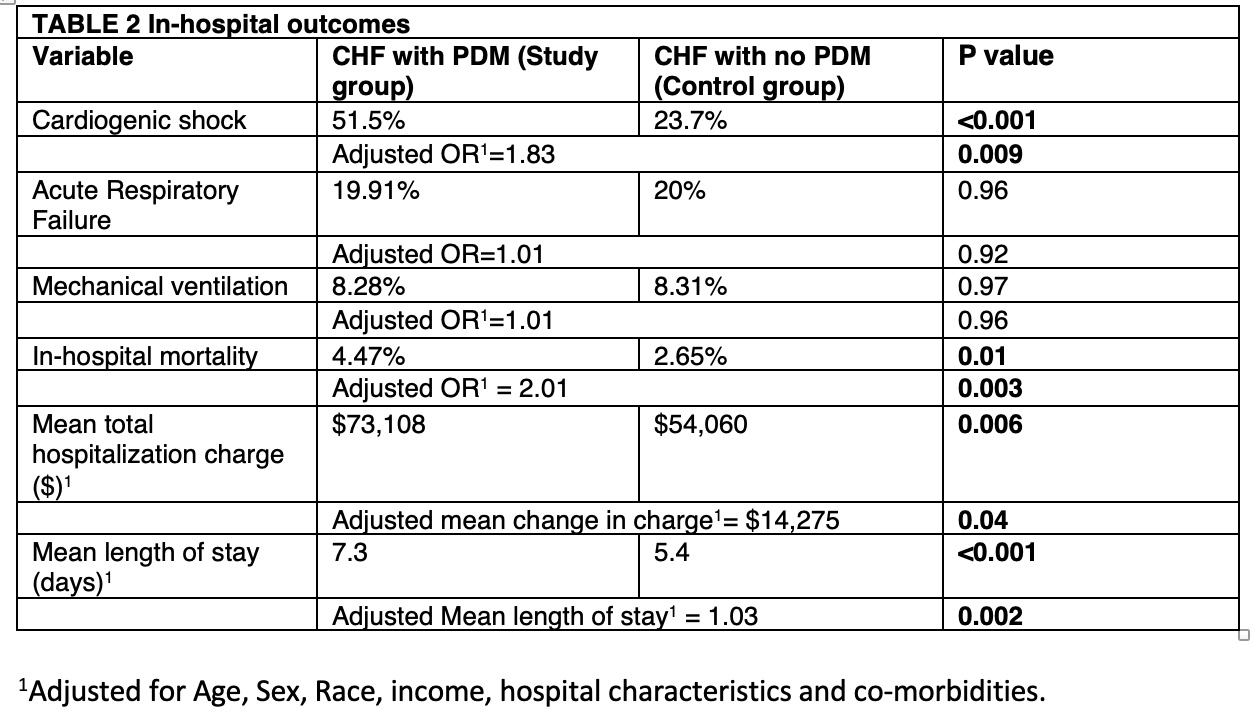 Table-1 In-Hospital outcomes and healthcare utilization in patients with congestive heart failure
Table-1 In-Hospital outcomes and healthcare utilization in patients with congestive heart failure
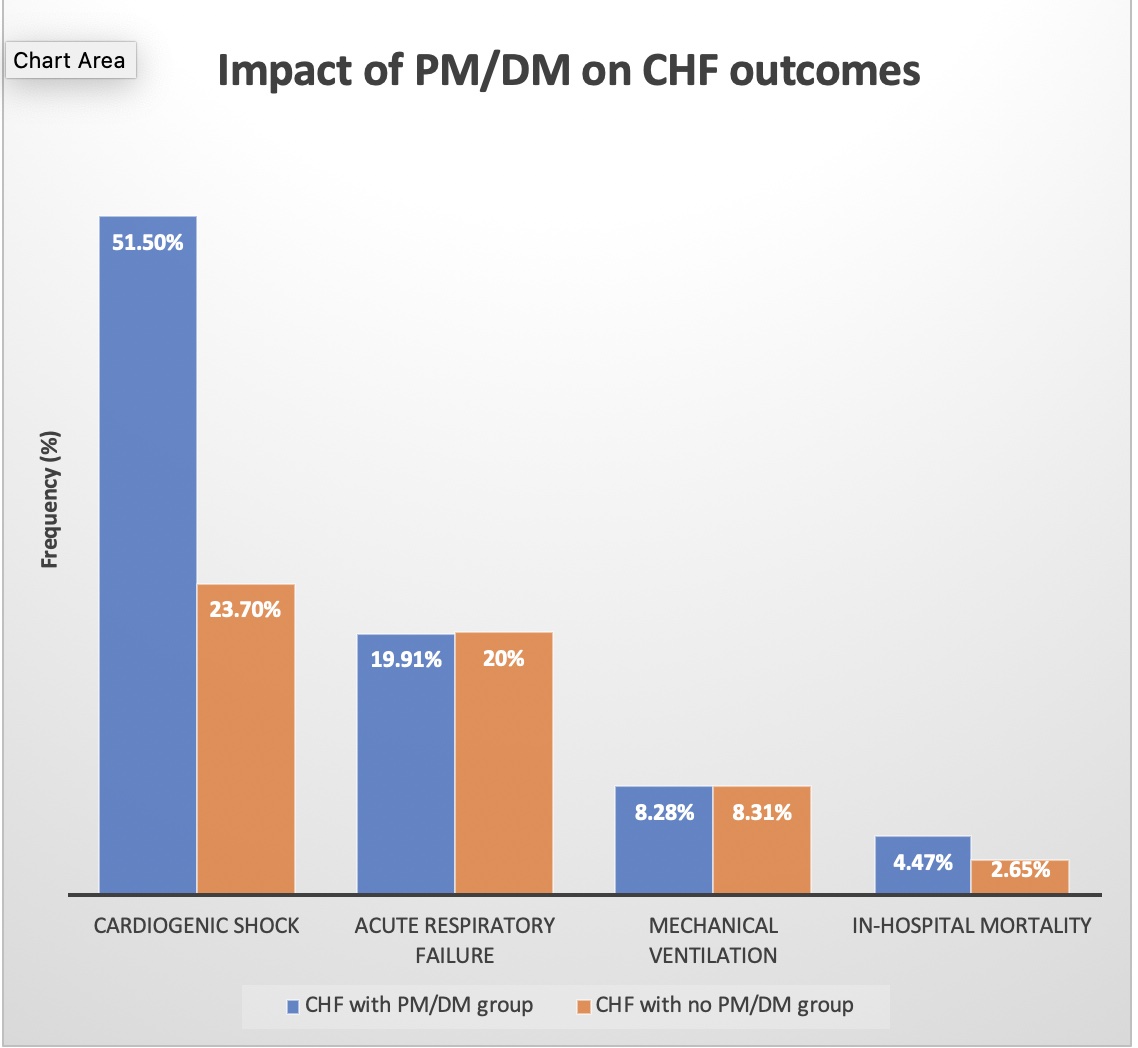 Figure-1 Impact of Polymyositis/Dermatomyositis on congestive heart failure outcomes
Figure-1 Impact of Polymyositis/Dermatomyositis on congestive heart failure outcomes
Disclosures: B. Basida, None; S. Basida, None; J. Kaur, None; U. Nagadia, None; m. mansour, None; P. Shah, None; M. Majmundar, None.
Background/Purpose: Polymyositis (PM) and Dermatomyositis (DM) are systemic autoimmune diseases of inflammatory infiltrates in skeletal muscle resulting in chronic muscle weakness. Systemic involvement of the lungs, esophagus, and heart is seen in patients with PM/DM. Cardiac complications in these patients have been demonstrated as a poor prognostic factor in previous studies. Most patients and physicians ignore these cardiac complications due to the lack of symptoms in the early stages. [1] Our study aims to analyze the impact of PM/DM on the in-hospital outcomes of patients with Congestive Heart Failure (CHF).
Methods: All adult hospitalized patients from January 2016 to December 2019 in the nationwide inpatient sample (NIS) were captured. The study population included all patients with a primary diagnosis of CHF using ICD-10 codes (International Classification of Diseases, tenth edition). We then identified patients with a secondary diagnosis of PM or DM. The CHF population was divided into patients with PM/DM (study) and without PM/DM (control). We used Wilcoxon rank sum test for comparing continuous variables and Chi-square tests for categorical variables. For univariate and multivariate analysis, we performed univariate and multivariate logistic regression models respectively. The primary outcome was mortality rates and secondary outcomes were morbidity rates and healthcare utilization.
Results: The sample size included 4,815,134 patients admitted for CHF, of which 99.95% did not have underlying PM/DM, while 0.05% did. 70.69% of patients in the study group were female and were relatively younger, with a mean age of 66 years vs. 71 years in the control group (p< 0.001). There was a higher mortality rate (4.47%) in those with PM/DM compared to those without it (2.65%) (adjusted OR=2.01, p< 0.003). There was a higher incidence of Cardiogenic shock in the study group. Still, the rate of Acute respiratory failure and need for mechanical ventilation were not statistically different between the two groups. The adjusted mean total hospitalization charge was $14,275 higher (p< 0.04), and the adjusted mean length of stay was 1.03 days higher (< 0.002) in group 2 compared to group 1.
Conclusion: Polymyositis/Dermatomyositis increases mortality by two-fold in CHF patients. It is also associated with increased cost and length of hospital stay, thus increasing the burden on patients and healthcare. Since there is no testing apart from the auxiliary examinations that are excellent in sensitivity and specificity to determine cardiac complications in its early stages, it is vital to pay more attention to the cardiac examination in PM/DM.
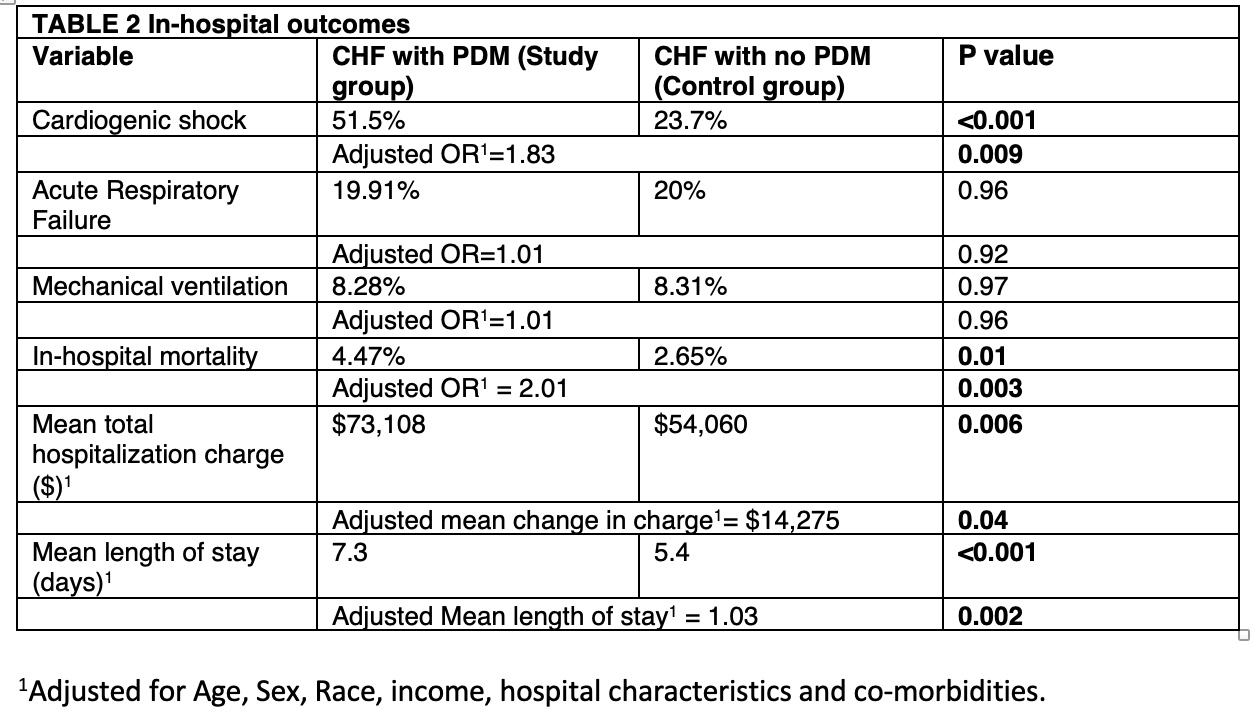 Table-1 In-Hospital outcomes and healthcare utilization in patients with congestive heart failure
Table-1 In-Hospital outcomes and healthcare utilization in patients with congestive heart failure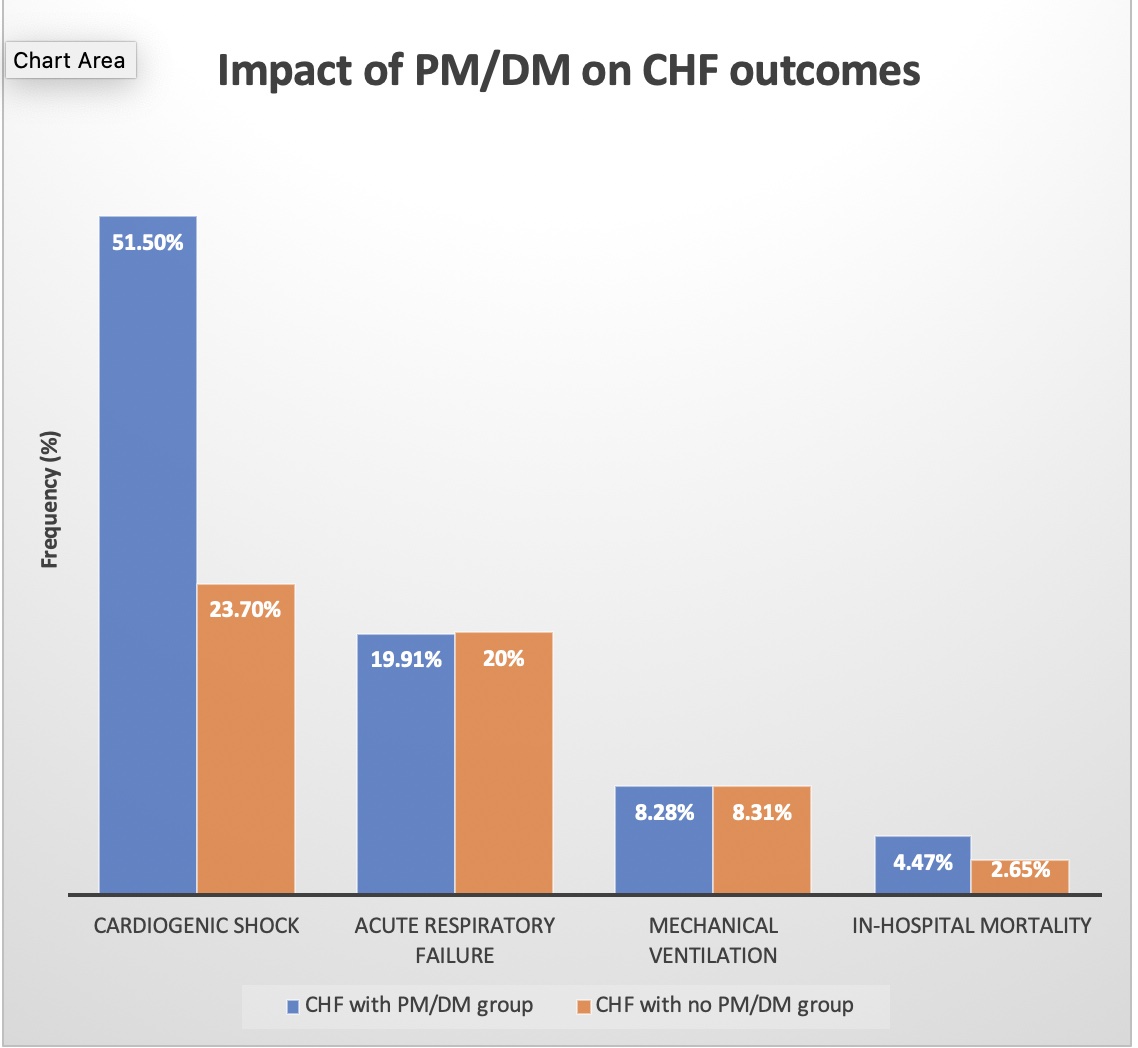 Figure-1 Impact of Polymyositis/Dermatomyositis on congestive heart failure outcomes
Figure-1 Impact of Polymyositis/Dermatomyositis on congestive heart failure outcomesDisclosures: B. Basida, None; S. Basida, None; J. Kaur, None; U. Nagadia, None; m. mansour, None; P. Shah, None; M. Majmundar, None.

