Back
Poster Session A
Rheumatoid arthritis (RA)
Session: (0272–0316) RA – Treatment Poster I
0273: An Update on the Integrated Safety Analysis of Filgotinib in Patients with Moderately to Severely Active RA
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
.png)
Kevin Winthrop
Oregon Health & Science University
portland, OR, United States
Abstract Poster Presenter(s)
Kevin Winthrop1, Daniel Aletaha2, Roberto Felice Caporali3, Yoshiya Tanaka4, Tsutomu Takeuchi5, Paul Van Hoek6, Christopher Watson7, Pieter-Jan Stiers6, Vijay Rajendran8, Katrien Van Beneden6, jacques-eric gottenberg9 and Gerd Burmester10, 1Oregon Health & Science University, Portland, OR, 2Medical University Vienna, Wien, Austria, 3University of Milan, Milano, Italy, 4University of Occupational and Environmental Health, Kitakyusyu Fukuoka, Japan, 5Keio University and Saitama Medical University, Tokyo, Japan, 6Galapagos NV, Mechelen, Belgium, 7Galapagos Biotech Ltd, Cambridge, United Kingdom, 8Galapagos NV, Gent, Belgium, 9Strasbourg University Hospital, Strasbourg, France, 10Charité University Medicine Berlin, Berlin, Germany
Background/Purpose: Filgotinib (FIL) is a second-generation oral Janus kinase 1 preferential inhibitor approved in Europe, Japan, and the UK for treatment of RA.1,2 Over a median treatment duration of 2.2 years, similar incidence of adverse events of special interest (AESIs) were reported for FIL 200 mg (FIL200) and 100 mg (FIL100) dose groups, with the exception of infections, serious infections, and herpes zoster (HZ).3 This analysis provides an update on the safety profile of FIL.
Methods: Integrated FIL RA data from 7 clinical trials are reported: phase 2 (NCT01668641, NCT01894516); phase 3 (NCT02889796, NCT02873936, NCT02886728); and the long-term extension studies, DARWIN 3 phase 2 (NCT02065700) and FINCH 4 phase 3 (NCT03025308). All patients met ACR criteria for functional class I–III. Exposure-adjusted incidence rates (EAIRs)/100 patient-years of exposure (PYE), censored at time of first event, were determined for major adverse cardiovascular event (MACE; including myocardial infarction), venous thromboembolism (VTE), malignancies excluding nonmelanoma skin cancer (NMSC), NMSC, (serious) infections, and deaths. Data were as of Jan 11, 2022 (DARWIN 3) and Jan 31, 2022 (FINCH 4). Analyses were performed on an ad hoc interim analysis data set without additional cleaning; MACE and VTE only include positively adjudicated events with a data cutoff of Nov 30, 2021.
Results: Overall, the as-treated population included 3691 patients with 12,014.1 PYE. Median (max) exposure was 3.59 (8.2) years in the pooled FIL group, 3.69 (8.2) years for FIL200, and 3.15 (7.5) years for FIL100. Baseline demographics and disease characteristics were balanced between treatment groups.4 Small numerical differences were observed between FIL doses for EAIRs of AESIs, except for a higher incidence of HZ with FIL200 (Table). Of 22 treatment-emergent adverse event deaths associated with COVID-19, 1 patient had a record of vaccination. Risk of MACE and VTE was generally stable over time (Figure) with a probability of 1.4% vs 1.2% for FIL100 vs FIL200 for MACE at Week 216 (4 years). Risk of VTE was 0.7% and 0.6% at Week 192 for FIL200 and FIL100, respectively; at 216 weeks the probability of VTE was 1.0% vs 0.7% for FIL100 vs FIL200, although low event numbers make interpretation of any difference difficult. Over 216 weeks (4 years), the risk was generally similar between FIL100 vs FIL200 to develop malignancies excluding NMSC (3.1% vs 2.8%), serious infections (8.2% vs 7.7%) (Figure), or death from any cause (2.3% vs 2.8%) (Figure). The risk of experiencing NMSC was 0.9% vs 1.6% with FIL100 vs FIL200 at Week 216.
Conclusion: Over a median of 3.6 years, both FIL doses continue to show small numerical differences in EAIRs of AESI between FIL100 and FIL200 groups, except for HZ. In this overall RA population, FIL200 showed the highest risk for developing NMSC vs FIL 100, but not for MACE, malignancies excluding NMSC, serious infections, or death. Assessing risk between both doses for VTE was difficult due to low numbers.
References1. Jyseleca SmPC. Galapagos NV; May 2022
2. Jyseleca Japanese PI. Gilead Sciences K.K.; Sep 2020
3. Winthrop KL, et al. Arthritis Rheumatol 2021;73(S10):abstract 1698
4. Winthrop KL, et al. Ann Rheum Dis 2022;81:184–92
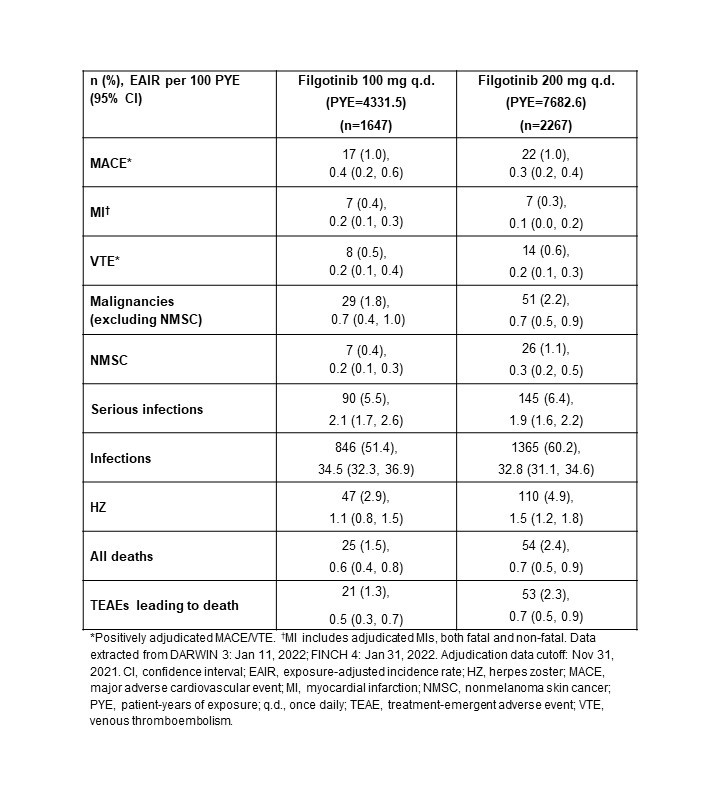 Table. Frequencies and EAIRs of adverse events of special interest in pooled parent and ongoing long-term extension clinical RA trials
Table. Frequencies and EAIRs of adverse events of special interest in pooled parent and ongoing long-term extension clinical RA trials
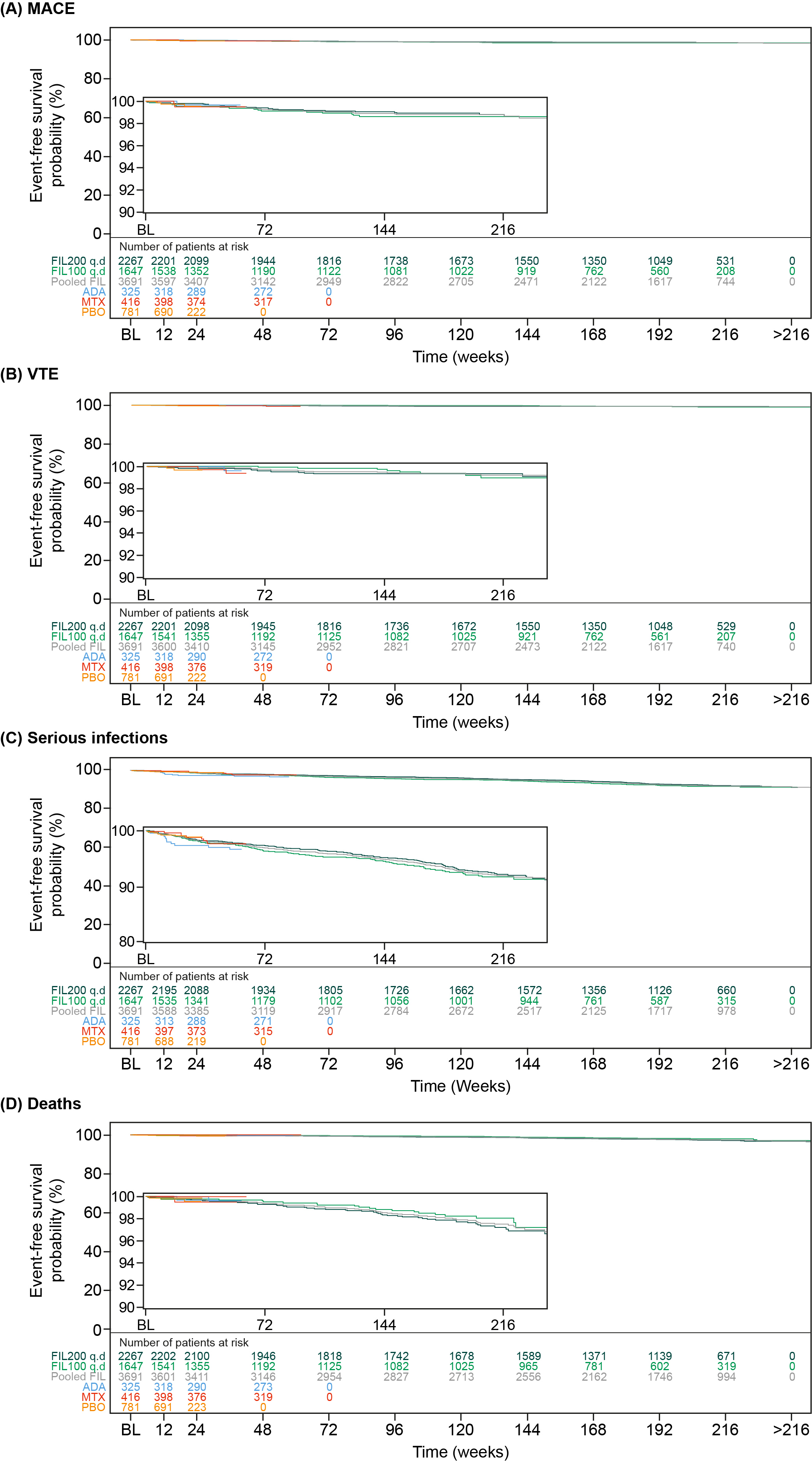 Figure. Event-free probability of (A) MACE, (B) VTE, (C) serious infection, and (D) death from any cause. Time to event was calculated as (onset date of first event – first dose date) + 1. The population was as-treated, including patients who received ≥1 dose of any study drug. A patient may contribute to ≥1 treatment group summary if the patient received ≥1 treatment of interest. Number of patients at risk = number of patients at risk at that the given time point. ADA, adalimumab; BL, baseline; FIL200/100, filgotinib 200/100 mg; MACE, major adverse cardiovascular event; PBO, placebo; q.d., once daily; VTE, venous thromboembolism. Numbers of patients assessed at each time point are shown below each graph.
Figure. Event-free probability of (A) MACE, (B) VTE, (C) serious infection, and (D) death from any cause. Time to event was calculated as (onset date of first event – first dose date) + 1. The population was as-treated, including patients who received ≥1 dose of any study drug. A patient may contribute to ≥1 treatment group summary if the patient received ≥1 treatment of interest. Number of patients at risk = number of patients at risk at that the given time point. ADA, adalimumab; BL, baseline; FIL200/100, filgotinib 200/100 mg; MACE, major adverse cardiovascular event; PBO, placebo; q.d., once daily; VTE, venous thromboembolism. Numbers of patients assessed at each time point are shown below each graph.
Disclosures: K. Winthrop, AbbVie, Bristol Myers Squibb, Eli Lilly, Galapagos, Gilead, GSK, Pfizer, Roche, Regeneron, Sanofi, UCB, AstraZeneca, Novartis; D. Aletaha, Novartis, SoBi, Sanofi, Amgen, Lilly, Merck, Pfizer, Roche, Sandoz, Janssen, AbbVie; R. Caporali, AbbVie, Celltrion, Fresenius-Kabi, Galapagos, Janssen, Pfizer, Roche, UCB, Eli Lilly, Gilead, Sanofi; Y. Tanaka, Lilly, AbbVie, Bristol Myers Squibb, Chugai, Daiichi Sankyo, Eisai, Pfizer, Mitsubishi Tanabe, GlaxoSmithKline, Asahi Kasei, Takeda, Astellas, Janssen, Novartis, Sanofi, UCB, YL Biologics, MSD, Ono, Taisho Toyama, Celltrion, Gilead, Boehringer-Ingelheim, Corrona, Kowa, Amgen, AstraZeneca, AstraZeneca, Eli Lilly; T. Takeuchi, Astellas Pharma, Eli Lilly Japan, Gilead Sciences, AbbVie, Eisai Co., Ltd, Pfizer Japan Inc., Asahi Kasei, Chugai, Daiichi Sankyo, Dainippon Sumitomo Eisai, Mitsubishi-Tanabe, Shionogi, Takeda, UCB Japan, Ayumi Pharmaceutical Corporation, Bristol-Myers Squibb, Novartis, Sanofi; P. Van Hoek, Galapagos; C. Watson, Galapagos; P. Stiers, Galapagos; V. Rajendran, Galapagos; K. Van Beneden, Galapagos; j. gottenberg, AbbVie, Bristol Myers Squibb, Galapagos, Gilead, Lilly, MSD, Novartis, Pfizer; G. Burmester, AbbVie, Galapagos, Lilly, MSD, Pfizer, Roche, UCB, Janssen, Gilead Sciences, Inc..
Background/Purpose: Filgotinib (FIL) is a second-generation oral Janus kinase 1 preferential inhibitor approved in Europe, Japan, and the UK for treatment of RA.1,2 Over a median treatment duration of 2.2 years, similar incidence of adverse events of special interest (AESIs) were reported for FIL 200 mg (FIL200) and 100 mg (FIL100) dose groups, with the exception of infections, serious infections, and herpes zoster (HZ).3 This analysis provides an update on the safety profile of FIL.
Methods: Integrated FIL RA data from 7 clinical trials are reported: phase 2 (NCT01668641, NCT01894516); phase 3 (NCT02889796, NCT02873936, NCT02886728); and the long-term extension studies, DARWIN 3 phase 2 (NCT02065700) and FINCH 4 phase 3 (NCT03025308). All patients met ACR criteria for functional class I–III. Exposure-adjusted incidence rates (EAIRs)/100 patient-years of exposure (PYE), censored at time of first event, were determined for major adverse cardiovascular event (MACE; including myocardial infarction), venous thromboembolism (VTE), malignancies excluding nonmelanoma skin cancer (NMSC), NMSC, (serious) infections, and deaths. Data were as of Jan 11, 2022 (DARWIN 3) and Jan 31, 2022 (FINCH 4). Analyses were performed on an ad hoc interim analysis data set without additional cleaning; MACE and VTE only include positively adjudicated events with a data cutoff of Nov 30, 2021.
Results: Overall, the as-treated population included 3691 patients with 12,014.1 PYE. Median (max) exposure was 3.59 (8.2) years in the pooled FIL group, 3.69 (8.2) years for FIL200, and 3.15 (7.5) years for FIL100. Baseline demographics and disease characteristics were balanced between treatment groups.4 Small numerical differences were observed between FIL doses for EAIRs of AESIs, except for a higher incidence of HZ with FIL200 (Table). Of 22 treatment-emergent adverse event deaths associated with COVID-19, 1 patient had a record of vaccination. Risk of MACE and VTE was generally stable over time (Figure) with a probability of 1.4% vs 1.2% for FIL100 vs FIL200 for MACE at Week 216 (4 years). Risk of VTE was 0.7% and 0.6% at Week 192 for FIL200 and FIL100, respectively; at 216 weeks the probability of VTE was 1.0% vs 0.7% for FIL100 vs FIL200, although low event numbers make interpretation of any difference difficult. Over 216 weeks (4 years), the risk was generally similar between FIL100 vs FIL200 to develop malignancies excluding NMSC (3.1% vs 2.8%), serious infections (8.2% vs 7.7%) (Figure), or death from any cause (2.3% vs 2.8%) (Figure). The risk of experiencing NMSC was 0.9% vs 1.6% with FIL100 vs FIL200 at Week 216.
Conclusion: Over a median of 3.6 years, both FIL doses continue to show small numerical differences in EAIRs of AESI between FIL100 and FIL200 groups, except for HZ. In this overall RA population, FIL200 showed the highest risk for developing NMSC vs FIL 100, but not for MACE, malignancies excluding NMSC, serious infections, or death. Assessing risk between both doses for VTE was difficult due to low numbers.
References1. Jyseleca SmPC. Galapagos NV; May 2022
2. Jyseleca Japanese PI. Gilead Sciences K.K.; Sep 2020
3. Winthrop KL, et al. Arthritis Rheumatol 2021;73(S10):abstract 1698
4. Winthrop KL, et al. Ann Rheum Dis 2022;81:184–92
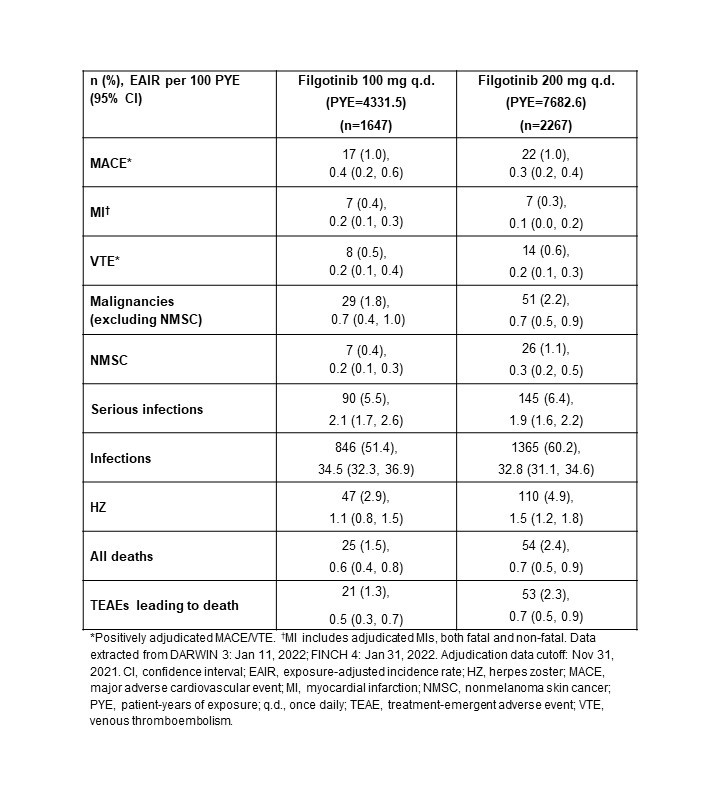 Table. Frequencies and EAIRs of adverse events of special interest in pooled parent and ongoing long-term extension clinical RA trials
Table. Frequencies and EAIRs of adverse events of special interest in pooled parent and ongoing long-term extension clinical RA trials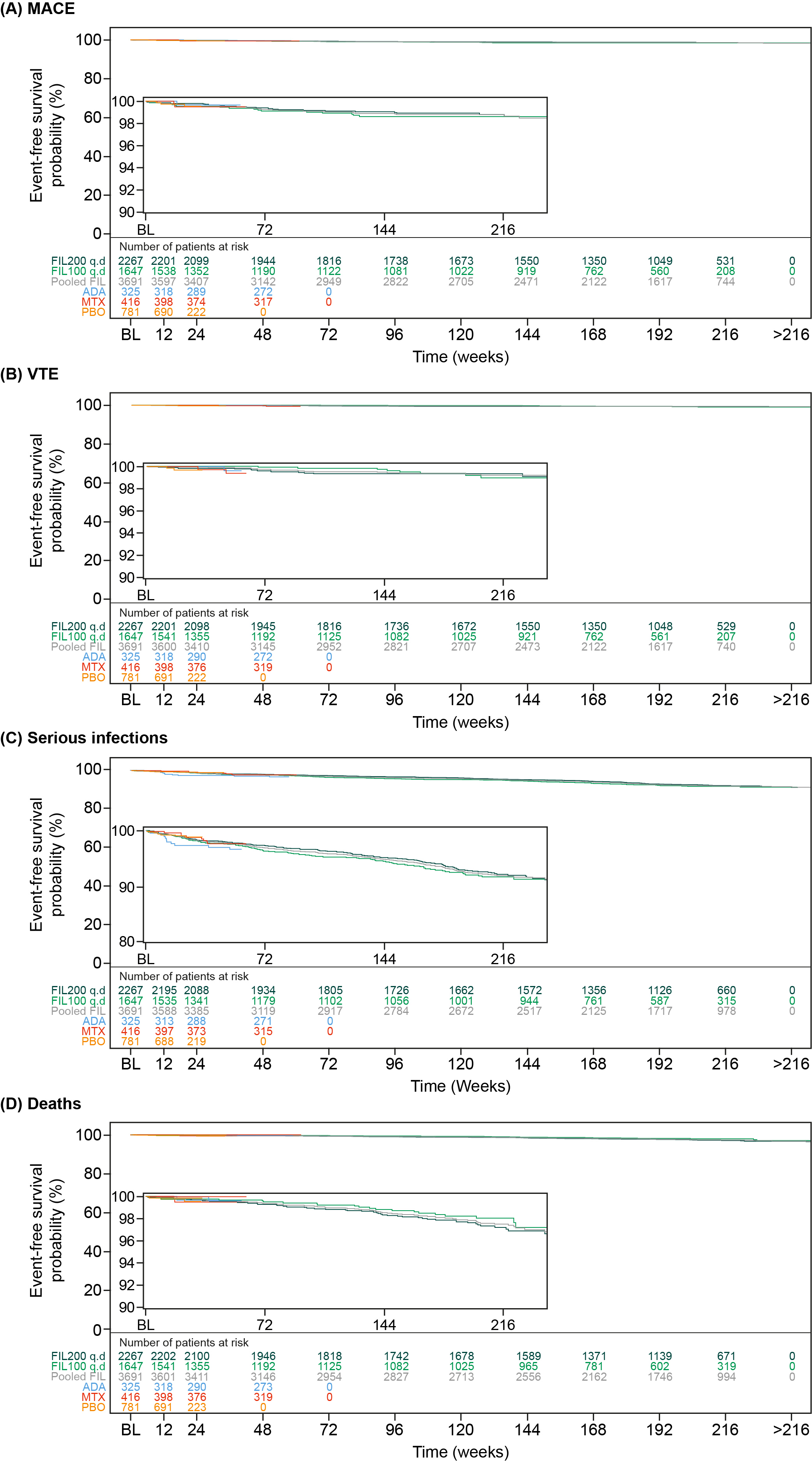 Figure. Event-free probability of (A) MACE, (B) VTE, (C) serious infection, and (D) death from any cause. Time to event was calculated as (onset date of first event – first dose date) + 1. The population was as-treated, including patients who received ≥1 dose of any study drug. A patient may contribute to ≥1 treatment group summary if the patient received ≥1 treatment of interest. Number of patients at risk = number of patients at risk at that the given time point. ADA, adalimumab; BL, baseline; FIL200/100, filgotinib 200/100 mg; MACE, major adverse cardiovascular event; PBO, placebo; q.d., once daily; VTE, venous thromboembolism. Numbers of patients assessed at each time point are shown below each graph.
Figure. Event-free probability of (A) MACE, (B) VTE, (C) serious infection, and (D) death from any cause. Time to event was calculated as (onset date of first event – first dose date) + 1. The population was as-treated, including patients who received ≥1 dose of any study drug. A patient may contribute to ≥1 treatment group summary if the patient received ≥1 treatment of interest. Number of patients at risk = number of patients at risk at that the given time point. ADA, adalimumab; BL, baseline; FIL200/100, filgotinib 200/100 mg; MACE, major adverse cardiovascular event; PBO, placebo; q.d., once daily; VTE, venous thromboembolism. Numbers of patients assessed at each time point are shown below each graph.Disclosures: K. Winthrop, AbbVie, Bristol Myers Squibb, Eli Lilly, Galapagos, Gilead, GSK, Pfizer, Roche, Regeneron, Sanofi, UCB, AstraZeneca, Novartis; D. Aletaha, Novartis, SoBi, Sanofi, Amgen, Lilly, Merck, Pfizer, Roche, Sandoz, Janssen, AbbVie; R. Caporali, AbbVie, Celltrion, Fresenius-Kabi, Galapagos, Janssen, Pfizer, Roche, UCB, Eli Lilly, Gilead, Sanofi; Y. Tanaka, Lilly, AbbVie, Bristol Myers Squibb, Chugai, Daiichi Sankyo, Eisai, Pfizer, Mitsubishi Tanabe, GlaxoSmithKline, Asahi Kasei, Takeda, Astellas, Janssen, Novartis, Sanofi, UCB, YL Biologics, MSD, Ono, Taisho Toyama, Celltrion, Gilead, Boehringer-Ingelheim, Corrona, Kowa, Amgen, AstraZeneca, AstraZeneca, Eli Lilly; T. Takeuchi, Astellas Pharma, Eli Lilly Japan, Gilead Sciences, AbbVie, Eisai Co., Ltd, Pfizer Japan Inc., Asahi Kasei, Chugai, Daiichi Sankyo, Dainippon Sumitomo Eisai, Mitsubishi-Tanabe, Shionogi, Takeda, UCB Japan, Ayumi Pharmaceutical Corporation, Bristol-Myers Squibb, Novartis, Sanofi; P. Van Hoek, Galapagos; C. Watson, Galapagos; P. Stiers, Galapagos; V. Rajendran, Galapagos; K. Van Beneden, Galapagos; j. gottenberg, AbbVie, Bristol Myers Squibb, Galapagos, Gilead, Lilly, MSD, Novartis, Pfizer; G. Burmester, AbbVie, Galapagos, Lilly, MSD, Pfizer, Roche, UCB, Janssen, Gilead Sciences, Inc..

