Back
Poster Session A
Myopathic rheumatic diseases (polymyositis, dermatomyositis, inclusion body myositis)
Session: (0150–0180) Muscle Biology, Myositis and Myopathies Poster I
0180: Alterations of Nutritional Status in Patients with Idiopathic Inflammatory Myopathies and Their Association with Disease-related Features
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall

Sabína Oreská, MD
Institute of Rheumatology
Prague, Czech Republic
Abstract Poster Presenter(s)
Sabína Oreská1, Hana Storkanova1, Maja Spiritovic2, Barbora Hermankova2, Michal Vrablík3, Karel Pavelka4, Ladislav Šenolt5, Heřman Mann1, Jiří Vencovský5 and Michal Tomcik1, 1Institute of Rheumatology, Department of Rheumatology, 1st Faculty of Medicine, Charles University, Prague, Czech Republic, Prague, Czech Republic, 2Institute of Rheumatology, Department of Physiotherapy, Faculty of Physical Education and Sport, Charles University, Prague, Czech Republic, Prague, Czech Republic, 33rd Department of Internal Medicine, General University Hospital and 1st Faculty of Medicine, Charles University, Prague, Czech Republic, Prague, Czech Republic, 4Institute of Rheumatology, Department of Rheumatology, 1st Faculty of Medicine, Charles University, Prague, Czech Republic, Praha, Czech Republic, 5Institute of Rheumatology and Department of Rheumatology, First Faculty of Medicine, Charles University, Prague, Czech Republic
Background/Purpose: Systemic inflammation, involvement of the gastrointestinal tract, and glucocorticoid (GC) treatment in idiopathic inflammatory myopathies (IIM) can have a negative impact on nutrition and intermediate metabolic pathways. The aim of this study was to evaluate the differences in the nutrition status of IIM patients in comparison with healthy controls (HC) and explore the associations with disease-specific features.
Methods: 133 patients with IIM (106 females; mean age 60.3; disease duration 2.2 years; dermatomyositis (DM) 45 / polymyositis (PM) 25 / immune-mediated necrotizing myositis (IMNM) 46, antisynthetase syndrome (ASS) 17) and 133 age-/sex-matched HC (106 females, mean age 60.2) were included. Patients with IIM fulfilled the 2017 EULAR/ACR classification criteria for adult IIM. Levels of selected nutrition parameters were measured in sera after 8 hours of fasting. In IIM patients, disease activity, damage, and muscle involvement [Myositis Intention to Treat Activity Index (MITAX), Myositis Damage Index (MDI), Manual Muscle Testing (MMT)-8,]) were assessed. Comorbidities and current treatment were recorded.
Results: In IIM, disease activity and damage were predominantly mild (MITAX 0.11, MDI 0.05, MMT-8 62). Nevertheless, compared to HC, IIM patients had significantly decreased levels of total protein, albumin and prealbumin, transferrin, and minerals (Fe, Zn) (p< 0.005 for all). Despite the levels of 1,25-OH-vitamin D (calcitriol) being significantly decreased in IIM compared to HC (p< 0.001), levels of calcidiol were comparable. Orosomucoid, lactate dehydrogenase (LDH), and vitamin B12 were significantly higher (p< 0.001 for both) in IIM compared to HC, as well as levels of insulin and C-peptide (p< 0.001 for both), and free thyroxine (p=0.01). On the other hand, cholinesterase levels (a marker of synthetic liver function) were decreased in IIM (p< 0.05). A trend to a higher complement C3 (p=0.09) and significantly lower C4 (p< 0.05) was observed in IIM compared to HC. Among the individual IIM subsets, there were significant differences in the levels of proteins, vitamin D, and LDH, with the most unfavorable changes in IMNM (p< 0.05). In the total IIM group, changes in the nutrition markers were associated mainly with disease duration, activity (MITAX and serum markers of muscular damage), body mass index (BMI), and the current dose of GC. Levels of proteins negatively correlated with disease activity and the current dose of GC but positively with disease duration, similarly to the levels of vitamin D. Complement C4 and C3 both correlated positively with BMI and negatively with MITAX. Increased levels of insulin and C-peptide were associated with higher BMI and the current dose of GC, while insulin correlated negatively with age (Table 1).
Conclusion: We have observed significant alterations in the serum markers of nutritional status in our IIM patients compared to age-/sex-matched healthy individuals. Differences were also found among the four subtypes of IIM. These alterations were associated with laboratory parameters of disease activity and the current dose of corticosteroids.
Acknowledgment: Supported by AZV NV18-01-00161A, MHCR-00023728, SVV-260523, GAUK 312218
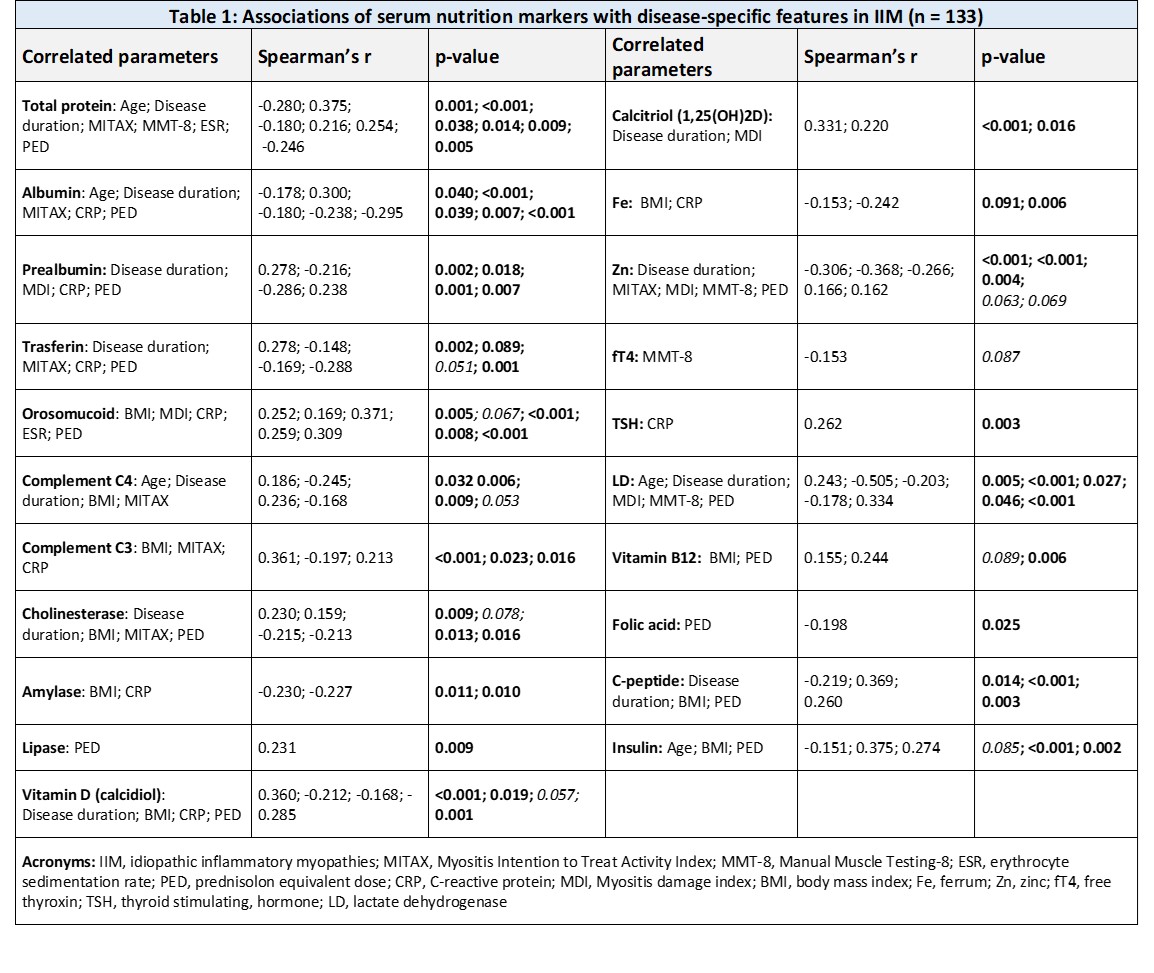 Table 1: Associations of serum nutrition markers with disease-specific features in IIM (n = 133)
Table 1: Associations of serum nutrition markers with disease-specific features in IIM (n = 133)
Disclosures: S. Oreská, None; H. Storkanova, None; M. Spiritovic, None; B. Hermankova, None; M. Vrablík, None; K. Pavelka, MSD, Pfizer, Roche, Eli Lilly, Medac, UCB, SOBI, Biogen, Sandoz, Viatris; L. Šenolt, None; H. Mann, None; J. Vencovský, Abbvie, Biogen, Boehringer, Eli Lilly, Gilead, Kezar, Merck, Novartis, Octapharma, Pfizer, Takeda, UCB, Werfen, Argenx; M. Tomcik, None.
Background/Purpose: Systemic inflammation, involvement of the gastrointestinal tract, and glucocorticoid (GC) treatment in idiopathic inflammatory myopathies (IIM) can have a negative impact on nutrition and intermediate metabolic pathways. The aim of this study was to evaluate the differences in the nutrition status of IIM patients in comparison with healthy controls (HC) and explore the associations with disease-specific features.
Methods: 133 patients with IIM (106 females; mean age 60.3; disease duration 2.2 years; dermatomyositis (DM) 45 / polymyositis (PM) 25 / immune-mediated necrotizing myositis (IMNM) 46, antisynthetase syndrome (ASS) 17) and 133 age-/sex-matched HC (106 females, mean age 60.2) were included. Patients with IIM fulfilled the 2017 EULAR/ACR classification criteria for adult IIM. Levels of selected nutrition parameters were measured in sera after 8 hours of fasting. In IIM patients, disease activity, damage, and muscle involvement [Myositis Intention to Treat Activity Index (MITAX), Myositis Damage Index (MDI), Manual Muscle Testing (MMT)-8,]) were assessed. Comorbidities and current treatment were recorded.
Results: In IIM, disease activity and damage were predominantly mild (MITAX 0.11, MDI 0.05, MMT-8 62). Nevertheless, compared to HC, IIM patients had significantly decreased levels of total protein, albumin and prealbumin, transferrin, and minerals (Fe, Zn) (p< 0.005 for all). Despite the levels of 1,25-OH-vitamin D (calcitriol) being significantly decreased in IIM compared to HC (p< 0.001), levels of calcidiol were comparable. Orosomucoid, lactate dehydrogenase (LDH), and vitamin B12 were significantly higher (p< 0.001 for both) in IIM compared to HC, as well as levels of insulin and C-peptide (p< 0.001 for both), and free thyroxine (p=0.01). On the other hand, cholinesterase levels (a marker of synthetic liver function) were decreased in IIM (p< 0.05). A trend to a higher complement C3 (p=0.09) and significantly lower C4 (p< 0.05) was observed in IIM compared to HC. Among the individual IIM subsets, there were significant differences in the levels of proteins, vitamin D, and LDH, with the most unfavorable changes in IMNM (p< 0.05). In the total IIM group, changes in the nutrition markers were associated mainly with disease duration, activity (MITAX and serum markers of muscular damage), body mass index (BMI), and the current dose of GC. Levels of proteins negatively correlated with disease activity and the current dose of GC but positively with disease duration, similarly to the levels of vitamin D. Complement C4 and C3 both correlated positively with BMI and negatively with MITAX. Increased levels of insulin and C-peptide were associated with higher BMI and the current dose of GC, while insulin correlated negatively with age (Table 1).
Conclusion: We have observed significant alterations in the serum markers of nutritional status in our IIM patients compared to age-/sex-matched healthy individuals. Differences were also found among the four subtypes of IIM. These alterations were associated with laboratory parameters of disease activity and the current dose of corticosteroids.
Acknowledgment: Supported by AZV NV18-01-00161A, MHCR-00023728, SVV-260523, GAUK 312218
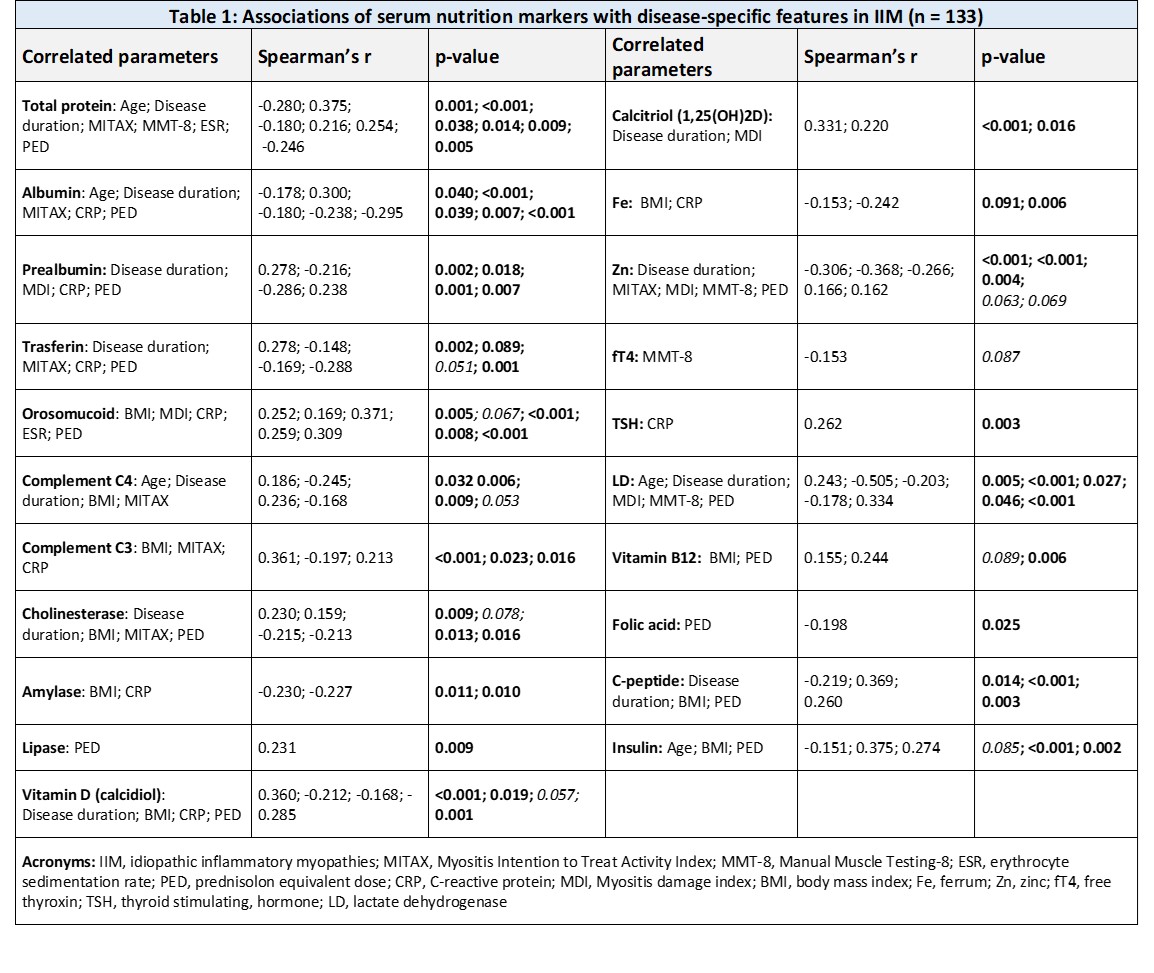 Table 1: Associations of serum nutrition markers with disease-specific features in IIM (n = 133)
Table 1: Associations of serum nutrition markers with disease-specific features in IIM (n = 133)Disclosures: S. Oreská, None; H. Storkanova, None; M. Spiritovic, None; B. Hermankova, None; M. Vrablík, None; K. Pavelka, MSD, Pfizer, Roche, Eli Lilly, Medac, UCB, SOBI, Biogen, Sandoz, Viatris; L. Šenolt, None; H. Mann, None; J. Vencovský, Abbvie, Biogen, Boehringer, Eli Lilly, Gilead, Kezar, Merck, Novartis, Octapharma, Pfizer, Takeda, UCB, Werfen, Argenx; M. Tomcik, None.

