Back
Poster Session A
Diversity, inclusion and racial disparities
Session: (0085–0122) Healthcare Disparities in Rheumatology Poster
0087: Does Limited English Proficiency Lead to Additional Health Inequity in Medically Vulnerable Populations in Outpatient Rheumatology?
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- VP
Veena Patel, MD
Dell Medical School - UT Health Austin
Austin, TX, United States
Abstract Poster Presenter(s)
Veena Patel1 and Kevin Hackshaw2, 1Dell Medical School - UT Health Austin, Austin, TX, 2The University of Texas at Austin, Hutto, TX
Background/Purpose: Lack of health insurance and limited English proficiency (LEP) are two factors that can create significant health disparity in the United States which can lead to poor health outcomes, especially for those with chronic medical conditions who have incredibly limited access to specialty care. We reside in Texas, where greater than 20% of our residents are uninsured and 14% are classified as LEP.
To improve access, our rheumatology clinic opened in a federally qualified health center in September 2018. We provide care to uninsured low-income residents who have health care coverage through a charity care program funded by taxpayer dollars in our county. Our division of three rheumatologists are the only in the area who accept this form of coverage.
The purpose of this project is to understand characteristics of an underserved population referred to rheumatology and evaluate if limited English proficiency (LEP) adds additional health inequity for this vulnerable population.
Methods: A retrospective chart review was conducted of all rheumatology referrals from September 2018 to November 2020. We collected demographic data, visit outcomes, disease activity and final diagnoses. Patients with confirmed rheumatologic disease were categorized into two groups: "inflammatory arthritis" (IA) or "connective tissue disease" (CTD) based on respective final diagnosis. Disease activity for these patients was noted by swollen/tender joint count from the physical exam section of the rheumatology clinic note, and overall impression noted in assessment/plan by the evaluating rheumatologist. Disease activity at first visit was then compared between English and LEP patients with rheumatologic disease using Fisher's exact test for IA, CTD and overall.
Results: Six hundred eighty-one patients were seen in rheumatology clinic during our review. Most were female (80%), Hispanic/Latino (67%) and received health care coverage through charity care (67%). Fifty-two percent spoke English as their primary language, 45% spoke Spanish and 3% spoke other languages (Table 1). Four hundred ninety-two patients were newly diagnosed with or confirmed to have rheumatologic disease and seventy-two percent had active disease at initial visit. Of patients with active inflammatory arthritis, 30% (94/312) had erosive disease on initial visit.
LEP patients in our clinic had significantly more active disease at time of initial presentation than English speakers overall (p = 0.0001) and in the CTD subgroup (p = 0.0066) as shown in Figure 1. In the IA subgroup, more LEP patients had active disease compared to English speakers, but this was not statistically significant.
Conclusion: Underserved patients have active, severe disease on presentation to rheumatology clinic. Our study showed that patients with LEP had significantly more active disease than English speakers at initial visit, particularly in connective tissue disease diagnoses. Our next step is to evaluate if disease activity improved over time at similar rates between language groups as patients continue to follow-up with rheumatology. With the LEP and uninsured populations growing, we as a specialty need to find ways to provide care to this population.
.jpg) Demographics of the study population
Demographics of the study population
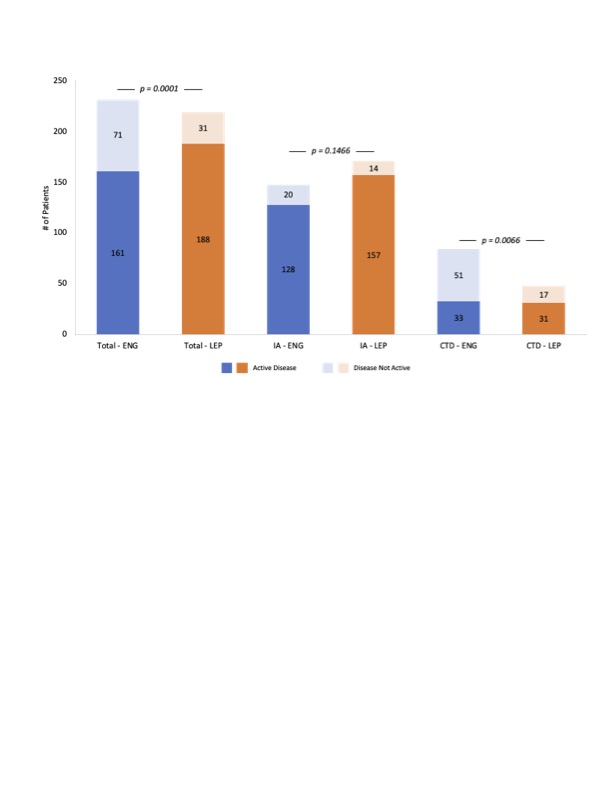 Figure 1. Active disease in English vs. limited English proficiency (LEP) speakers at initial rheumatology visit.
Figure 1. Active disease in English vs. limited English proficiency (LEP) speakers at initial rheumatology visit.
ENG: English speakers; LEP: limited English proficiency; IA: inflammatory arthritis; CTD: connective tissue disease
Disclosures: V. Patel, None; K. Hackshaw, None.
Background/Purpose: Lack of health insurance and limited English proficiency (LEP) are two factors that can create significant health disparity in the United States which can lead to poor health outcomes, especially for those with chronic medical conditions who have incredibly limited access to specialty care. We reside in Texas, where greater than 20% of our residents are uninsured and 14% are classified as LEP.
To improve access, our rheumatology clinic opened in a federally qualified health center in September 2018. We provide care to uninsured low-income residents who have health care coverage through a charity care program funded by taxpayer dollars in our county. Our division of three rheumatologists are the only in the area who accept this form of coverage.
The purpose of this project is to understand characteristics of an underserved population referred to rheumatology and evaluate if limited English proficiency (LEP) adds additional health inequity for this vulnerable population.
Methods: A retrospective chart review was conducted of all rheumatology referrals from September 2018 to November 2020. We collected demographic data, visit outcomes, disease activity and final diagnoses. Patients with confirmed rheumatologic disease were categorized into two groups: "inflammatory arthritis" (IA) or "connective tissue disease" (CTD) based on respective final diagnosis. Disease activity for these patients was noted by swollen/tender joint count from the physical exam section of the rheumatology clinic note, and overall impression noted in assessment/plan by the evaluating rheumatologist. Disease activity at first visit was then compared between English and LEP patients with rheumatologic disease using Fisher's exact test for IA, CTD and overall.
Results: Six hundred eighty-one patients were seen in rheumatology clinic during our review. Most were female (80%), Hispanic/Latino (67%) and received health care coverage through charity care (67%). Fifty-two percent spoke English as their primary language, 45% spoke Spanish and 3% spoke other languages (Table 1). Four hundred ninety-two patients were newly diagnosed with or confirmed to have rheumatologic disease and seventy-two percent had active disease at initial visit. Of patients with active inflammatory arthritis, 30% (94/312) had erosive disease on initial visit.
LEP patients in our clinic had significantly more active disease at time of initial presentation than English speakers overall (p = 0.0001) and in the CTD subgroup (p = 0.0066) as shown in Figure 1. In the IA subgroup, more LEP patients had active disease compared to English speakers, but this was not statistically significant.
Conclusion: Underserved patients have active, severe disease on presentation to rheumatology clinic. Our study showed that patients with LEP had significantly more active disease than English speakers at initial visit, particularly in connective tissue disease diagnoses. Our next step is to evaluate if disease activity improved over time at similar rates between language groups as patients continue to follow-up with rheumatology. With the LEP and uninsured populations growing, we as a specialty need to find ways to provide care to this population.
.jpg) Demographics of the study population
Demographics of the study population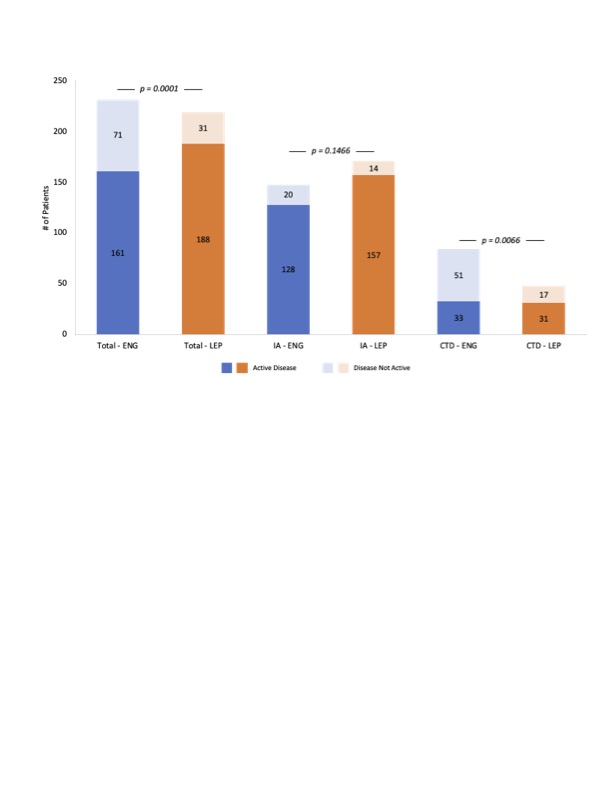 Figure 1. Active disease in English vs. limited English proficiency (LEP) speakers at initial rheumatology visit.
Figure 1. Active disease in English vs. limited English proficiency (LEP) speakers at initial rheumatology visit.ENG: English speakers; LEP: limited English proficiency; IA: inflammatory arthritis; CTD: connective tissue disease
Disclosures: V. Patel, None; K. Hackshaw, None.

