Back
Poster Session A
Epidemiology, health policy and outcomes
Session: (0056–0084) Health Services Research Poster I: Lupus, RA, Spondyloarthritis and More
0063: Implementability of a SLE Medication Adherence Intervention
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- KS
Kai Sun, MD, MS, RhMSUS
Duke University
Durham, NC, United States
Abstract Poster Presenter(s)
Kai Sun1, Nneka Molokwu2, Amy Corneli1, Kathryn Pollak1, Alexandria Bennion2, Jennifer L Rogers3, Rebecca Sadun2, Lisa Criscione-Schreiber1, Jayanth Doss2, Amanda Eudy4, Hayden Bosworth1 and Megan Clowse2, 1Duke University School of Medicine, Durham, NC, 2Duke University, Durham, NC, 3Duke University School of Medicine, Division of Rheumatology & Immunology, Durham, NC, 4Duke University, Raleigh, NC
Background/Purpose: Medication nonadherence in SLE is common and negatively impacts patient outcomes. Yet, little is known about how to improve medication adherence in patients with SLE. We developed a provider-led adherence intervention with the goals of identifying nonadherence, improving patient-provider communication, and facilitating logistics and increasing motivation for taking SLE medications. The intervention encourages providers to review real-time refill data with patients; use communication strategies such as validating the patient's experiences, providing positive reinforcement, and asking open-ended and nonjudgmental questions to encourage discussion; and address identified adherence barriers (Figure 1). Prior pilot testing showed 10% improvement in medication adherence after one visit, and results from provider and patient surveys supported intervention feasibility and acceptability. In the current study, we examined provider fidelity, time spent, and quality of patient-provider communication during the adherence intervention to identify areas for improvement and to inform implementation.
Methods: All providers in an academic lupus clinic were asked to implement the intervention. With patients' consent, we audio recorded patient encounters during which the adherence intervention was performed. Patients were eligible if they were prescribed SLE-specific medications and had a medication possession ratio < 80% based on pharmacy refill information in the past 3 months. During analysis, we coded whether the clinician shared refill data with the patient, asked open-ended questions regarding adherence, made nonjudgmental statements to normalize missing doses or recognize difficulty taking medications, and used positive reinforcement, such as praising patients for good behaviors observed. Following their clinic visit, patients were invited to participate in in-depth individual interviews about their experiences with the adherence intervention. The interviews were audio-recorded and analyzed using applied thematic analysis.
Results: We recorded and analyzed 24 encounters among six lupus clinic physicians. Patients' median age was 37, 100% were female, and 75% were Black. Physicians reviewed refill information with patients in 20 encounters, used positive reinforcement in 21, validated the patient in 17, and asked open-ended questions in 11. On average, clinicians spent 3.9 minutes discussing medication adherence.
We interviewed 15 patients. All felt that the amount of time spent discussing lupus medications was "just right" except for one who felt that it was slightly long in the context of an otherwise short visit. Nearly all patients described having a positive experience with the adherence intervention.
Conclusion: We provide additional evidence to support the feasibility of incorporating the adherence intervention into routine clinical care and acceptability by patients. We also found an opportunity to improve provider training in asking open-ended questions and using patient validation when communicating with patients about medication adherence. Future work should test the intervention in a larger controlled setting.
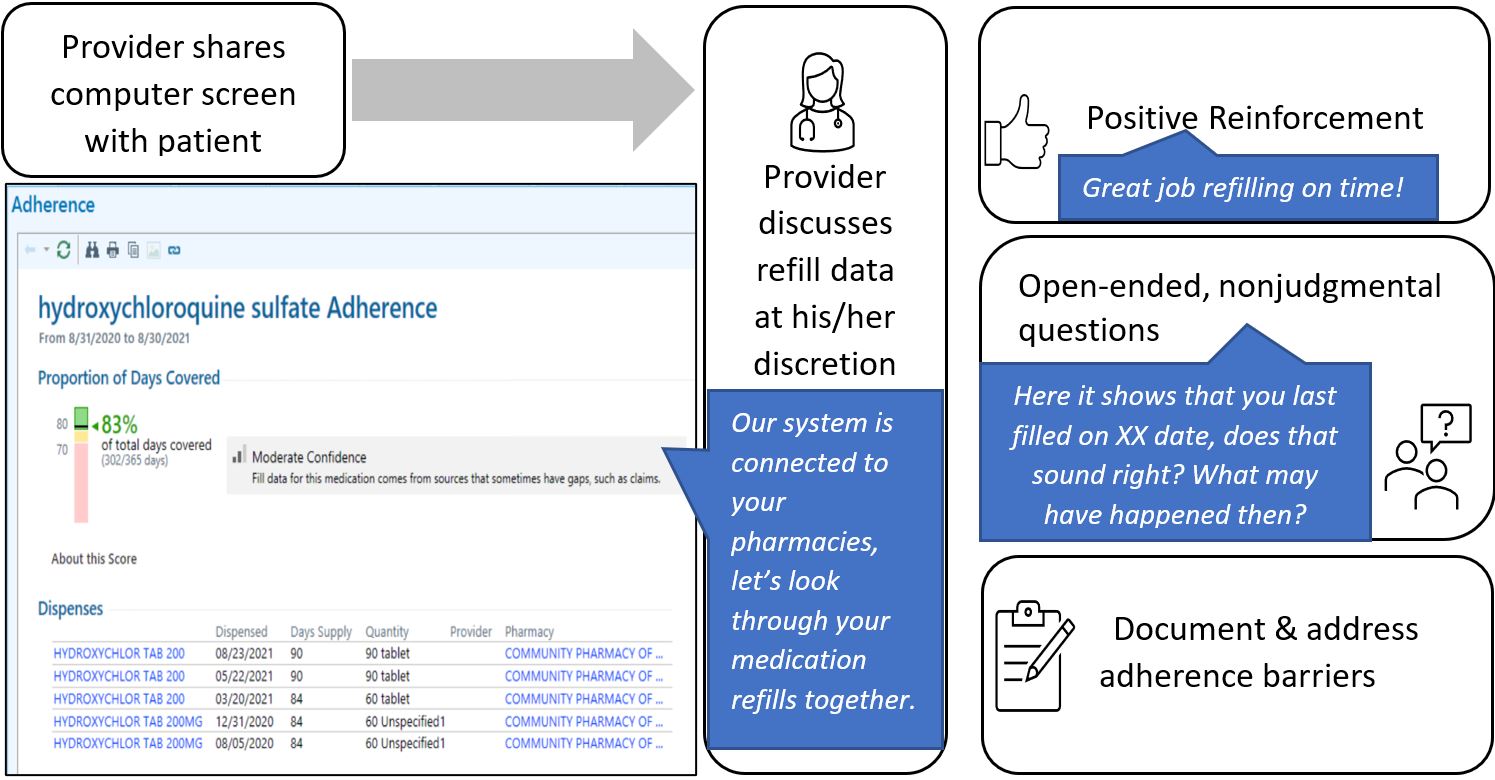 Figure 1. Adherence intervention workflow with screenshot of pharmacy refill data and example language.
Figure 1. Adherence intervention workflow with screenshot of pharmacy refill data and example language.
Disclosures: K. Sun, None; N. Molokwu, None; A. Corneli, None; K. Pollak, None; A. Bennion, None; J. Rogers, None; R. Sadun, None; L. Criscione-Schreiber, GlaxoSmithKlein(GSK); J. Doss, Pfizer; A. Eudy, GlaxoSmithKlein(GSK), Pfizer, Exagen; H. Bosworth, Boehringer-Ingelheim, BeBetter Therapeutics, nordisk, Merck/MSD, Improved Patient Outcomes, otuska, sanofi, walmart; M. Clowse, Exagen.
Background/Purpose: Medication nonadherence in SLE is common and negatively impacts patient outcomes. Yet, little is known about how to improve medication adherence in patients with SLE. We developed a provider-led adherence intervention with the goals of identifying nonadherence, improving patient-provider communication, and facilitating logistics and increasing motivation for taking SLE medications. The intervention encourages providers to review real-time refill data with patients; use communication strategies such as validating the patient's experiences, providing positive reinforcement, and asking open-ended and nonjudgmental questions to encourage discussion; and address identified adherence barriers (Figure 1). Prior pilot testing showed 10% improvement in medication adherence after one visit, and results from provider and patient surveys supported intervention feasibility and acceptability. In the current study, we examined provider fidelity, time spent, and quality of patient-provider communication during the adherence intervention to identify areas for improvement and to inform implementation.
Methods: All providers in an academic lupus clinic were asked to implement the intervention. With patients' consent, we audio recorded patient encounters during which the adherence intervention was performed. Patients were eligible if they were prescribed SLE-specific medications and had a medication possession ratio < 80% based on pharmacy refill information in the past 3 months. During analysis, we coded whether the clinician shared refill data with the patient, asked open-ended questions regarding adherence, made nonjudgmental statements to normalize missing doses or recognize difficulty taking medications, and used positive reinforcement, such as praising patients for good behaviors observed. Following their clinic visit, patients were invited to participate in in-depth individual interviews about their experiences with the adherence intervention. The interviews were audio-recorded and analyzed using applied thematic analysis.
Results: We recorded and analyzed 24 encounters among six lupus clinic physicians. Patients' median age was 37, 100% were female, and 75% were Black. Physicians reviewed refill information with patients in 20 encounters, used positive reinforcement in 21, validated the patient in 17, and asked open-ended questions in 11. On average, clinicians spent 3.9 minutes discussing medication adherence.
We interviewed 15 patients. All felt that the amount of time spent discussing lupus medications was "just right" except for one who felt that it was slightly long in the context of an otherwise short visit. Nearly all patients described having a positive experience with the adherence intervention.
Conclusion: We provide additional evidence to support the feasibility of incorporating the adherence intervention into routine clinical care and acceptability by patients. We also found an opportunity to improve provider training in asking open-ended questions and using patient validation when communicating with patients about medication adherence. Future work should test the intervention in a larger controlled setting.
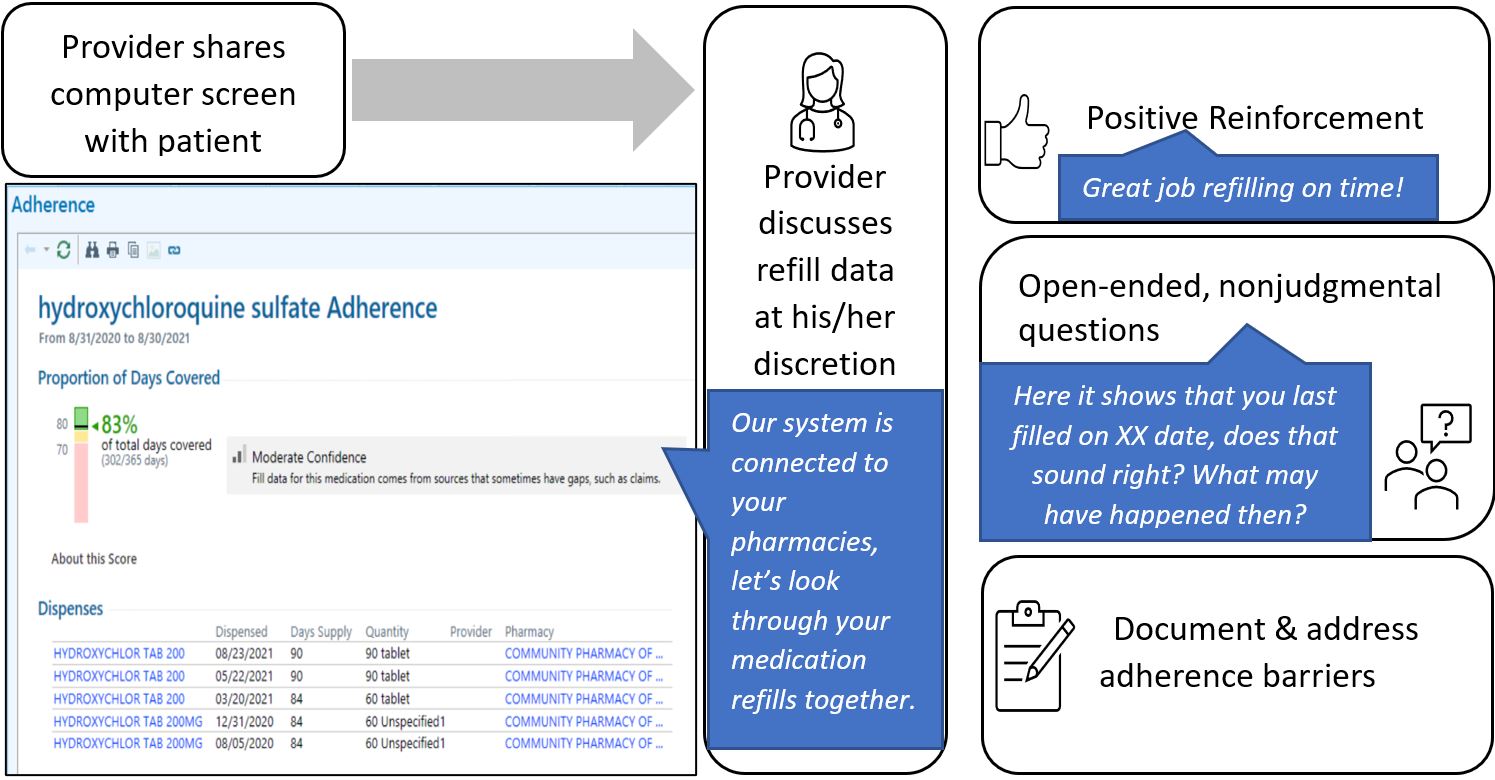 Figure 1. Adherence intervention workflow with screenshot of pharmacy refill data and example language.
Figure 1. Adherence intervention workflow with screenshot of pharmacy refill data and example language.Disclosures: K. Sun, None; N. Molokwu, None; A. Corneli, None; K. Pollak, None; A. Bennion, None; J. Rogers, None; R. Sadun, None; L. Criscione-Schreiber, GlaxoSmithKlein(GSK); J. Doss, Pfizer; A. Eudy, GlaxoSmithKlein(GSK), Pfizer, Exagen; H. Bosworth, Boehringer-Ingelheim, BeBetter Therapeutics, nordisk, Merck/MSD, Improved Patient Outcomes, otuska, sanofi, walmart; M. Clowse, Exagen.

