Back
Poster Session A
Diversity, inclusion and racial disparities
Session: (0085–0122) Healthcare Disparities in Rheumatology Poster
0103: Retention in Rheumatology Care and Receipt of Lupus-Specific Serologic Testing Among Young Adults with Systemic Lupus Erythematosus: A Medicare Cohort Study
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall

Maria Schletzbaum, PhD
University of Wisconsin School of Medicine and Public Health
Middleton, WI, United States
Abstract Poster Presenter(s)
Maria Schletzbaum1, W. Ryan Powell2, Shivani Garg3, Joseph A. Kramer4, Brad C. Astor5, Andrea Gilmore-Bykovskyi6, Amy J. Kind7 and Christie Bartels8, 1University of Wisconsin School of Medicine and Public Health, Department of Population Health Sciences, Middleton, WI, 2University of Wisconsin School of Medicine and Public Health, Center for Health Disparities Research, Thousand Oaks, CA, 3University of Madison, School of Medicine and Public Health, Madison, WI, 4University of Wisconsin School of Medicine and Public Health, Department of Medicine & Center for Health Disparities Research,, Madison, WI, 5University of Wisconsin School of Medicine and Public Health, Department of Medicine, Nephrology Division and Department of Population Sciences, Madison, WI, 6University of Wisconsin School of Medicine and Public Health, Department of Emergency Medicine; and the Center for Health Disparities Research, Madison, WI, 7University of Wisconsin School of Medicine and Public Health, Department of Medicine, Geriatrics Division & Center for Health Disparities Research, Madison, WI, 8University of Wisconsin School of Medicine and Public Health, Madison, WI
Background/Purpose: SLE is a leading cause of mortality in young adults, particularly in those identifying as Black or Hispanic or who are socioeconomically disadvantaged. These populations may also experience differential access to lupus care and care quality, which could contribute to existing outcome disparities. Thus, we sought to examine potential disparities in markers of lupus care access and quality in a uniformly insured, national cohort of young adults with lupus who are at particularly high risk for poor outcomes. The objective of this study was to compare visit-based retention in lupus care (marker of access) and receipt of serologic testing (marker of quality) by race and ethnicity, neighborhood socioeconomic disadvantage, and geography.
Methods: This cohort study analyzed a geo-linked 20% national sample of young adult (ages 18-35) Medicare beneficiaries. Inclusion required a hospitalization, rheumatology physician visit, or two other non-hospitalization encounters at least two months apart that were associated with a lupus diagnosis code between January 1, 2013 and June 30, 2014 (98% specificity, 85% sensitivity). Patients had to have 18 months of claims. The first six months were used to establish comorbid conditions. Rheumatology visits and serologic testing were evaluated in a subsequent 12-month assessment period. Visit-based retention in lupus care was defined as a rheumatology visit in both six-month periods of the assessment period. Serologic testing was defined as at least one complement or dsDNA test within the 12 months. Patients were categorized into US census region, quintile of neighborhood disadvantaged based on Area Deprivation Index, and rural, suburban, or urban area. Multivariable logistic regression models were fit for retention and serologic testing.
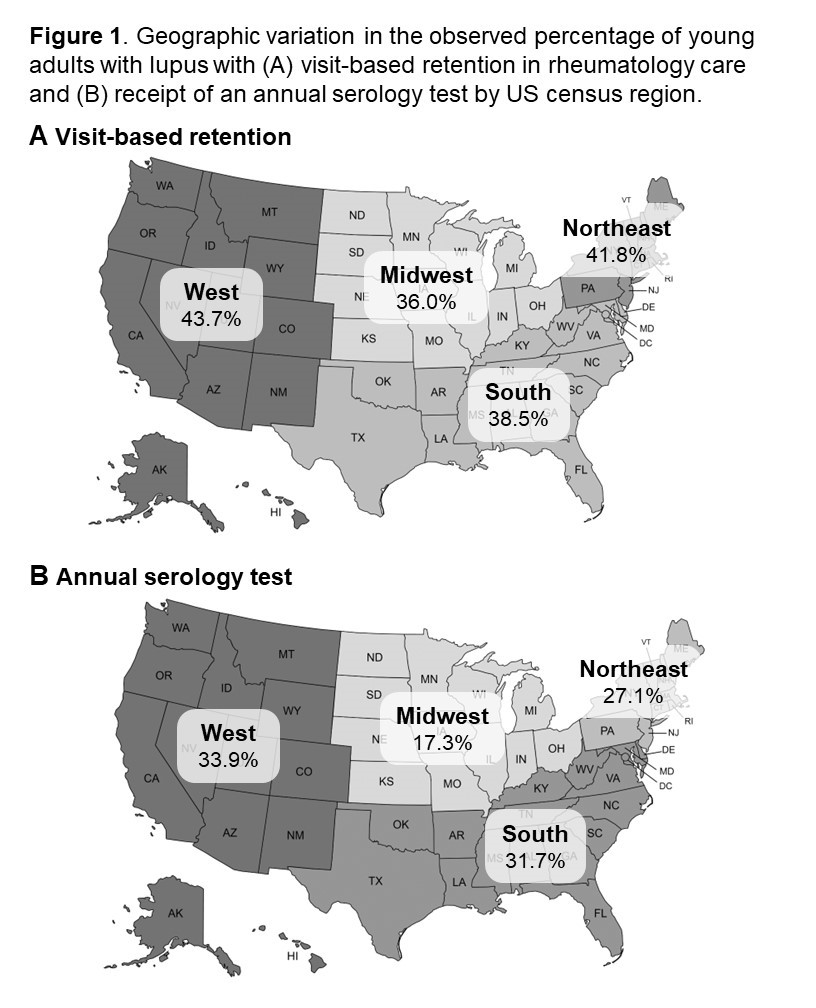
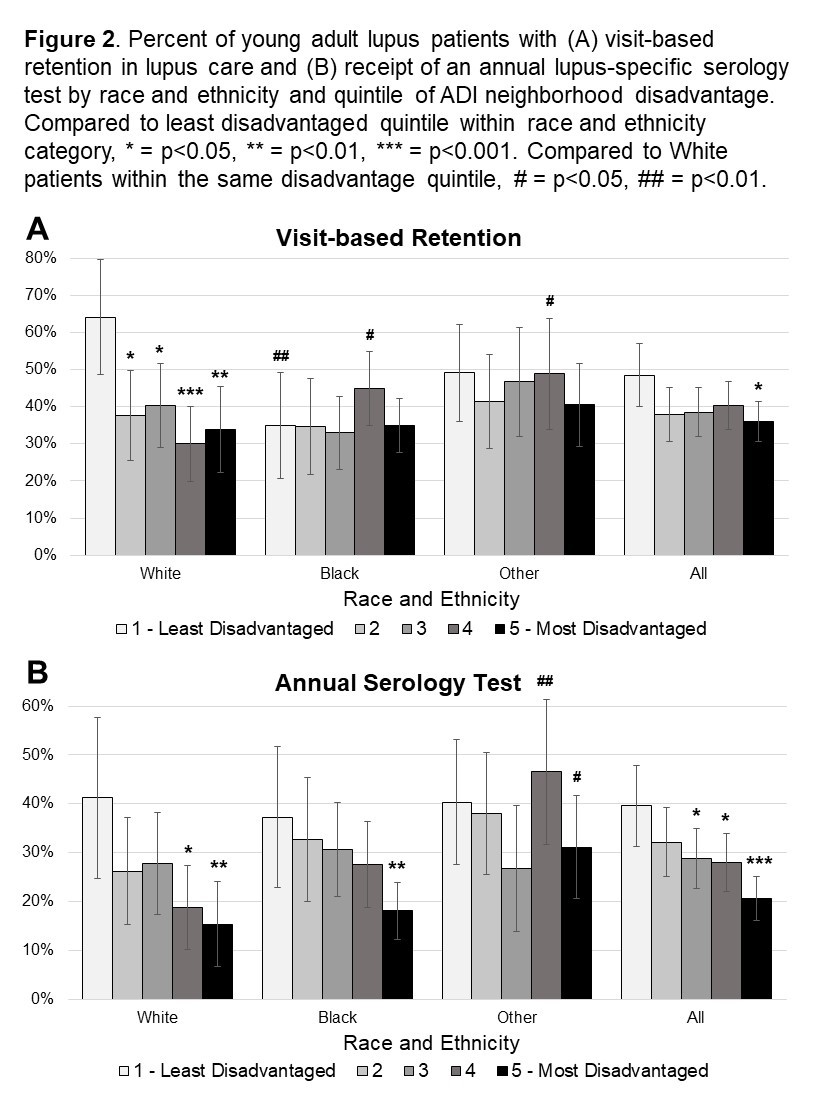
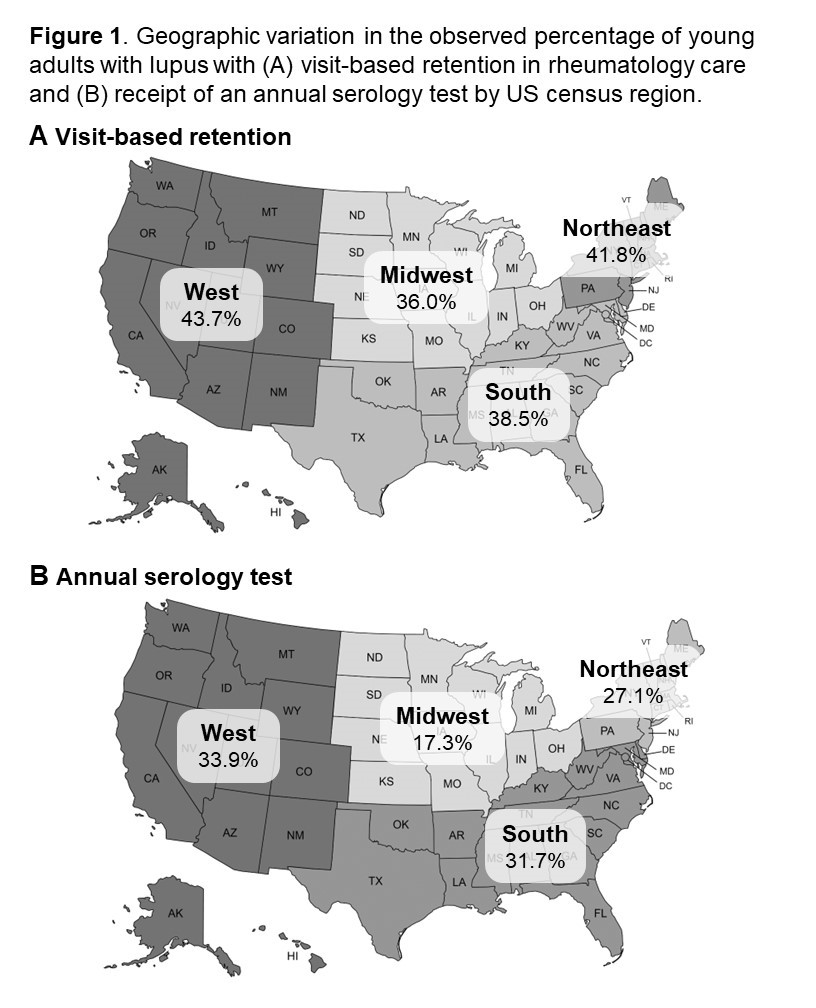
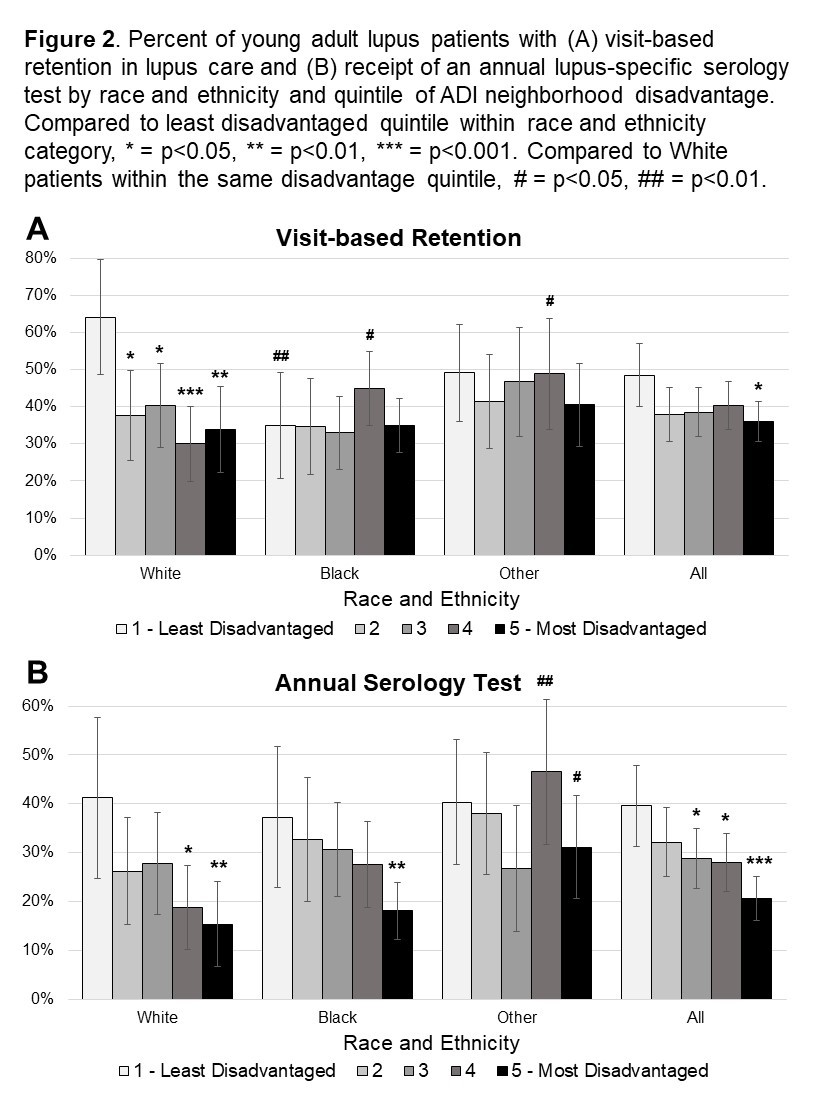
Results: Among 1,036 young adults with lupus (mean age 29), 39% (95% CI 36-42%) had visit-based retention in lupus care, and 28% (95% CI 26-31%) had serologic testing. Both visit-based retention and serologic testing was lowest in the Midwest and highest in the West (Figure 1). No differences were found by rural, suburban, or urban area. White beneficiaries from the least disadvantaged quintile of neighborhoods had ≥15% higher visit-based retention than other beneficiaries (64 vs 30-49%; Figure 2). Serologic testing was lower with higher neighborhood disadvantage (Figure 2), decreasing 19% for each quintile increase in neighborhood disadvantage (aOR 0.81; 95% CI 0.72, 0.91; Table 1). Visit-based retention but not serologic testing, increased with higher comorbidity burden. Presence of primary care visits increased odds of serologic testing two-fold, while rheumatology visits were the strongest predictor (aOR 3.83; 2.44, 6.01).
Conclusion: In this cohort of young adults with lupus, only 39% saw a rheumatologist at least once each six months and fewer than one in three had an annual serologic test. Despite uniform Medicare coverage, disparities in markers of lupus care access and quality were identified by neighborhood disadvantage, race and ethnicity, and region. These findings suggest further research is needed to evaluate additional lupus care quality indicators and how such care differences may impact lupus outcome disparities in the US.
.jpeg)
Disclosures: M. Schletzbaum, None; W. Powell, None; S. Garg, None; J. Kramer, None; B. Astor, None; A. Gilmore-Bykovskyi, None; A. Kind, None; C. Bartels, Pfizer.
Background/Purpose: SLE is a leading cause of mortality in young adults, particularly in those identifying as Black or Hispanic or who are socioeconomically disadvantaged. These populations may also experience differential access to lupus care and care quality, which could contribute to existing outcome disparities. Thus, we sought to examine potential disparities in markers of lupus care access and quality in a uniformly insured, national cohort of young adults with lupus who are at particularly high risk for poor outcomes. The objective of this study was to compare visit-based retention in lupus care (marker of access) and receipt of serologic testing (marker of quality) by race and ethnicity, neighborhood socioeconomic disadvantage, and geography.
Methods: This cohort study analyzed a geo-linked 20% national sample of young adult (ages 18-35) Medicare beneficiaries. Inclusion required a hospitalization, rheumatology physician visit, or two other non-hospitalization encounters at least two months apart that were associated with a lupus diagnosis code between January 1, 2013 and June 30, 2014 (98% specificity, 85% sensitivity). Patients had to have 18 months of claims. The first six months were used to establish comorbid conditions. Rheumatology visits and serologic testing were evaluated in a subsequent 12-month assessment period. Visit-based retention in lupus care was defined as a rheumatology visit in both six-month periods of the assessment period. Serologic testing was defined as at least one complement or dsDNA test within the 12 months. Patients were categorized into US census region, quintile of neighborhood disadvantaged based on Area Deprivation Index, and rural, suburban, or urban area. Multivariable logistic regression models were fit for retention and serologic testing.
Results: Among 1,036 young adults with lupus (mean age 29), 39% (95% CI 36-42%) had visit-based retention in lupus care, and 28% (95% CI 26-31%) had serologic testing. Both visit-based retention and serologic testing was lowest in the Midwest and highest in the West (Figure 1). No differences were found by rural, suburban, or urban area. White beneficiaries from the least disadvantaged quintile of neighborhoods had ≥15% higher visit-based retention than other beneficiaries (64 vs 30-49%; Figure 2). Serologic testing was lower with higher neighborhood disadvantage (Figure 2), decreasing 19% for each quintile increase in neighborhood disadvantage (aOR 0.81; 95% CI 0.72, 0.91; Table 1). Visit-based retention but not serologic testing, increased with higher comorbidity burden. Presence of primary care visits increased odds of serologic testing two-fold, while rheumatology visits were the strongest predictor (aOR 3.83; 2.44, 6.01).
Conclusion: In this cohort of young adults with lupus, only 39% saw a rheumatologist at least once each six months and fewer than one in three had an annual serologic test. Despite uniform Medicare coverage, disparities in markers of lupus care access and quality were identified by neighborhood disadvantage, race and ethnicity, and region. These findings suggest further research is needed to evaluate additional lupus care quality indicators and how such care differences may impact lupus outcome disparities in the US.
.jpeg)
Disclosures: M. Schletzbaum, None; W. Powell, None; S. Garg, None; J. Kramer, None; B. Astor, None; A. Gilmore-Bykovskyi, None; A. Kind, None; C. Bartels, Pfizer.

