Back
Poster Session A
Systemic lupus erythematosus (SLE)
Session: (0317–0342) SLE – Diagnosis, Manifestations, and Outcomes Poster I: Diagnosis
0323: Identifying Distinct Phenotypes of Patients with Juvenile Systemic Lupus Erythematosus: Results from a Cluster Analysis by the Egyptian College of Rheumatology (ECR) Study Group
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- NH
Nevin Hammam, MD, PhD
Rheumatology Department, Faculty of Medicine, Assiut University, Assiut, Egypt
PASADENA, CA, United States
Abstract Poster Presenter(s)
Nevin Hammam1, Mohamed Bakrey Mahmoud2, Aly Bakhiet3, Rasha El Owaidy4, Hend Abdel Nabi5, Ahmed M Elsaman6, Iman Khalifa7, Abeer M NourEl-Din8, Rawhya R ElShereef9, Eman Hassan10, Faten Ismail9, Iman I El-Gazzar11, Abdelhafeez Moshrif12, Noha M Khalil13, Marwa A Amer14, Hanan M Fathy15, Nancy Abdel Salam15, Samar Tharwat16, Mervat I Abd Elazeem17, Hanan M Fathi18 and Tamer A Gheita11, 1Rheumatology Department, Faculty of Medicine, Assiut University, Assiut, Egypt, PASADENA, CA, 2Higher Institute for Computer Science and Information Systems, 6th of October City, Cairo, Egypt, 3Higher Institute for Computer Science and Information Systems, 6th of October City, Assiut, Egypt, 4Pediatric Allergy, Immunology and Rheumatology Unit, Children's Hospital, Ain Shams University, Cairo, Egypt, 5Pediatrics Department, Rheumatology and Nephrology Unit, Tanta University, Gharbia, Egypt, 6Rheumatology Department, Faculty of Medicine, Sohag University, Sohag, Egypt, 7Pediatrics Department, Rheumatology and Nephrology Unit, Helwan University, Cairo, Egypt, 8Pediatrics Department, National Research Centre (NRC), Cairo, Egypt, 9Rheumatology Department, Faculty of Medicine, Minia University, Minia, Egypt, 10Internal Medicine Department, Rheumatology Unit, Faculty of Medicine, Alexandria University, Alexandria, Egypt, 11Rheumatology Department, Faculty of Medicine, Cairo University, Cairo, Egypt, 12Rheumatology Department, Faculty of Medicine, Al-Azhar University, Assiut, Egypt, 13Internal Medicine Department, Rheumatology Unit, Faculty of Medicine, Cairo University, Cairo, Egypt, 14Rheumatology Department, Faculty of Medicine, Alexandria University, Alexandria, Egypt, 15Pediatrics Department, Rheumatology and Nephrology Unit, Alexandria University, Alexandria, Egypt, 16Internal Medicine, Rheumatology Unit, Mansoura University, Dakahlia, Egypt, Dakahlia, Egypt, 17Rheumatology Department, Faculty of Medicine, Beni-Suef University, Beni-Suef, Egypt, 18Rheumatology Department, Faculty of Medicine, Fayoum University, Fayoum, Egypt
Background/Purpose: Juvenile systemic lupus erythematosus (J-SLE) is a complex autoimmune disease characterized by a great heterogeneity in organs involvement. A better understanding of the organ involvement patterns in patients with J-SLE may facilitate making accurate individualized management decisions. Therefore, we examined the clinical patterns of organ manifestations in patients with J-SLE by using cluster analysis and compared the frequency of various clinical features including lupus nephritis (LN), laboratory variables, and immunosuppressive therapies among these clusters of patients.
Methods: Patients (≤18 years) have a confirmed diagnosis of J-SLE by SLICC classification criteria were identified from the clinical database of the Egyptian College of Rheumatology (ECR) SLE study group (Eesa NN, et al. Lupus 2021). The demographic data, clinical characteristics, disease activity score, disease damage index, autoantibodies, and current therapies were selected. Patients were divided into groups by using the K-mean cluster analysis. After clustering, distinct J-SLE subtypes were identified and then validated by detecting significant differences across clusters. The Chi-square test was used for categorical variables and one-way ANOVA for continuous measures.
Results: Overall, 404 patients (355 (87.9%) female, mean age at diagnosis 11.2 years; mean disease duration 2.3 years) were included. Four distinct subsets of patients were identified with the characteristics of patients in each of these clusters summarized in Table 1, including the inter-cluster differences. The demographic characteristics and disease duration were comparable between groups (p > 0.05). Patients in cluster 1 (n=103, 25.5%) were characterized predominantly by mucocutaneous and neurologic manifestations. Patients in cluster 2 (n=101, 25.0%) were more likely to have arthritis and pulmonary manifestations. Cluster 3 was the smallest group (n=71, 17.6%), and patients in this group had the lowest prevalence of arthritis and LN, indicative of mild disease intensity. Patients in cluster 4 (n=129, 31.9%) have the highest prevalence of arthritis, vasculitis, renal involvement, and proliferative LN, Figure 1. The severity of the disease was different across clusters; patients in clusters 1 and 4 had the highest systemic lupus erythematosus disease activity index score, and lowest complement level, and were significantly less likely to use low dose aspirin (LDA). We found that autoantibodies positivity and SLE damage score were comparable across clusters.
Conclusion: We describe a large cohort of J-SLE and identify four distinct subgroups of patients using cluster analysis. The use of LDA appears to be associated with a mild severity form of the disease. Clustering analysis might help to implement targeted therapy for various disease subsets in heterogenous diseases like lupus. Further research to better understand the mechanistic pathways underlying different clinical phenotypes is needed.
Acknowledgment: The authors are grateful for Amany S El-Bahnasawy, Marwa ElKhalifa, Emad El-Shebini, Samah I Nasef, Nermeen Noshy, Nermeen Samy, Nouran M Abaza, Eman F Mohamed, Mohamed N Salem, Ahmed M Abdalla, Esam Abualfadl.
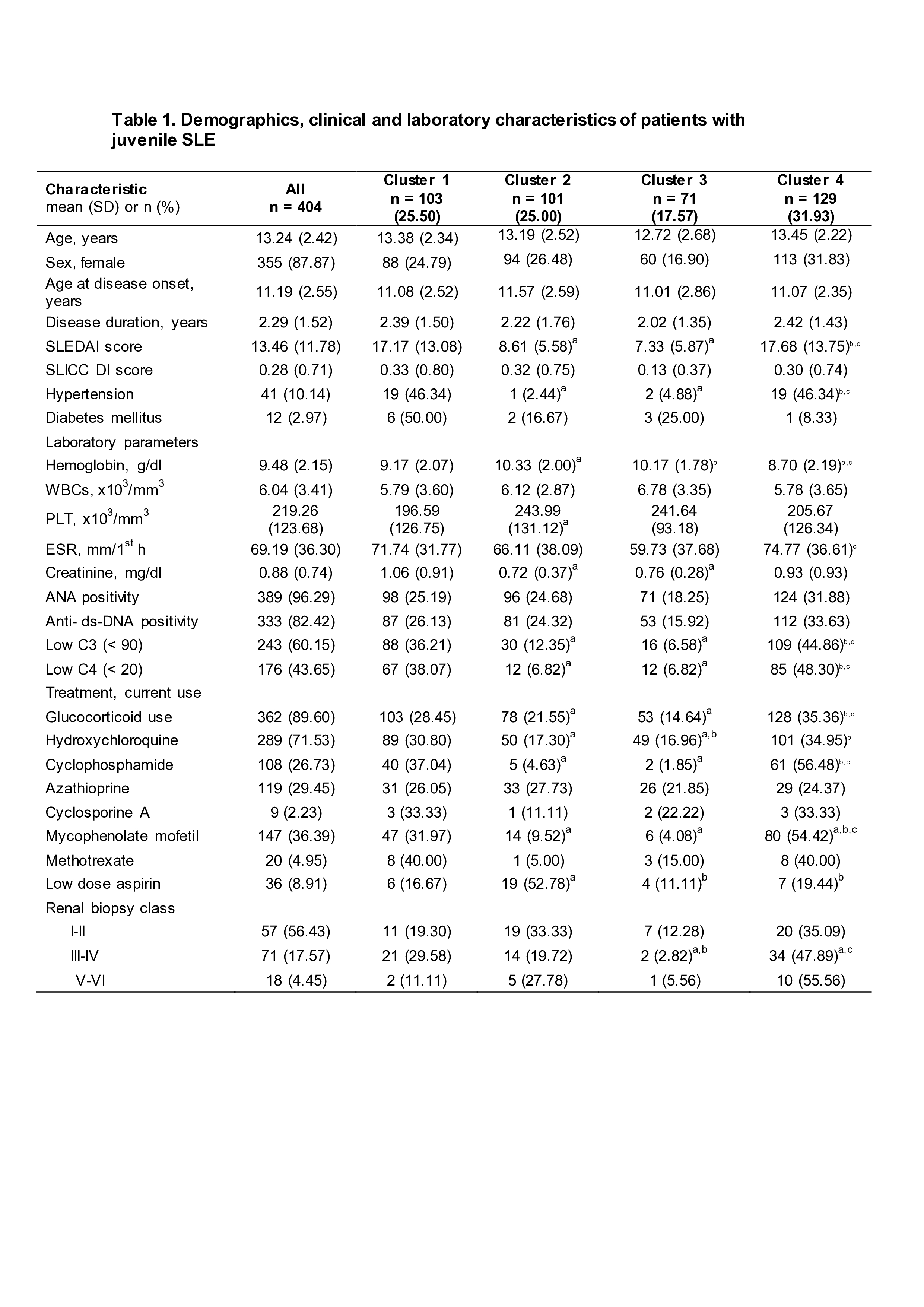 SD: standard deviation; SLE: systemic lupus erythematosus; SLEDAI: SLE Disease Activity Index; SLICC DI: Systemic Lupus Erythematosus International Collaborating Clinics Damage Index; WBCs: white blood cells, PLT: platelets, ESR: erythrocyte sedimentation rate; ANA: antinuclear antibody; anti-dsDNA: anti-double-stranded deoxyribonucleic acid antibody; and C: complement.
SD: standard deviation; SLE: systemic lupus erythematosus; SLEDAI: SLE Disease Activity Index; SLICC DI: Systemic Lupus Erythematosus International Collaborating Clinics Damage Index; WBCs: white blood cells, PLT: platelets, ESR: erythrocyte sedimentation rate; ANA: antinuclear antibody; anti-dsDNA: anti-double-stranded deoxyribonucleic acid antibody; and C: complement.
a Significantly different from cluster 1, b Significantly different from cluster 2, c Significantly different from cluster 3.
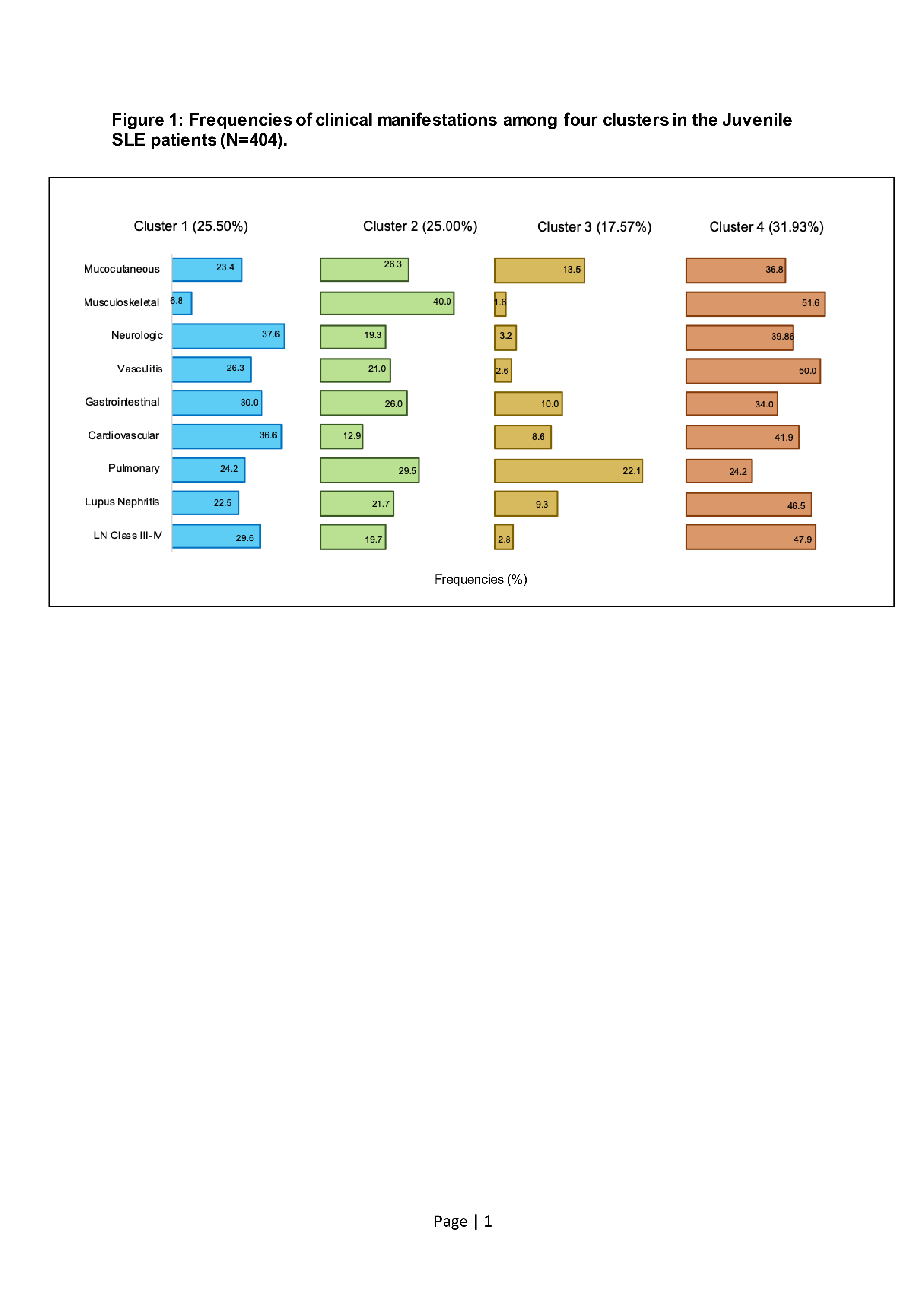 Mucocutaneous manifestations include malar rash, discoid rash, photosensitivity, and oral ulcer; Musculoskeletal manifestations include arthritis and myositis; Neurologic manifestations include depression, concentration problem, chorea, seizure, lupus headache, and peripheral neuropathy; Gastrointestinal manifestations include abdominal pain, hepatomegaly, elevated transaminase, and autoimmune hepatitis; Cardiovascular manifestations include pericarditis, myocarditis, endocarditis, and valvular insufficiency; Pulmonary manifestations include pleurisy/pleural effusion and pulmonary infiltrates; and Lupus Nephritis according to the 2018 revised classification of the International Society of Nephrology and the Renal Pathology Society.
Mucocutaneous manifestations include malar rash, discoid rash, photosensitivity, and oral ulcer; Musculoskeletal manifestations include arthritis and myositis; Neurologic manifestations include depression, concentration problem, chorea, seizure, lupus headache, and peripheral neuropathy; Gastrointestinal manifestations include abdominal pain, hepatomegaly, elevated transaminase, and autoimmune hepatitis; Cardiovascular manifestations include pericarditis, myocarditis, endocarditis, and valvular insufficiency; Pulmonary manifestations include pleurisy/pleural effusion and pulmonary infiltrates; and Lupus Nephritis according to the 2018 revised classification of the International Society of Nephrology and the Renal Pathology Society.
Disclosures: N. Hammam, None; M. Bakrey Mahmoud, None; A. Bakhiet, None; R. El Owaidy, None; H. Abdel Nabi, None; A. M Elsaman, None; I. Khalifa, None; A. M NourEl-Din, None; R. R ElShereef, None; E. Hassan, None; F. Ismail, None; I. I El-Gazzar, None; A. Moshrif, None; N. M Khalil, None; M. A Amer, None; H. M Fathy, None; N. Abdel Salam, None; S. Tharwat, None; M. I Abd Elazeem, None; H. M Fathi, None; T. Gheita, None.
Background/Purpose: Juvenile systemic lupus erythematosus (J-SLE) is a complex autoimmune disease characterized by a great heterogeneity in organs involvement. A better understanding of the organ involvement patterns in patients with J-SLE may facilitate making accurate individualized management decisions. Therefore, we examined the clinical patterns of organ manifestations in patients with J-SLE by using cluster analysis and compared the frequency of various clinical features including lupus nephritis (LN), laboratory variables, and immunosuppressive therapies among these clusters of patients.
Methods: Patients (≤18 years) have a confirmed diagnosis of J-SLE by SLICC classification criteria were identified from the clinical database of the Egyptian College of Rheumatology (ECR) SLE study group (Eesa NN, et al. Lupus 2021). The demographic data, clinical characteristics, disease activity score, disease damage index, autoantibodies, and current therapies were selected. Patients were divided into groups by using the K-mean cluster analysis. After clustering, distinct J-SLE subtypes were identified and then validated by detecting significant differences across clusters. The Chi-square test was used for categorical variables and one-way ANOVA for continuous measures.
Results: Overall, 404 patients (355 (87.9%) female, mean age at diagnosis 11.2 years; mean disease duration 2.3 years) were included. Four distinct subsets of patients were identified with the characteristics of patients in each of these clusters summarized in Table 1, including the inter-cluster differences. The demographic characteristics and disease duration were comparable between groups (p > 0.05). Patients in cluster 1 (n=103, 25.5%) were characterized predominantly by mucocutaneous and neurologic manifestations. Patients in cluster 2 (n=101, 25.0%) were more likely to have arthritis and pulmonary manifestations. Cluster 3 was the smallest group (n=71, 17.6%), and patients in this group had the lowest prevalence of arthritis and LN, indicative of mild disease intensity. Patients in cluster 4 (n=129, 31.9%) have the highest prevalence of arthritis, vasculitis, renal involvement, and proliferative LN, Figure 1. The severity of the disease was different across clusters; patients in clusters 1 and 4 had the highest systemic lupus erythematosus disease activity index score, and lowest complement level, and were significantly less likely to use low dose aspirin (LDA). We found that autoantibodies positivity and SLE damage score were comparable across clusters.
Conclusion: We describe a large cohort of J-SLE and identify four distinct subgroups of patients using cluster analysis. The use of LDA appears to be associated with a mild severity form of the disease. Clustering analysis might help to implement targeted therapy for various disease subsets in heterogenous diseases like lupus. Further research to better understand the mechanistic pathways underlying different clinical phenotypes is needed.
Acknowledgment: The authors are grateful for Amany S El-Bahnasawy, Marwa ElKhalifa, Emad El-Shebini, Samah I Nasef, Nermeen Noshy, Nermeen Samy, Nouran M Abaza, Eman F Mohamed, Mohamed N Salem, Ahmed M Abdalla, Esam Abualfadl.
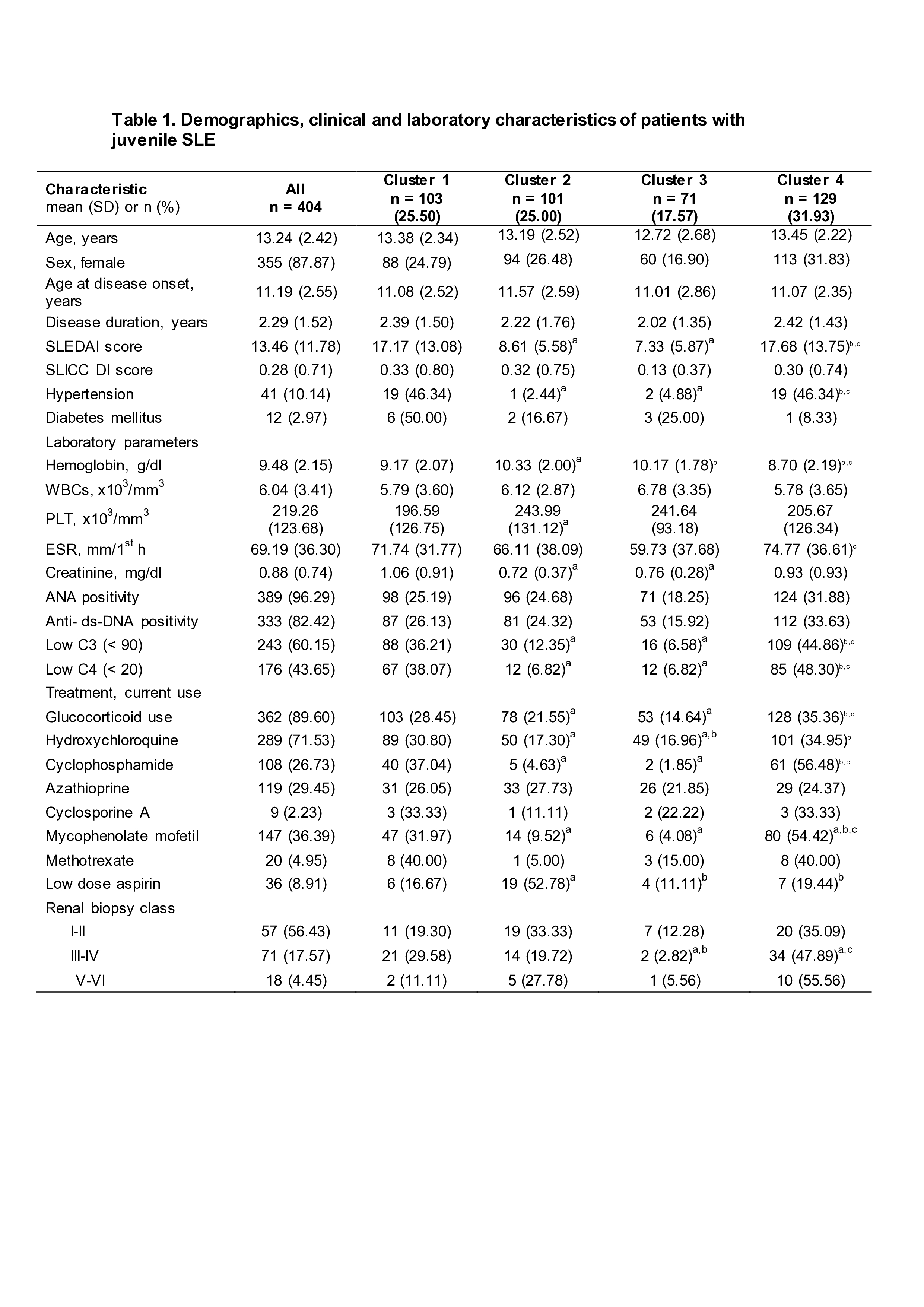 SD: standard deviation; SLE: systemic lupus erythematosus; SLEDAI: SLE Disease Activity Index; SLICC DI: Systemic Lupus Erythematosus International Collaborating Clinics Damage Index; WBCs: white blood cells, PLT: platelets, ESR: erythrocyte sedimentation rate; ANA: antinuclear antibody; anti-dsDNA: anti-double-stranded deoxyribonucleic acid antibody; and C: complement.
SD: standard deviation; SLE: systemic lupus erythematosus; SLEDAI: SLE Disease Activity Index; SLICC DI: Systemic Lupus Erythematosus International Collaborating Clinics Damage Index; WBCs: white blood cells, PLT: platelets, ESR: erythrocyte sedimentation rate; ANA: antinuclear antibody; anti-dsDNA: anti-double-stranded deoxyribonucleic acid antibody; and C: complement. a Significantly different from cluster 1, b Significantly different from cluster 2, c Significantly different from cluster 3.
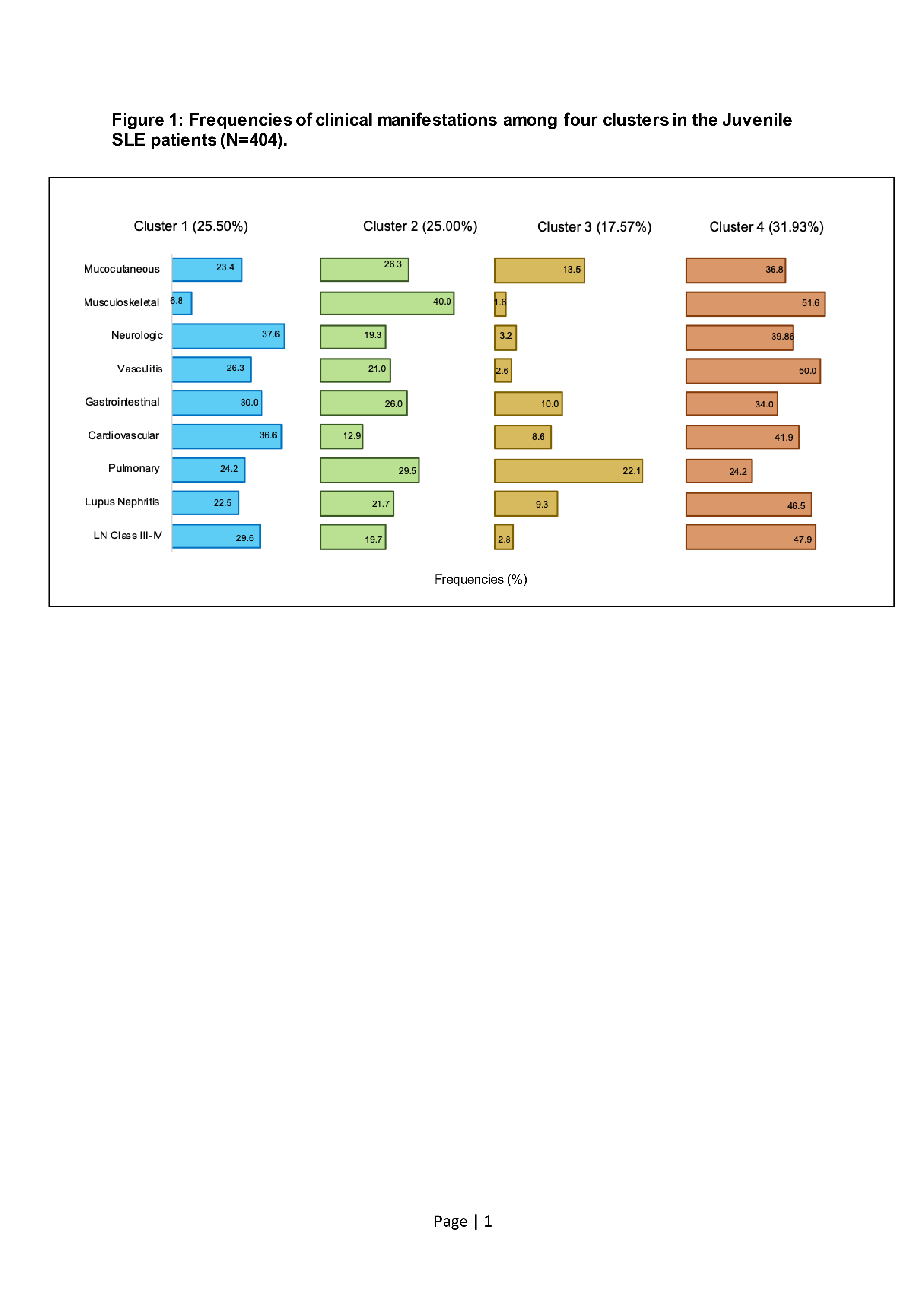 Mucocutaneous manifestations include malar rash, discoid rash, photosensitivity, and oral ulcer; Musculoskeletal manifestations include arthritis and myositis; Neurologic manifestations include depression, concentration problem, chorea, seizure, lupus headache, and peripheral neuropathy; Gastrointestinal manifestations include abdominal pain, hepatomegaly, elevated transaminase, and autoimmune hepatitis; Cardiovascular manifestations include pericarditis, myocarditis, endocarditis, and valvular insufficiency; Pulmonary manifestations include pleurisy/pleural effusion and pulmonary infiltrates; and Lupus Nephritis according to the 2018 revised classification of the International Society of Nephrology and the Renal Pathology Society.
Mucocutaneous manifestations include malar rash, discoid rash, photosensitivity, and oral ulcer; Musculoskeletal manifestations include arthritis and myositis; Neurologic manifestations include depression, concentration problem, chorea, seizure, lupus headache, and peripheral neuropathy; Gastrointestinal manifestations include abdominal pain, hepatomegaly, elevated transaminase, and autoimmune hepatitis; Cardiovascular manifestations include pericarditis, myocarditis, endocarditis, and valvular insufficiency; Pulmonary manifestations include pleurisy/pleural effusion and pulmonary infiltrates; and Lupus Nephritis according to the 2018 revised classification of the International Society of Nephrology and the Renal Pathology Society. Disclosures: N. Hammam, None; M. Bakrey Mahmoud, None; A. Bakhiet, None; R. El Owaidy, None; H. Abdel Nabi, None; A. M Elsaman, None; I. Khalifa, None; A. M NourEl-Din, None; R. R ElShereef, None; E. Hassan, None; F. Ismail, None; I. I El-Gazzar, None; A. Moshrif, None; N. M Khalil, None; M. A Amer, None; H. M Fathy, None; N. Abdel Salam, None; S. Tharwat, None; M. I Abd Elazeem, None; H. M Fathi, None; T. Gheita, None.

