Back
Poster Session A
Diversity, inclusion and racial disparities
Session: (0085–0122) Healthcare Disparities in Rheumatology Poster
0116: Racial Differences in Medication Beliefs and Barriers to Taking Medications Among Patients with SLE
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- EG
Emilio Guzman Cisneros, MD
Duke University Internal Medicine Residency
Durham, NC, United States
Abstract Poster Presenter(s)
Emilio Guzman Cisneros1, Shannon Herndon1, Theresa Coles2, Corrine Voils3, Megan Clowse4, Rebecca Sadun4, Jennifer Rogers5, Lisa Criscione-Schreiber2, Jayanth Doss4, Amanda Eudy6 and Kai Sun4, 1Duke University Hospital, Durham, NC, 2Duke University School of Medicine, Durham, NC, 3University of Wisconsin School of Medicine and Public Health, Madison, WI, 4Duke University, Durham, NC, 5Duke, Durham, NC, 6Duke University, Raleigh, NC
Background/Purpose: Medication adherence is critical for SLE management and can be influenced by patients' barriers and beliefs about treatment. Patients of color with SLE have higher rates of medication nonadherence leading to worse health outcomes. However, racial differences in barriers and beliefs about medications have not been well studied. We compared differences in medication beliefs and barriers to taking SLE medications between Black and White patients and explored the association between beliefs and adherence.
Methods: Patients meeting ACR or SLICC SLE criteria from an academic lupus clinic completed the Beliefs about Medicines Questionnaire (BMQ) that measures four domains: disease-specific medication necessity, disease-specific medication concern, general medication overuse, and general medication harm. Participants also completed the SLE-specific Domains of Subjective Extent of Nonadherence (DOSE-Nonadherence-SLE), which has two domains measuring the extent of and reasons for nonadherence over the past 7 days. We compared scores in BMQ and DOSE-Nonadherence-SLE between Black and White patients and explored differences in BMQ scores between adherent and nonadherent patients stratified by race.
Results: The analysis included 125 patients (52% Black, median age 49, 94% female, 59% ≥ college education, 41% Medicaid/Medicare insurance, median disease duration 14 years). Adherence measured by DOSE-Nonadherence-SLE was 64% among White, and 44% among Black participants (p=0.02).
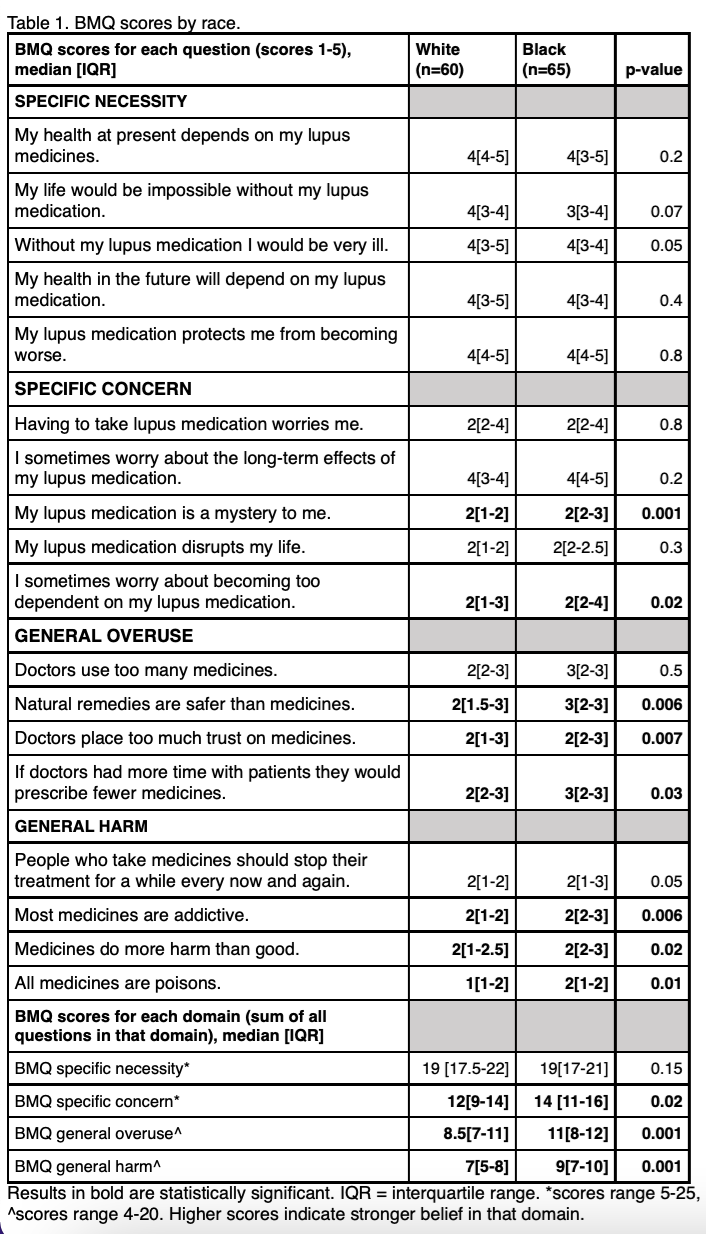
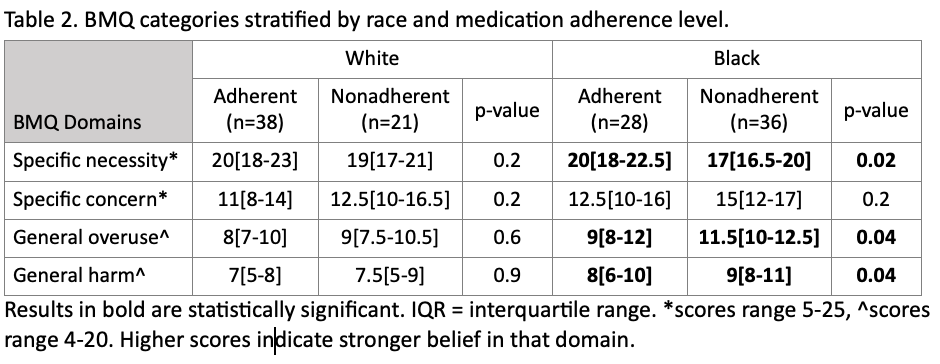
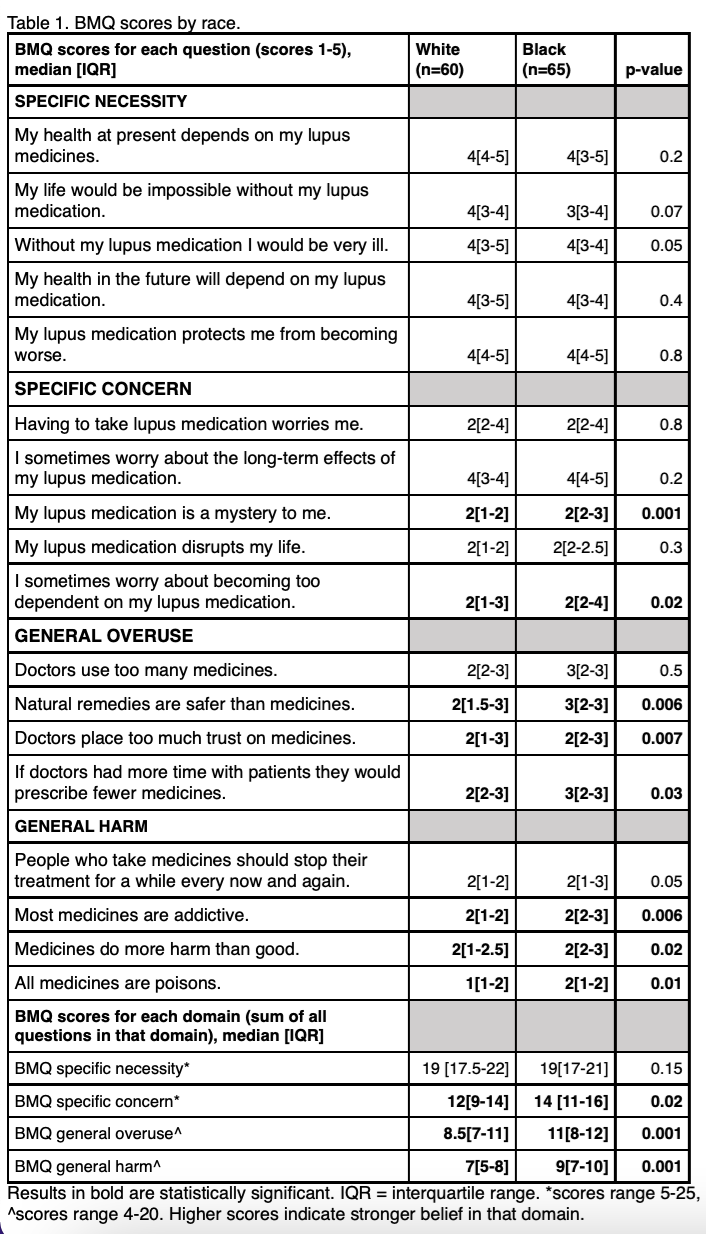
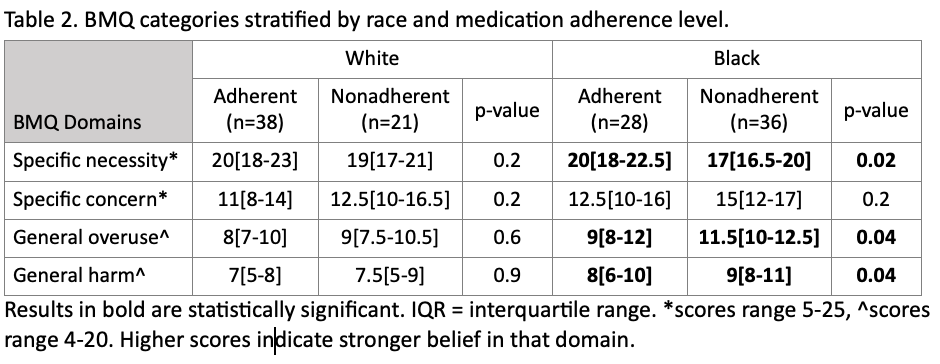
Black compared to White patients had significantly higher scores in BMQ domains of SLE-specific medication concern and general medication overuse and harm (Table 1). There were no significant differences in BMQ scores between adherent and nonadherent White patients. Nonadherent Black patients had significantly lower scores in BMQ SLE-specific necessity and higher scores in BMQ general overuse and harm than adherent Black patients (Table 2).
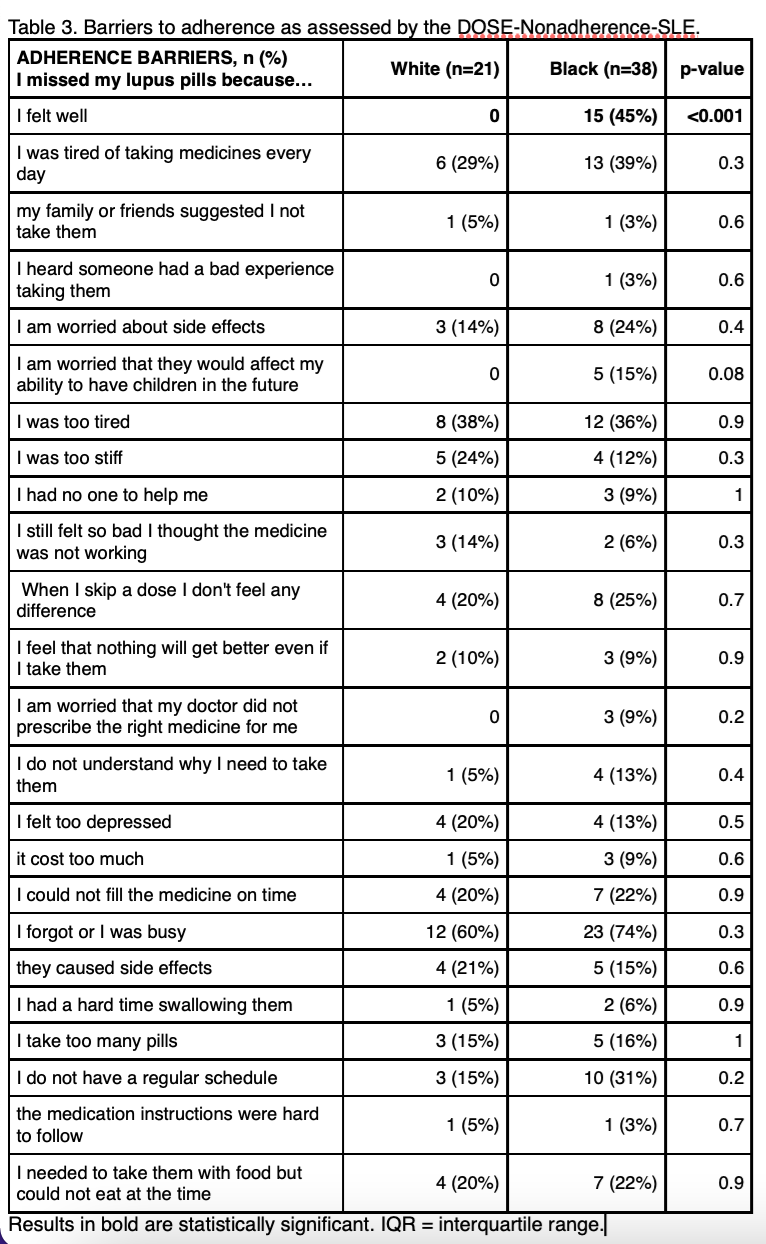
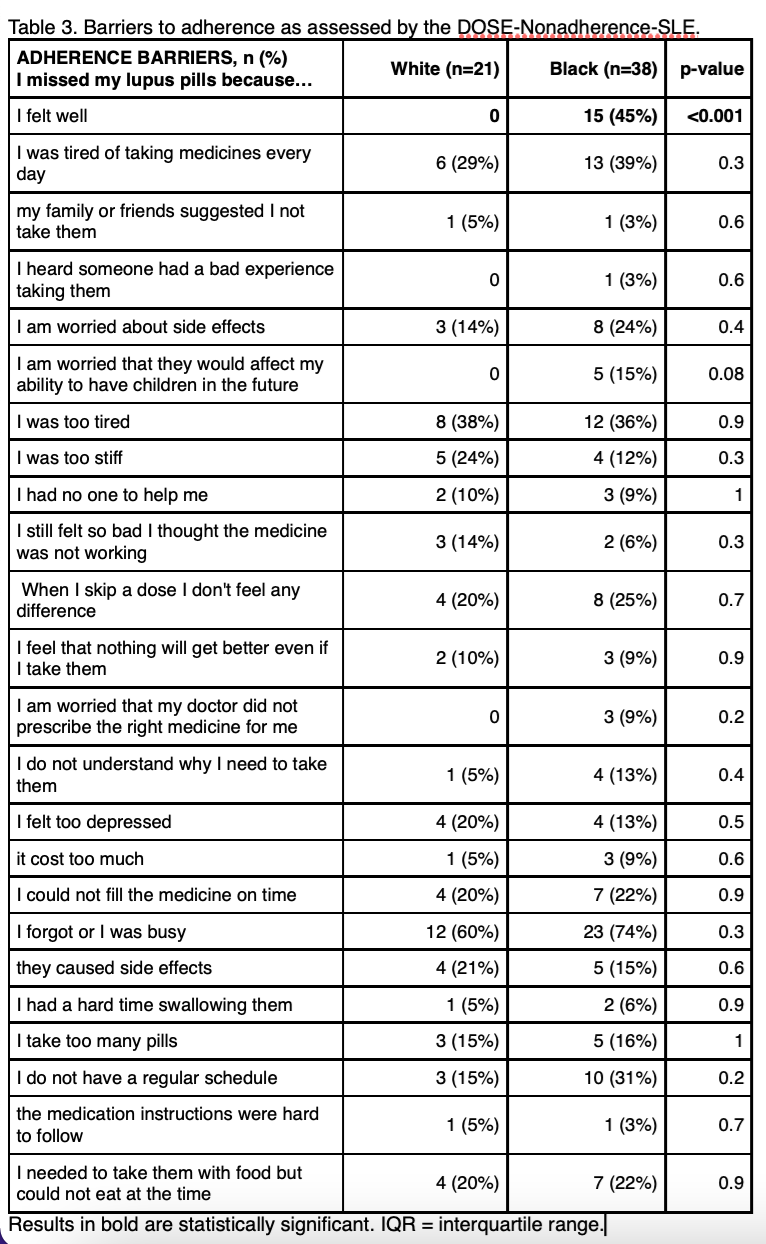
Nonadherent Black patients on average identified four barriers to medication adherence compared to three identified by their White counterparts (p=0.009). Among nonadherent Black patients, 45% reported missing doses because they felt well, compared to 0% of nonadherent White patients (p< 0.001). Additionally, 15% of nonadherent Black patients worried that SLE medicines would affect their fertility, and 9% worried that their doctor did not prescribe the right SLE medicine, while none of these factors were reported by White patients as barriers to adherence (Table 3).
Conclusion: Black patients with SLE were more likely to be nonadherent, have more adherence barriers and greater mistrust about medications. Specifically, nonadherent Black patients held stronger beliefs that medicines were overused and harmful in general, and weaker beliefs that SLE medicines were necessary. These beliefs may reflect a general sense of mistrust in the medical system and may drive the behavior of skipping doses when feeling well and when concerns arise. Our results suggest that adherence interventions among Black patients should include a focus on building trust and an emphasis on ensuring adherence even when the patient feels well.
Disclosures: E. Guzman Cisneros, None; S. Herndon, None; T. Coles, Pfizer, Regenxbio, Merck/MSD; C. Voils, None; M. Clowse, Exagen; R. Sadun, None; J. Rogers, Pfizer, Exagen, Aurinia, Immunovant, Janssen, Eli Lilly; L. Criscione-Schreiber, GlaxoSmithKlein(GSK), UCB; J. Doss, Pfizer; A. Eudy, GlaxoSmithKlein(GSK), Pfizer, Exagen; K. Sun, Exagen.
Background/Purpose: Medication adherence is critical for SLE management and can be influenced by patients' barriers and beliefs about treatment. Patients of color with SLE have higher rates of medication nonadherence leading to worse health outcomes. However, racial differences in barriers and beliefs about medications have not been well studied. We compared differences in medication beliefs and barriers to taking SLE medications between Black and White patients and explored the association between beliefs and adherence.
Methods: Patients meeting ACR or SLICC SLE criteria from an academic lupus clinic completed the Beliefs about Medicines Questionnaire (BMQ) that measures four domains: disease-specific medication necessity, disease-specific medication concern, general medication overuse, and general medication harm. Participants also completed the SLE-specific Domains of Subjective Extent of Nonadherence (DOSE-Nonadherence-SLE), which has two domains measuring the extent of and reasons for nonadherence over the past 7 days. We compared scores in BMQ and DOSE-Nonadherence-SLE between Black and White patients and explored differences in BMQ scores between adherent and nonadherent patients stratified by race.
Results: The analysis included 125 patients (52% Black, median age 49, 94% female, 59% ≥ college education, 41% Medicaid/Medicare insurance, median disease duration 14 years). Adherence measured by DOSE-Nonadherence-SLE was 64% among White, and 44% among Black participants (p=0.02).
Black compared to White patients had significantly higher scores in BMQ domains of SLE-specific medication concern and general medication overuse and harm (Table 1). There were no significant differences in BMQ scores between adherent and nonadherent White patients. Nonadherent Black patients had significantly lower scores in BMQ SLE-specific necessity and higher scores in BMQ general overuse and harm than adherent Black patients (Table 2).
Nonadherent Black patients on average identified four barriers to medication adherence compared to three identified by their White counterparts (p=0.009). Among nonadherent Black patients, 45% reported missing doses because they felt well, compared to 0% of nonadherent White patients (p< 0.001). Additionally, 15% of nonadherent Black patients worried that SLE medicines would affect their fertility, and 9% worried that their doctor did not prescribe the right SLE medicine, while none of these factors were reported by White patients as barriers to adherence (Table 3).
Conclusion: Black patients with SLE were more likely to be nonadherent, have more adherence barriers and greater mistrust about medications. Specifically, nonadherent Black patients held stronger beliefs that medicines were overused and harmful in general, and weaker beliefs that SLE medicines were necessary. These beliefs may reflect a general sense of mistrust in the medical system and may drive the behavior of skipping doses when feeling well and when concerns arise. Our results suggest that adherence interventions among Black patients should include a focus on building trust and an emphasis on ensuring adherence even when the patient feels well.
Disclosures: E. Guzman Cisneros, None; S. Herndon, None; T. Coles, Pfizer, Regenxbio, Merck/MSD; C. Voils, None; M. Clowse, Exagen; R. Sadun, None; J. Rogers, Pfizer, Exagen, Aurinia, Immunovant, Janssen, Eli Lilly; L. Criscione-Schreiber, GlaxoSmithKlein(GSK), UCB; J. Doss, Pfizer; A. Eudy, GlaxoSmithKlein(GSK), Pfizer, Exagen; K. Sun, Exagen.

