Back
Poster Session A
Diversity, inclusion and racial disparities
Session: (0085–0122) Healthcare Disparities in Rheumatology Poster
0119: Emergency Department Utilization by Persons with Inflammatory Arthritis Conditions Varies by Geographic Location of Residence
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- CB
Cheryl Barnabe, MD, FRCPC, MSc
University of Calgary
Calgary, AB, Canada
Abstract Poster Presenter(s)
Cheryl Barnabe1, Patrick McLane2, Nadia Luca1, Kelsey Chomistek1, Meghan Elliott1, Shanon McQuitty3, Steven Katz2, Eileen Davidson3, Clare Hildebrandt4, Katie Lin1, Brian Holroyd2 and Claire Barber1, 1University of Calgary, Calgary, AB, Canada, 2University of Alberta, Edmonton, AB, Canada, 3Arthritis Research Canada, Vancouver, BC, Canada, 4Patient and Family Advisors, Alberta Health Services, Calgary, AB, Canada
Background/Purpose: Rheumatology services in Canada are largely restricted to urban centres, resulting in significant access difficulties for residents of rural and remote locations. As a result, some emergency department (ED) utilization by persons with inflammatory arthritis (IA) conditions may reflect deficiencies in current arthritis health service delivery models. Our objective was to characterize ED use by persons with IA conditions based on residence in an urban or rural location to inform required ambulatory care service enhancements.
Methods: Estimates of ED utilization were obtained from analyzing population-based data from a universal provincial health system in Alberta, Canada (~4.4 million residents). Validated case definitions were applied to physician claims and hospitalization administrative datasets (years 2002-2018) to create prevalent cohorts of persons with Rheumatoid Arthritis (RA), Ankylosing Spondylitis (AS), Psoriatic Arthritis (PsA), gout and Juvenile Idiopathic Arthritis (JIA). Records were then linked to the National Ambulatory Care Reporting System dataset in which ED use is documented with details of presentation (timing, acuity, diagnosis, and disposition). Estimates were stratified by postal code for descriptive analysis; annual estimates for years 2008-2018 were generated to identify possible time trends, and data presented here are from fiscal year 2017-2018.
Results: There were 60,373 persons with an IA condition (15,320 rural) with 156,570 ED visits (52,739 rural) in the 2017-2018 fiscal year (Table 1). Those living in rural locations were significantly more likely to have at least 1 ED visit per year (difference RA 19.5%, PsA 18.3%, AS 20.5%, gout 19.3%, JIA 14.5%). For all conditions except JIA, an individual rural resident with an IA condition had nearly twice the annual mean number of visits to the ED compared to urban residents (all p< 0.01). A significantly higher number of visits by rural persons with IA conditions were triaged into less urgent and non-urgent acuity levels (all p< 0.01). Rural persons with IA conditions were significantly more likely to present to the ED during daytime hours (08:00-16:00 hours) than their urban counterparts, and for all conditions except JIA during a weekday (range 72-73% for rural vs 68-69%) rather than a weekend or holiday day. Lengths of stay in the ED were significantly shorter for rural persons with RA, PsA, AS and gout (range 197-230 minutes) than urban persons with these conditions (range 323-470 minutes). The frequency of return visits to the ED within 72 hours of the initial presentation was significantly higher in rural patients with RA (difference 8.9%; 95%CI 7.6, 10.3), PsA (difference 9.9%; 95%CI 5.4, 14.3), AS (difference 6.0%; 95%CI 3.7, 8.2), and Gout (difference 7.3%; 95%CI 6.2, 8.3). Rural patients were not significantly more likely to present to the ED for a flare of their IA condition.
Conclusion: The ED is an important health service access location for rural patients with IA conditions, although not directly related to their arthritis condition. Persons with JIA conditions and who are rural residents are potentially seeking ED care in urban centres.
.jpg) Table 1. Emergency Department Use by Urban and Rural Patients with Inflammatory Arthritis Conditions in Alberta, Canada (fiscal year 2017-2018)
Table 1. Emergency Department Use by Urban and Rural Patients with Inflammatory Arthritis Conditions in Alberta, Canada (fiscal year 2017-2018)
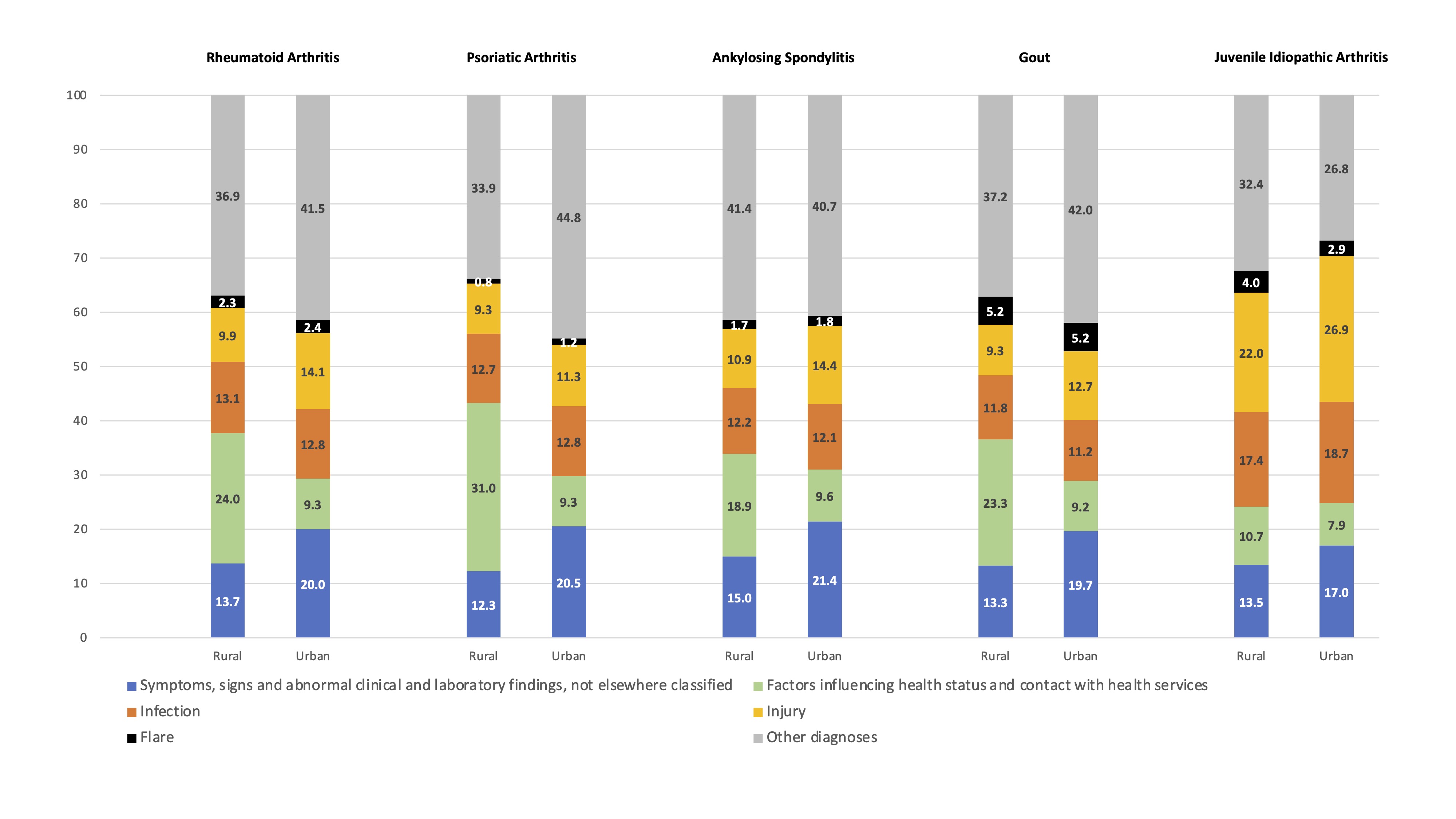 Figure 1. Diagnoses from Emergency Department Use by Rural and Urban Residents with Inflammatory Arthritis Conditions in Alberta, Canada (fiscal year 2017-2018, proportions)
Figure 1. Diagnoses from Emergency Department Use by Rural and Urban Residents with Inflammatory Arthritis Conditions in Alberta, Canada (fiscal year 2017-2018, proportions)
Disclosures: C. Barnabe, Janssen, Fresenius Kabi, Celltrion Healthcare, Pfizer; P. McLane, None; N. Luca, None; K. Chomistek, None; M. Elliott, None; S. McQuitty, None; S. Katz, None; E. Davidson, None; C. Hildebrandt, None; K. Lin, None; B. Holroyd, None; C. Barber, None.
Background/Purpose: Rheumatology services in Canada are largely restricted to urban centres, resulting in significant access difficulties for residents of rural and remote locations. As a result, some emergency department (ED) utilization by persons with inflammatory arthritis (IA) conditions may reflect deficiencies in current arthritis health service delivery models. Our objective was to characterize ED use by persons with IA conditions based on residence in an urban or rural location to inform required ambulatory care service enhancements.
Methods: Estimates of ED utilization were obtained from analyzing population-based data from a universal provincial health system in Alberta, Canada (~4.4 million residents). Validated case definitions were applied to physician claims and hospitalization administrative datasets (years 2002-2018) to create prevalent cohorts of persons with Rheumatoid Arthritis (RA), Ankylosing Spondylitis (AS), Psoriatic Arthritis (PsA), gout and Juvenile Idiopathic Arthritis (JIA). Records were then linked to the National Ambulatory Care Reporting System dataset in which ED use is documented with details of presentation (timing, acuity, diagnosis, and disposition). Estimates were stratified by postal code for descriptive analysis; annual estimates for years 2008-2018 were generated to identify possible time trends, and data presented here are from fiscal year 2017-2018.
Results: There were 60,373 persons with an IA condition (15,320 rural) with 156,570 ED visits (52,739 rural) in the 2017-2018 fiscal year (Table 1). Those living in rural locations were significantly more likely to have at least 1 ED visit per year (difference RA 19.5%, PsA 18.3%, AS 20.5%, gout 19.3%, JIA 14.5%). For all conditions except JIA, an individual rural resident with an IA condition had nearly twice the annual mean number of visits to the ED compared to urban residents (all p< 0.01). A significantly higher number of visits by rural persons with IA conditions were triaged into less urgent and non-urgent acuity levels (all p< 0.01). Rural persons with IA conditions were significantly more likely to present to the ED during daytime hours (08:00-16:00 hours) than their urban counterparts, and for all conditions except JIA during a weekday (range 72-73% for rural vs 68-69%) rather than a weekend or holiday day. Lengths of stay in the ED were significantly shorter for rural persons with RA, PsA, AS and gout (range 197-230 minutes) than urban persons with these conditions (range 323-470 minutes). The frequency of return visits to the ED within 72 hours of the initial presentation was significantly higher in rural patients with RA (difference 8.9%; 95%CI 7.6, 10.3), PsA (difference 9.9%; 95%CI 5.4, 14.3), AS (difference 6.0%; 95%CI 3.7, 8.2), and Gout (difference 7.3%; 95%CI 6.2, 8.3). Rural patients were not significantly more likely to present to the ED for a flare of their IA condition.
Conclusion: The ED is an important health service access location for rural patients with IA conditions, although not directly related to their arthritis condition. Persons with JIA conditions and who are rural residents are potentially seeking ED care in urban centres.
.jpg) Table 1. Emergency Department Use by Urban and Rural Patients with Inflammatory Arthritis Conditions in Alberta, Canada (fiscal year 2017-2018)
Table 1. Emergency Department Use by Urban and Rural Patients with Inflammatory Arthritis Conditions in Alberta, Canada (fiscal year 2017-2018)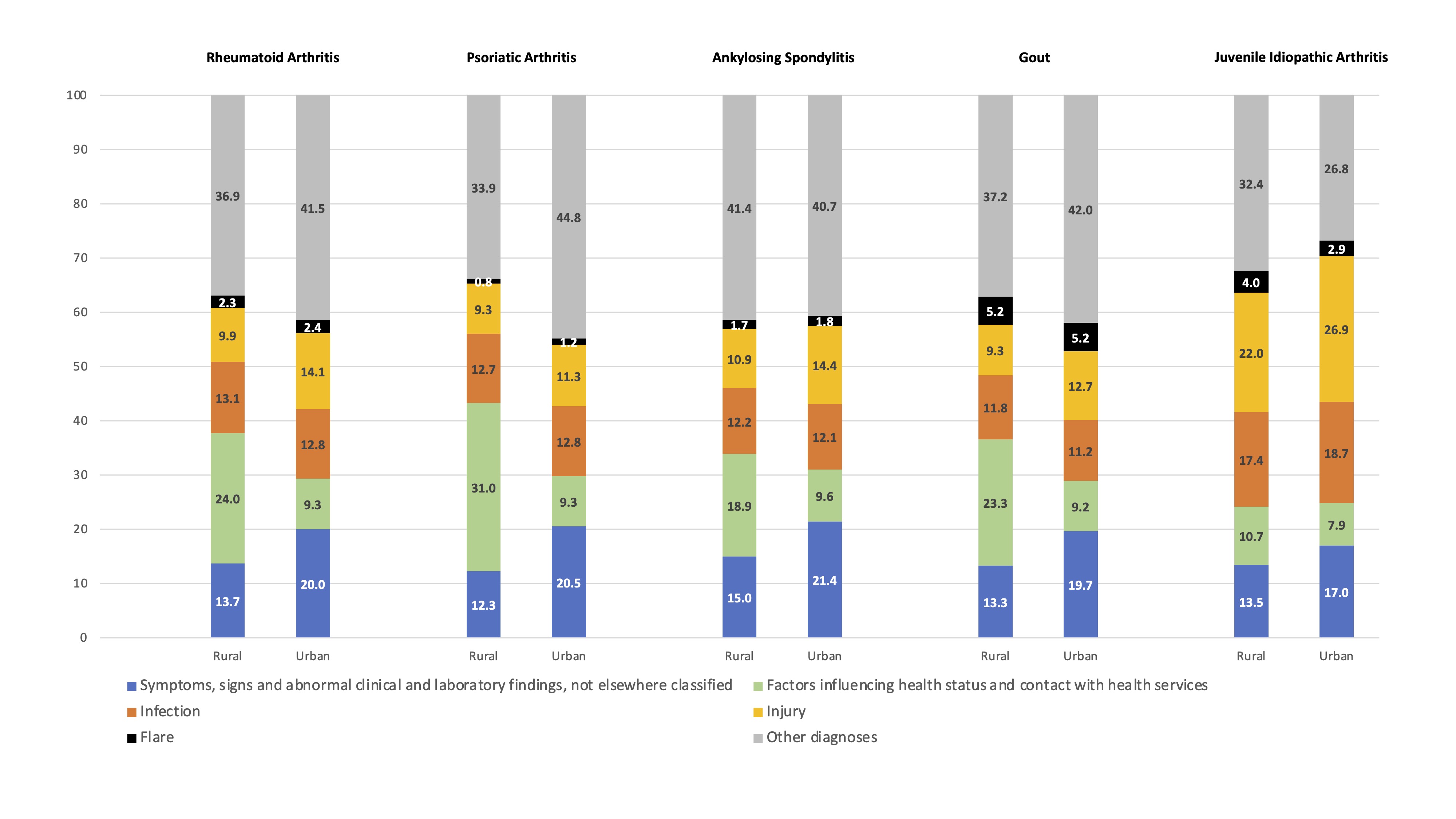 Figure 1. Diagnoses from Emergency Department Use by Rural and Urban Residents with Inflammatory Arthritis Conditions in Alberta, Canada (fiscal year 2017-2018, proportions)
Figure 1. Diagnoses from Emergency Department Use by Rural and Urban Residents with Inflammatory Arthritis Conditions in Alberta, Canada (fiscal year 2017-2018, proportions)Disclosures: C. Barnabe, Janssen, Fresenius Kabi, Celltrion Healthcare, Pfizer; P. McLane, None; N. Luca, None; K. Chomistek, None; M. Elliott, None; S. McQuitty, None; S. Katz, None; E. Davidson, None; C. Hildebrandt, None; K. Lin, None; B. Holroyd, None; C. Barber, None.

