Back
Poster Session A
Myopathic rheumatic diseases (polymyositis, dermatomyositis, inclusion body myositis)
Session: (0150–0180) Muscle Biology, Myositis and Myopathies Poster I
0175: Extracorporeal Membrane Oxygenation for Acute Lung Injury in Idiopathic Inflammatory Myopathies – a Potential Lifesaving Intervention
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- BZ
Boyang Zheng, MD
McGill University
Laval, QC, Canada
Abstract Poster Presenter(s)
boyang zheng1, Ellen Eline2, Lilian Xu3, Kun Huang4, Greet Hermans5, michael Perch6, gordan Samoukovic1, ellen De Langhe5, Maryam Dastmalchi7, Lisa Christopher-Stine2, Louise Diederichsen8 and Valerie Leclair1, 1McGill University, Montréal, QC, Canada, 2Johns Hopkins University, Baltimore, MD, 3Johns Hopkins University School of Medicine, Baltimore, MD, 4University of British Columbia, Vancouver, BC, Canada, 5University Hospitals Leuven, Leuven, Belgium, 6Righospitalet, University of Copenhagen, Copenhagen, Denmark, 7Karolinska University Hospital, Stockholm, Sweden, 8Copenhagen University Hospital, Rigshospitalet, Dragør, Denmark
Background/Purpose: Idiopathic inflammatory myopathies (IIM) can present with acute IIM-related lung injury and respiratory failure, leading to a high mortality risk in intensive care units (ICU). Extracorporeal membrane oxygenation (ECMO) is a last resort measure in patients with acute respiratory distress syndrome (ARDS) that can be lifesaving. We aimed to report outcomes of patients with IIM receiving ECMO to better inform clinicians on its use in these diseases.
Methods: Patients diagnosed with IIM from tertiary care centers in Belgium, Canada, Denmark, United States, and Sweden who underwent ECMO were reviewed to identify clinical characteristics and describe disease outcomes and hospitalization course. Clinical characteristics at admission and during ICU stay including ECMO complications and mortality causes were summarized for ICU survivors and those who died. Comorbidity burden was measured using the Charlson Comorbidity Index.
Results: The study included 25 patients (56% female, mean age at admission 47 ± 11 years, median disease duration 3 months [IQR 2, 10]) with dermatomyositis (64%), anti-synthetase syndrome (24%), polymyositis (8%) and overlap myositis (4%) (Table 1). IIM patients had low comorbidity scores and half of them (52%) received immunosuppression before their ICU admission. In the group of patients that survived, 62% were females compared to 44% in the non-survivor group and survivors were younger (44±11 vs 52±10). With regards to in-hospital treatment, 63% of ICU survivors were on >2 immunosuppressors compared to 88% in the non-survivor group. Among the 16 (64%) ICU survivors, 8 (32%) were bridged to transplant and 13 patients (52%) survived beyond 1 year after discharge (Figure 1). When comparing ICU survivors to non-survivors, those who survived were frequently found to have concomitant infections at ICU admission (75% vs 44%) and sepsis (75% vs 56%) (Table 2). Both groups had similar frequencies of ECMO-related complications (38% vs 44%).
Conclusion: ECMO was a lifesaving intervention in a majority of IIM patients presenting with acute IIM-related lung injury. ECMO allowed the necessary time for immunosuppression to take effect, and in some cases, was a bridge to lung transplant in patients who would have otherwise died without intervention.
.jpg) Table 1. Clinical characteristics at hospital admission of IIM patients exposed to ECMO
Table 1. Clinical characteristics at hospital admission of IIM patients exposed to ECMO
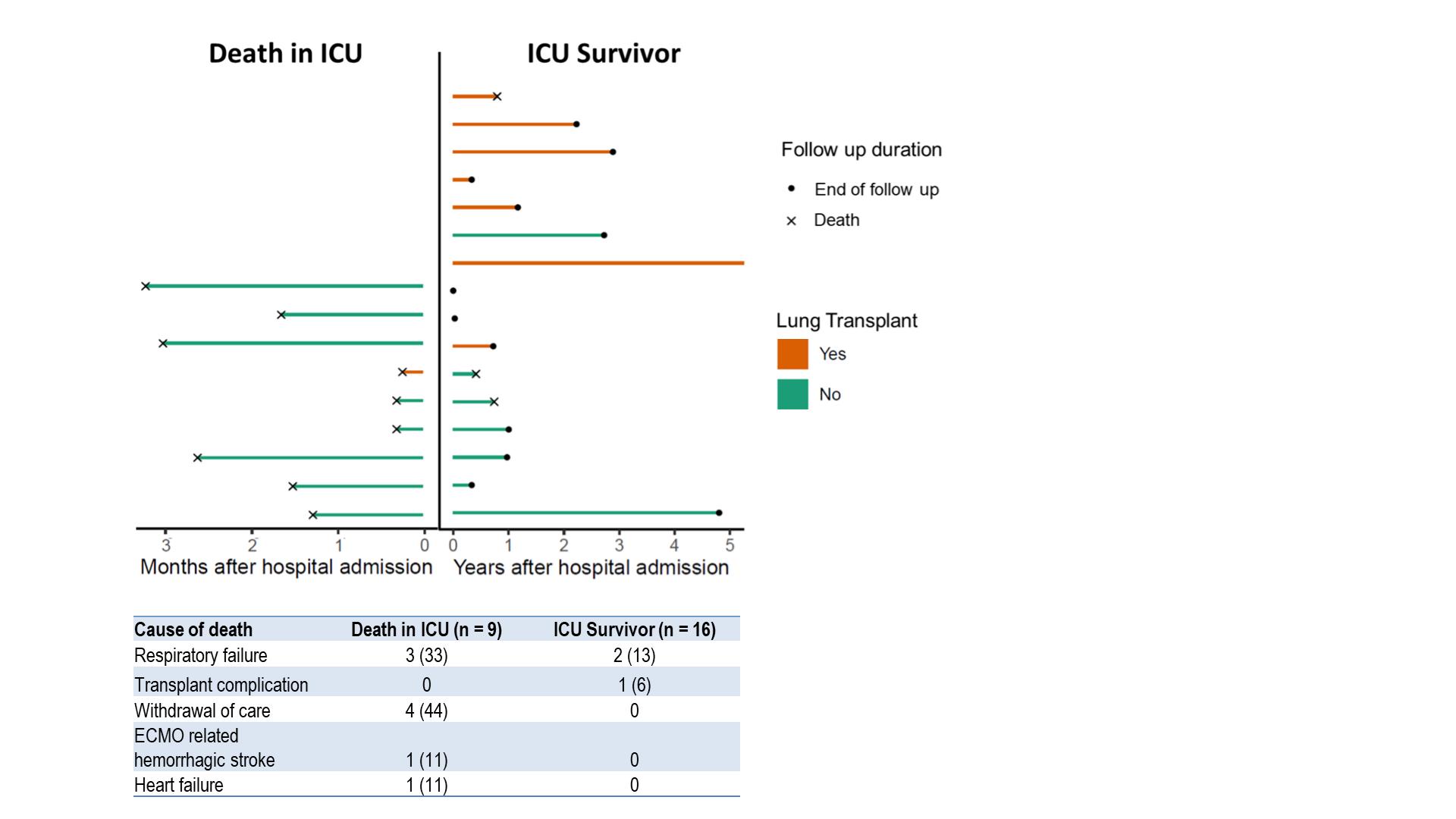 Figure 1. Survival and cause of death in IIM patients exposed to ECMO
Figure 1. Survival and cause of death in IIM patients exposed to ECMO
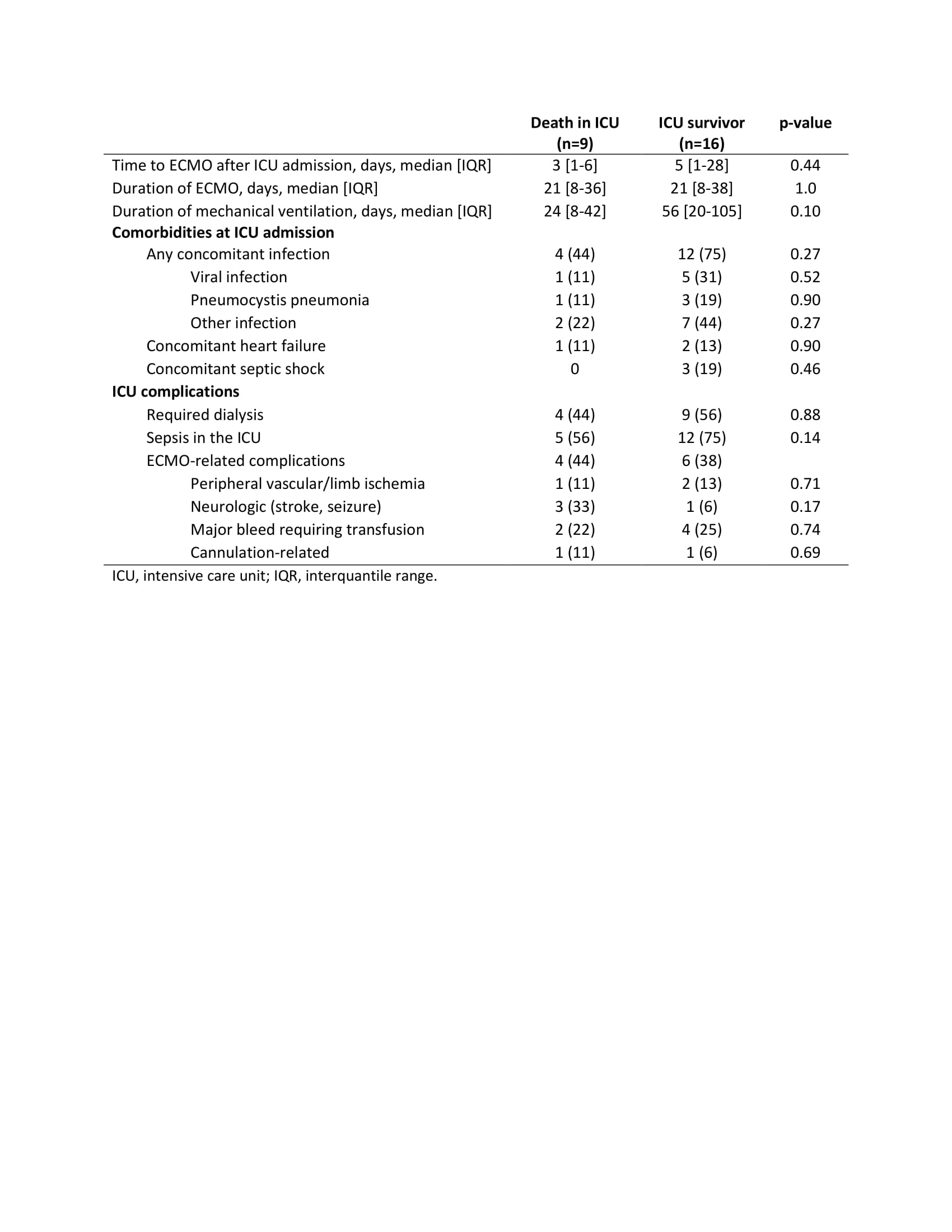 Table 2. ICU outcomes of IIM patients exposed to ECMO
Table 2. ICU outcomes of IIM patients exposed to ECMO
Disclosures: b. zheng, None; E. Eline, None; L. Xu, None; K. Huang, AbbVie/Abbott, Eli Lilly, Janssen, Pfizer; G. Hermans, None; m. Perch, PulmonX, Takeda, Therakos, AMBU, Boeringer-Ingelheim; g. Samoukovic, None; e. De Langhe, None; M. Dastmalchi, None; L. Christopher-Stine, Janssen, Boehringer-Ingelheim, Mallinckroft, EMD-Serono, Allogene, ArgenX; L. Diederichsen, None; V. Leclair, None.
Background/Purpose: Idiopathic inflammatory myopathies (IIM) can present with acute IIM-related lung injury and respiratory failure, leading to a high mortality risk in intensive care units (ICU). Extracorporeal membrane oxygenation (ECMO) is a last resort measure in patients with acute respiratory distress syndrome (ARDS) that can be lifesaving. We aimed to report outcomes of patients with IIM receiving ECMO to better inform clinicians on its use in these diseases.
Methods: Patients diagnosed with IIM from tertiary care centers in Belgium, Canada, Denmark, United States, and Sweden who underwent ECMO were reviewed to identify clinical characteristics and describe disease outcomes and hospitalization course. Clinical characteristics at admission and during ICU stay including ECMO complications and mortality causes were summarized for ICU survivors and those who died. Comorbidity burden was measured using the Charlson Comorbidity Index.
Results: The study included 25 patients (56% female, mean age at admission 47 ± 11 years, median disease duration 3 months [IQR 2, 10]) with dermatomyositis (64%), anti-synthetase syndrome (24%), polymyositis (8%) and overlap myositis (4%) (Table 1). IIM patients had low comorbidity scores and half of them (52%) received immunosuppression before their ICU admission. In the group of patients that survived, 62% were females compared to 44% in the non-survivor group and survivors were younger (44±11 vs 52±10). With regards to in-hospital treatment, 63% of ICU survivors were on >2 immunosuppressors compared to 88% in the non-survivor group. Among the 16 (64%) ICU survivors, 8 (32%) were bridged to transplant and 13 patients (52%) survived beyond 1 year after discharge (Figure 1). When comparing ICU survivors to non-survivors, those who survived were frequently found to have concomitant infections at ICU admission (75% vs 44%) and sepsis (75% vs 56%) (Table 2). Both groups had similar frequencies of ECMO-related complications (38% vs 44%).
Conclusion: ECMO was a lifesaving intervention in a majority of IIM patients presenting with acute IIM-related lung injury. ECMO allowed the necessary time for immunosuppression to take effect, and in some cases, was a bridge to lung transplant in patients who would have otherwise died without intervention.
.jpg) Table 1. Clinical characteristics at hospital admission of IIM patients exposed to ECMO
Table 1. Clinical characteristics at hospital admission of IIM patients exposed to ECMO 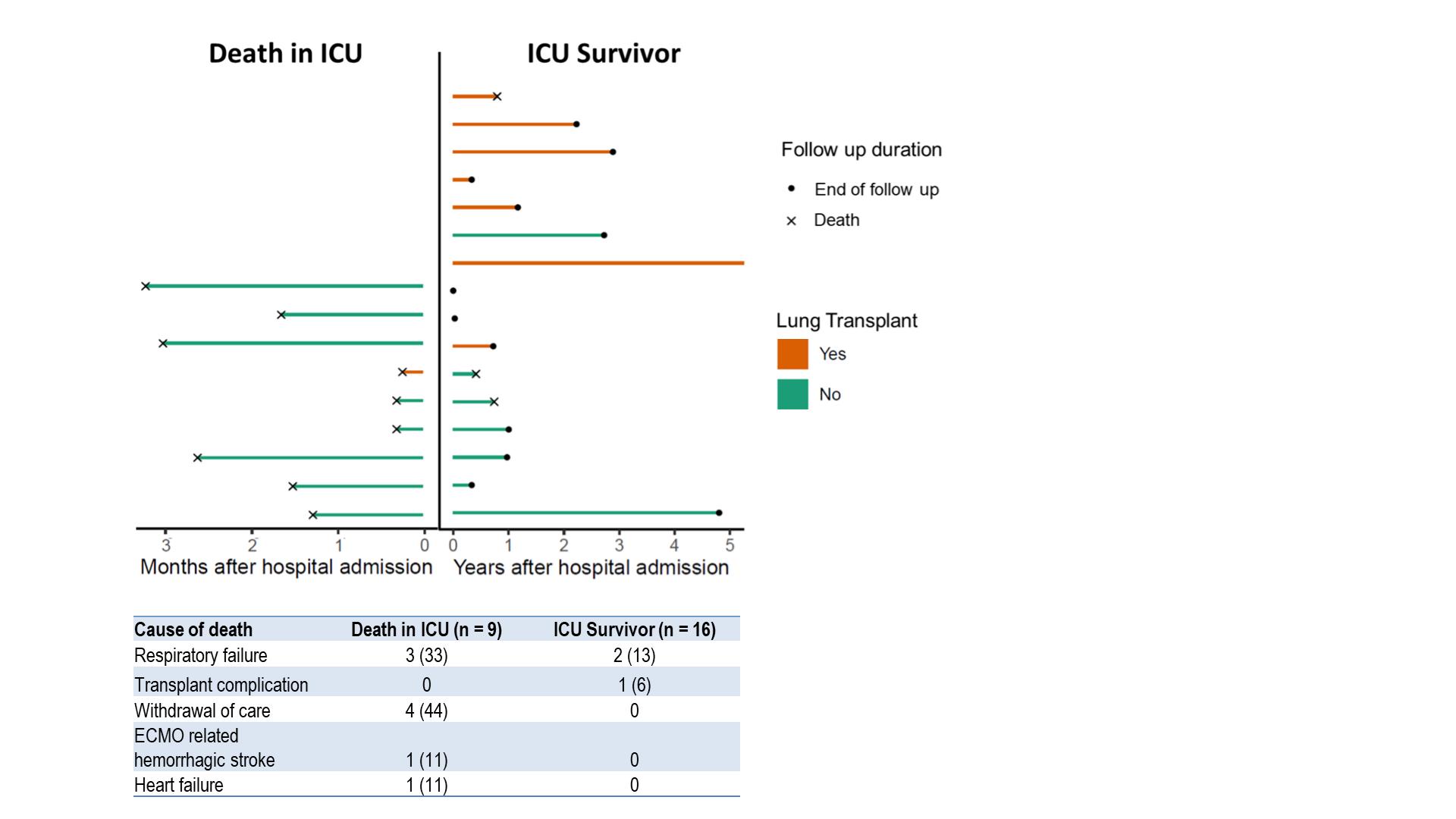 Figure 1. Survival and cause of death in IIM patients exposed to ECMO
Figure 1. Survival and cause of death in IIM patients exposed to ECMO 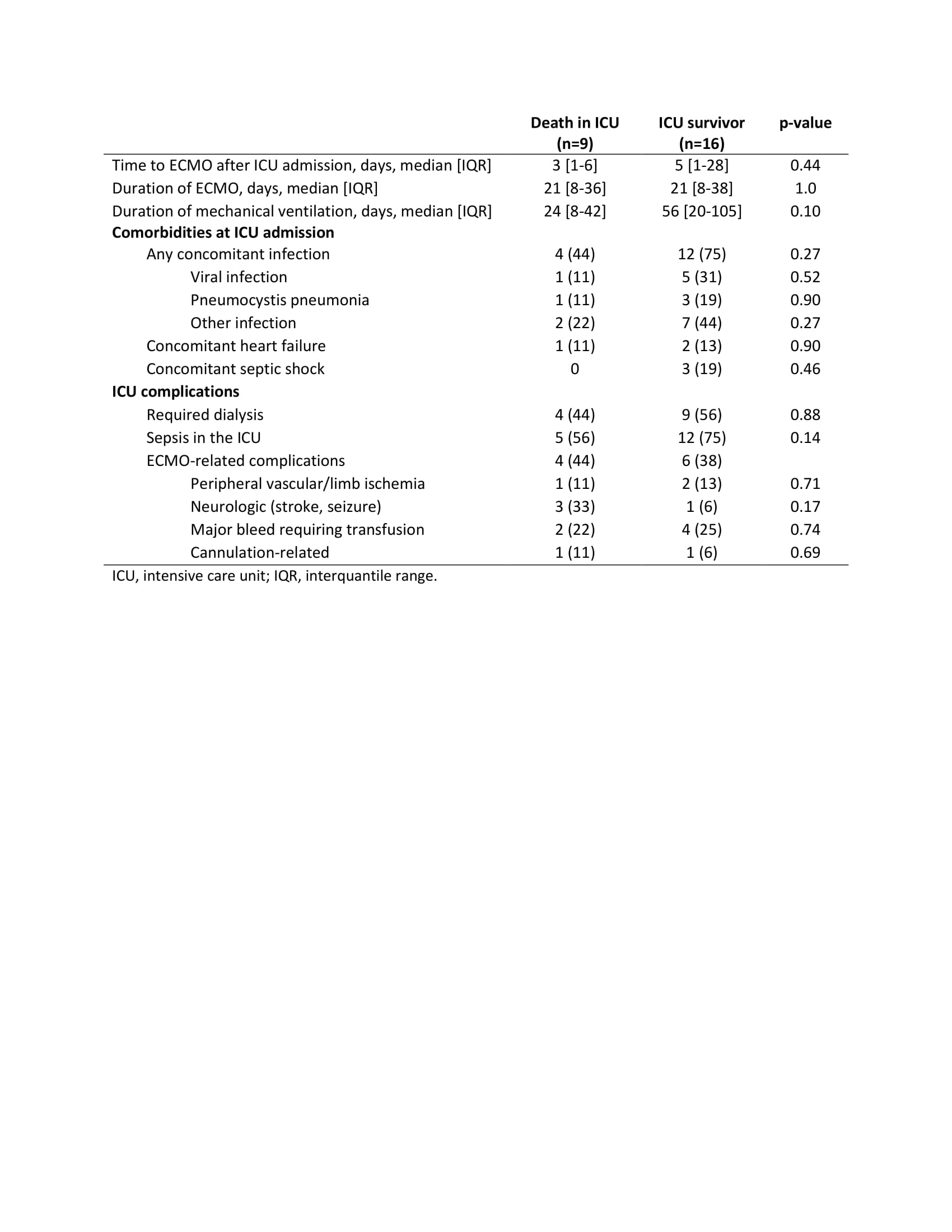 Table 2. ICU outcomes of IIM patients exposed to ECMO
Table 2. ICU outcomes of IIM patients exposed to ECMODisclosures: b. zheng, None; E. Eline, None; L. Xu, None; K. Huang, AbbVie/Abbott, Eli Lilly, Janssen, Pfizer; G. Hermans, None; m. Perch, PulmonX, Takeda, Therakos, AMBU, Boeringer-Ingelheim; g. Samoukovic, None; e. De Langhe, None; M. Dastmalchi, None; L. Christopher-Stine, Janssen, Boehringer-Ingelheim, Mallinckroft, EMD-Serono, Allogene, ArgenX; L. Diederichsen, None; V. Leclair, None.

