Back
Poster Session A
Rheumatoid arthritis (RA)
Session: (0241–0271) RA – Diagnosis, Manifestations, and Outcomes Poster I
0271: Temporal Trends and Risk of Rheumatoid Arthritis in Celiac Disease Patients: A Nationwide Population-based Study
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- BB
Brinda Basida, MD
Brown university/ Rhode Island Hospital
East Greenwich, RI, United States
Abstract Poster Presenter(s)
Brinda Basida1, maryam haider1, Noren Din2 and Vinit Gilvaz3, 1DMC/Sinai Grace Hospital, Detroit, MI, 2DMC/Sinai- Grace Hospital, Birmingham, AL, 3Brown University, East Providence, RI
Background/Purpose: There has been an increasing global prevalence of celiac diseases (CD) and rheumatoid arthritis (RA). Modifications in proteins play a significant role in the loss of tolerance and the development of immune response in both these diseases. Rheumatoid arthritis and celiac disease are connected based on similar histocompatibility antigens (HLA) mutations, serological markers, and rheumatological, and gastrointestinal manifestations. HLA locus is the most potent risk factor where different alleles confer risk of the two diseases. Several studies have described the "Gut-Joint Effect." This study aimed to investigate the co-existence and socioeconomic burden of rheumatoid arthritis in patients with celiac diseases.
Methods: The National Inpatient Sample database from 2000 to 2019 was queried for patients identified with CD. We utilized the international classification of disease (ICD) to identify patients diagnosed with CD, ICD-9 code of 579.0 from 2000 to Q3 2015, and ICD-10 code of K90.0 from Q4 2015 to 2019. To compare the risk of RA, a year-wise non-CD matched group is selected based on age, sex, and race using the 1:1 ratio nearest neighbor (greedy) propensity score method. Categorical variables are presented using the frequency distribution, and continuous variables such as age were presented using the mean (±standard deviation-SD). Group comparisons were performed using the student's t-test for continuous variables and the χ2 test for categorical variables. We performed hypothesis testing using a two-tailed p-value with a significance level of 0.05.
Results: After weighting, we identified 526559 patients with CD between 2000 and 2019. We identified 14885 (2.83%) RA patients in CD group and 8955 (1.83%) RA patients in non-CD matched group. The prevalence of RA in hospitalized CD patients increased from 2.40% in 2000 to 3.80% in 2019 with Ptrend< 0.001. Overall, CD patients have 57% higher odds of RA as compared to matched non-CD patients (OR, 1.57; 95% CI, 1.49 – 1.67). The multivariate analyses showed that older age (aOR : 2.4; 95% CI, 2.1 - 2.8 for 41-64 years, 2.0; 95% CI, 1.7 - 2.4 for 65 years and above, compared to 18-40 years, all P < 0.0001), female (aOR, 2.6; 95% CI, 2.3 - 2.9; P < 0.0001) as compared to male, socioeconomic status in quartile 1 (aOR, 1.2 ; 95% CI, 1.1 - 1.3; P = 0.02) as compared to quartile 4, Medicaid (aOR : 1.3; 95% CI, 1.2 – 1.5) as compared to private insurance have higher risk of RA in CD patients.
OR= odd's ratio; aOR= adjusted odd's ratio
Conclusion: Our study highlights the prevalence of rheumatoid arthritis in hospitalized patients with celiac disease compared to the general population. There is an overall increased hospitalization and socioeconomic burden in these patients. Reinforcing and educating the healthcare workers will help improve the overall treatment outcome in these patients.
The association between rheumatoid arthritis and celiac disease could have several clinical implications. Adopting a gluten-free diet has been shown to alleviate rheumatic manifestations in CD. Still, it is unclear if similar dietary interventions are effective in patients with RA, highlighting the need for further research in this area.
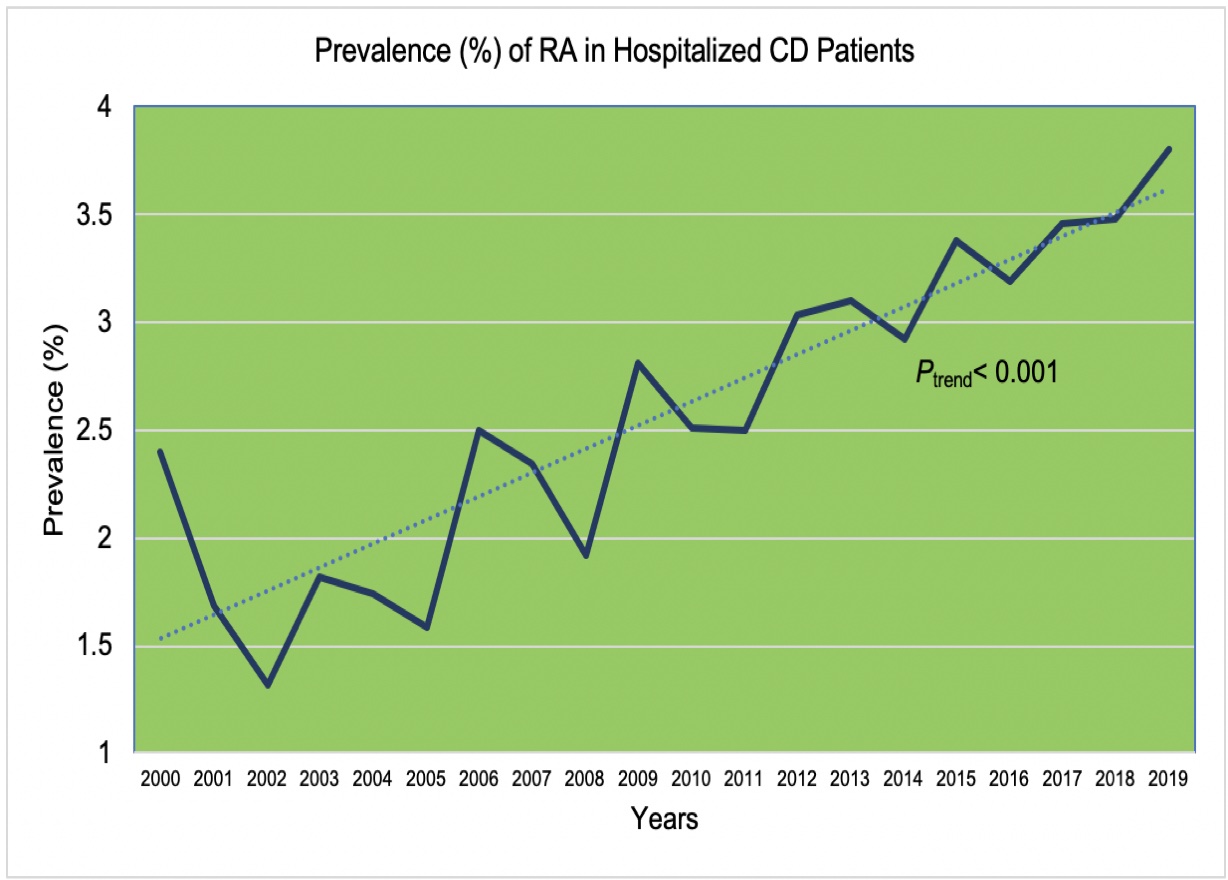 Figure 1 Prevalence of Rheumatoid arthritis in hospitalized Celiac disease patients admitted NIS 2000-2019.
Figure 1 Prevalence of Rheumatoid arthritis in hospitalized Celiac disease patients admitted NIS 2000-2019.
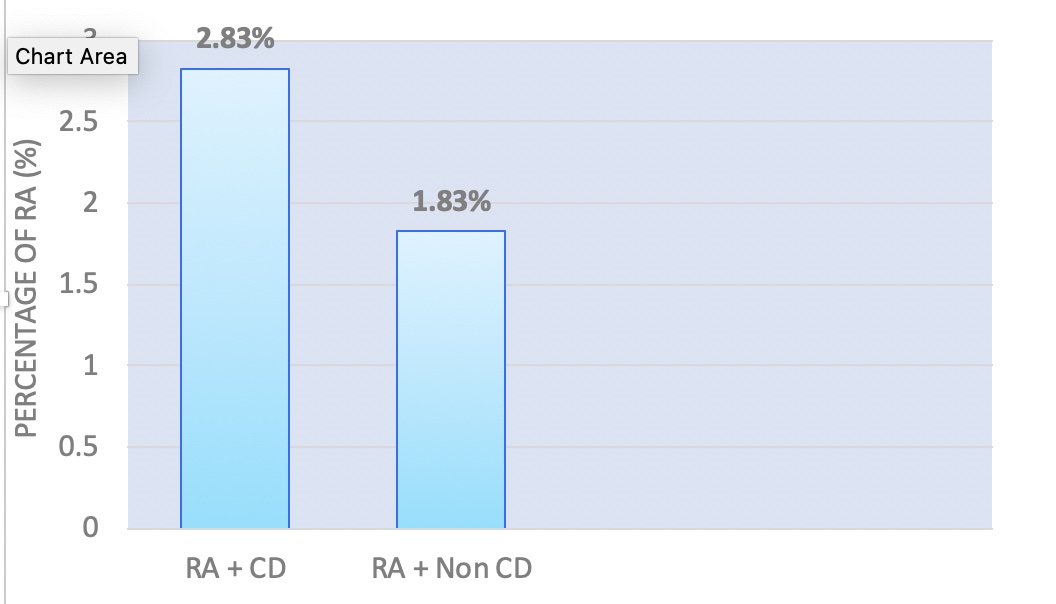 Figure 2 Prevalence of Rheumatoid arthritis in patients with Celiac disease vs. Non-Celiac disease
Figure 2 Prevalence of Rheumatoid arthritis in patients with Celiac disease vs. Non-Celiac disease
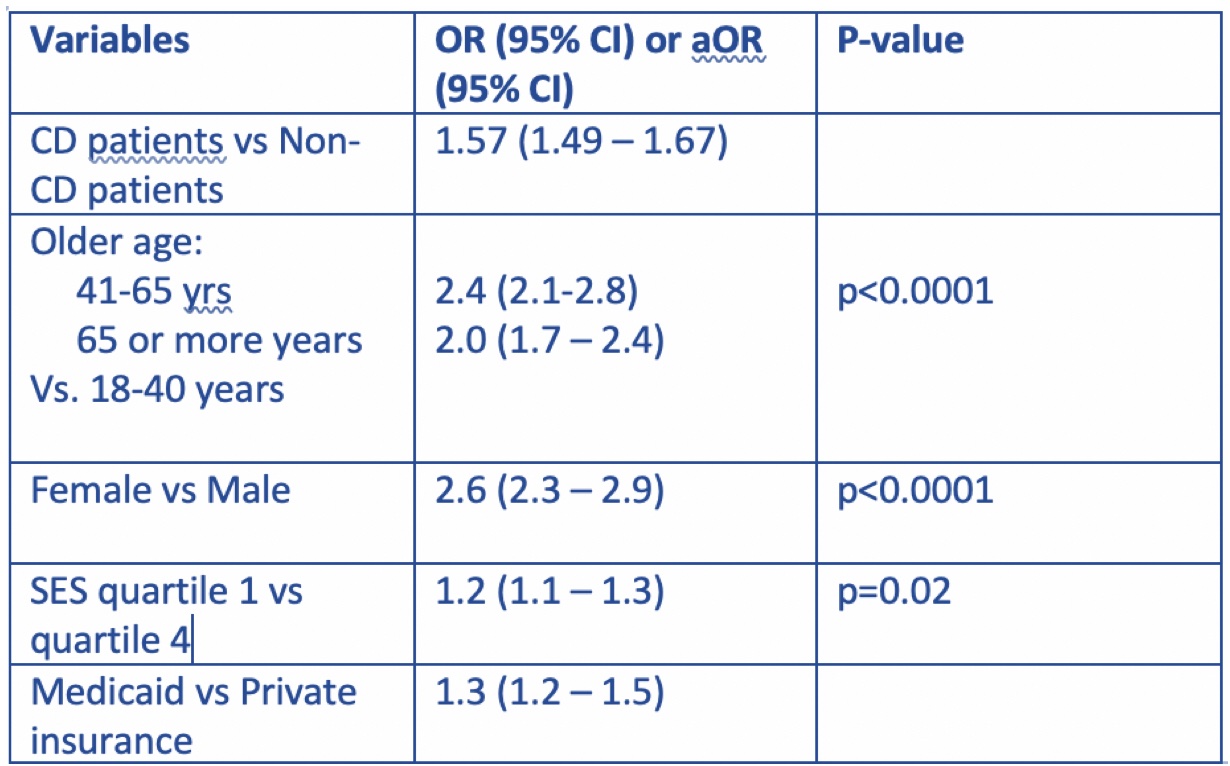 Table -1 Predictors of Rheumatoid arthritis
Table -1 Predictors of Rheumatoid arthritis
Disclosures: B. Basida, None; m. haider, None; N. Din, None; V. Gilvaz, None.
Background/Purpose: There has been an increasing global prevalence of celiac diseases (CD) and rheumatoid arthritis (RA). Modifications in proteins play a significant role in the loss of tolerance and the development of immune response in both these diseases. Rheumatoid arthritis and celiac disease are connected based on similar histocompatibility antigens (HLA) mutations, serological markers, and rheumatological, and gastrointestinal manifestations. HLA locus is the most potent risk factor where different alleles confer risk of the two diseases. Several studies have described the "Gut-Joint Effect." This study aimed to investigate the co-existence and socioeconomic burden of rheumatoid arthritis in patients with celiac diseases.
Methods: The National Inpatient Sample database from 2000 to 2019 was queried for patients identified with CD. We utilized the international classification of disease (ICD) to identify patients diagnosed with CD, ICD-9 code of 579.0 from 2000 to Q3 2015, and ICD-10 code of K90.0 from Q4 2015 to 2019. To compare the risk of RA, a year-wise non-CD matched group is selected based on age, sex, and race using the 1:1 ratio nearest neighbor (greedy) propensity score method. Categorical variables are presented using the frequency distribution, and continuous variables such as age were presented using the mean (±standard deviation-SD). Group comparisons were performed using the student's t-test for continuous variables and the χ2 test for categorical variables. We performed hypothesis testing using a two-tailed p-value with a significance level of 0.05.
Results: After weighting, we identified 526559 patients with CD between 2000 and 2019. We identified 14885 (2.83%) RA patients in CD group and 8955 (1.83%) RA patients in non-CD matched group. The prevalence of RA in hospitalized CD patients increased from 2.40% in 2000 to 3.80% in 2019 with Ptrend< 0.001. Overall, CD patients have 57% higher odds of RA as compared to matched non-CD patients (OR, 1.57; 95% CI, 1.49 – 1.67). The multivariate analyses showed that older age (aOR : 2.4; 95% CI, 2.1 - 2.8 for 41-64 years, 2.0; 95% CI, 1.7 - 2.4 for 65 years and above, compared to 18-40 years, all P < 0.0001), female (aOR, 2.6; 95% CI, 2.3 - 2.9; P < 0.0001) as compared to male, socioeconomic status in quartile 1 (aOR, 1.2 ; 95% CI, 1.1 - 1.3; P = 0.02) as compared to quartile 4, Medicaid (aOR : 1.3; 95% CI, 1.2 – 1.5) as compared to private insurance have higher risk of RA in CD patients.
OR= odd's ratio; aOR= adjusted odd's ratio
Conclusion: Our study highlights the prevalence of rheumatoid arthritis in hospitalized patients with celiac disease compared to the general population. There is an overall increased hospitalization and socioeconomic burden in these patients. Reinforcing and educating the healthcare workers will help improve the overall treatment outcome in these patients.
The association between rheumatoid arthritis and celiac disease could have several clinical implications. Adopting a gluten-free diet has been shown to alleviate rheumatic manifestations in CD. Still, it is unclear if similar dietary interventions are effective in patients with RA, highlighting the need for further research in this area.
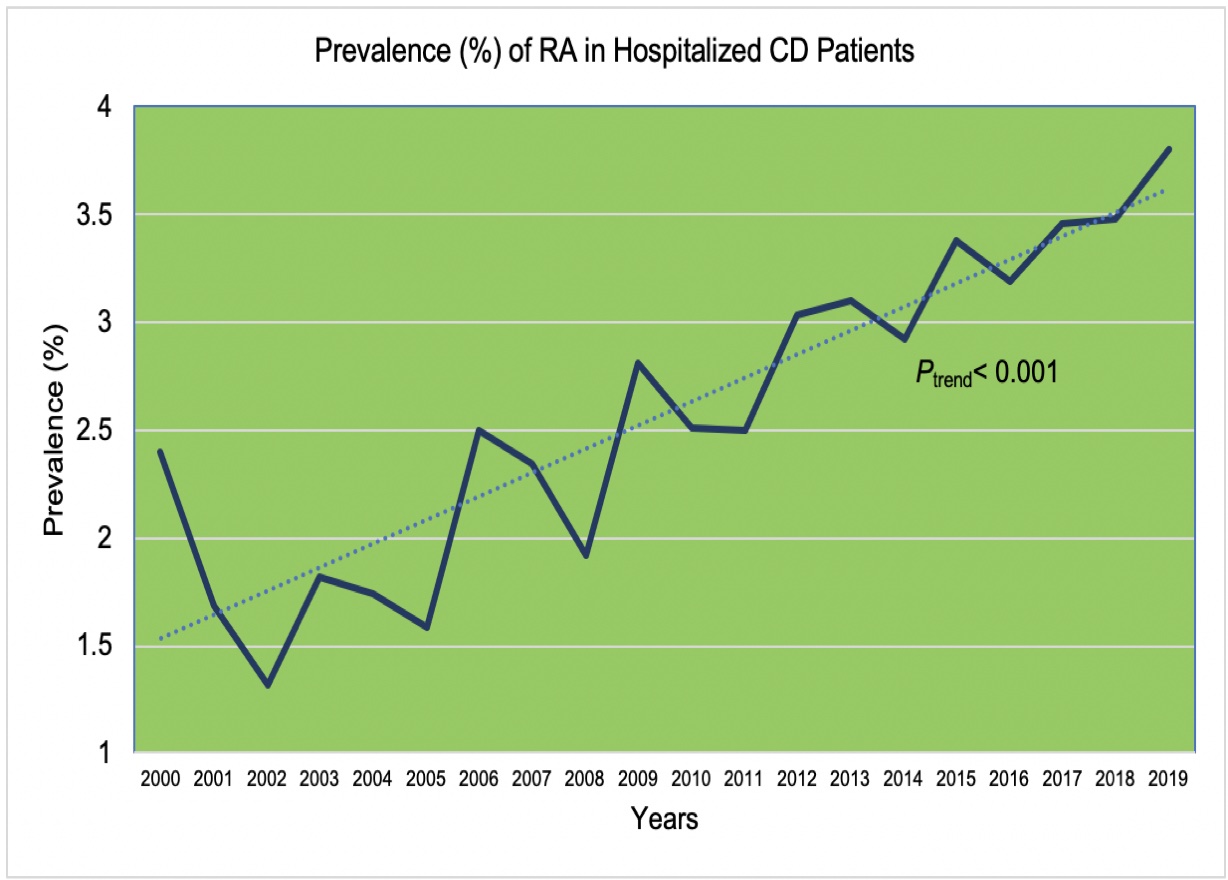 Figure 1 Prevalence of Rheumatoid arthritis in hospitalized Celiac disease patients admitted NIS 2000-2019.
Figure 1 Prevalence of Rheumatoid arthritis in hospitalized Celiac disease patients admitted NIS 2000-2019.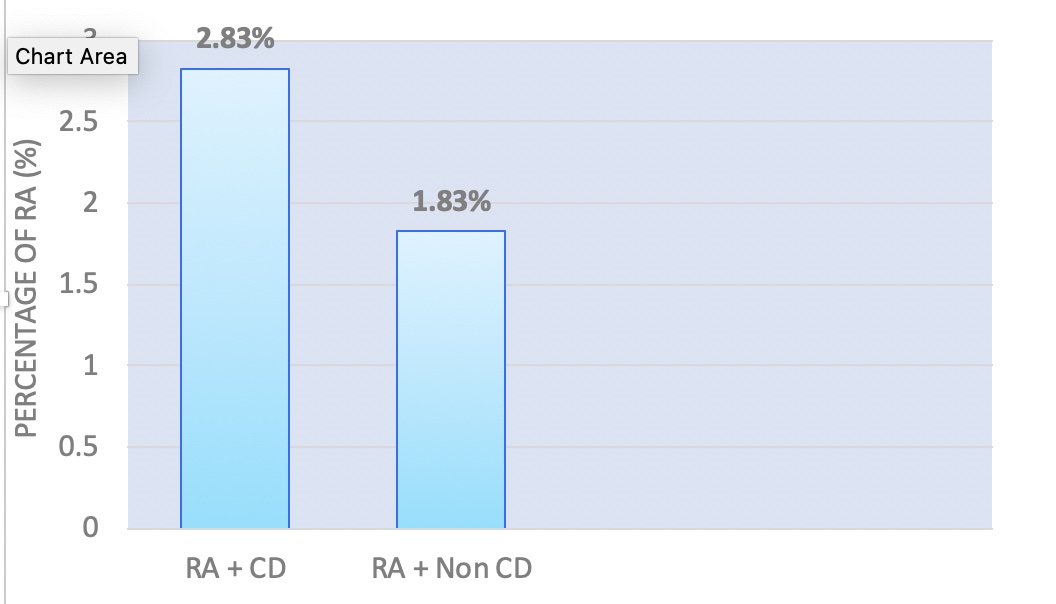 Figure 2 Prevalence of Rheumatoid arthritis in patients with Celiac disease vs. Non-Celiac disease
Figure 2 Prevalence of Rheumatoid arthritis in patients with Celiac disease vs. Non-Celiac disease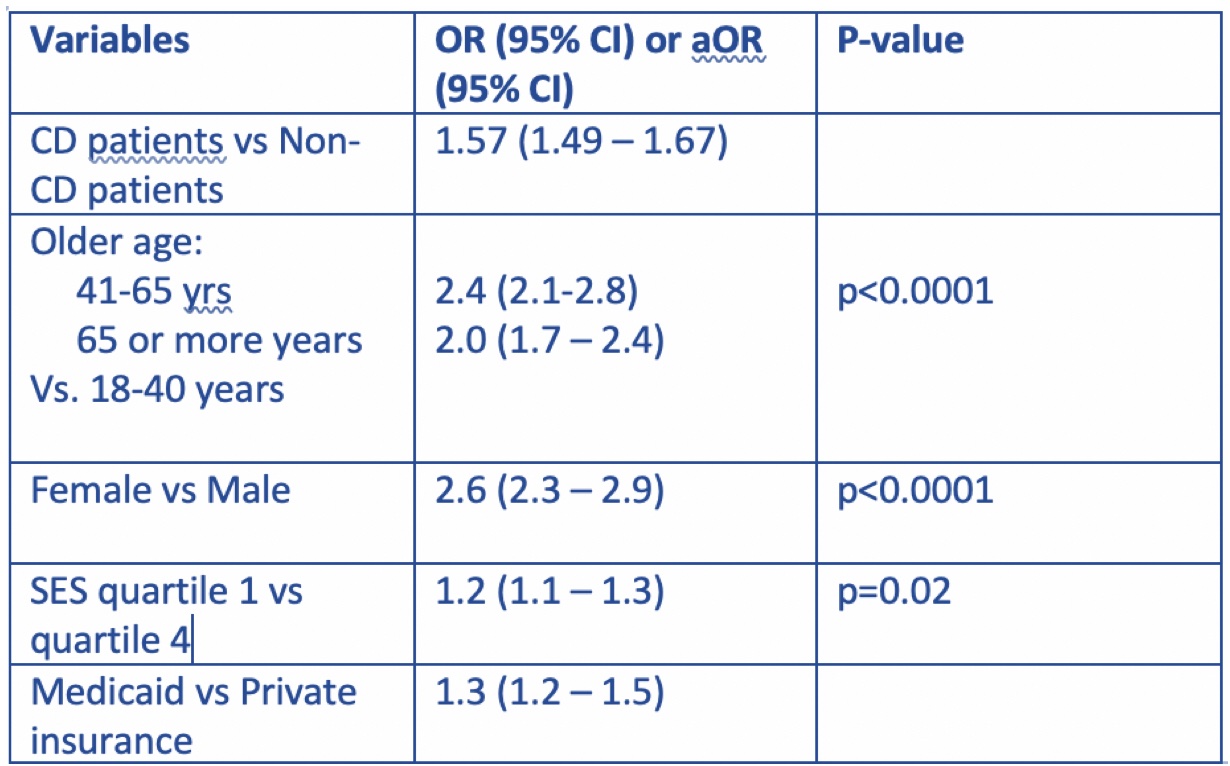 Table -1 Predictors of Rheumatoid arthritis
Table -1 Predictors of Rheumatoid arthritisDisclosures: B. Basida, None; m. haider, None; N. Din, None; V. Gilvaz, None.

