Back
Poster Session A
Systemic lupus erythematosus (SLE)
Session: (0317–0342) SLE – Diagnosis, Manifestations, and Outcomes Poster I: Diagnosis
0325: Ordering Practices and Diagnostic Utility of Cardiac MRI in SLE Patients at a Single Academic Institution
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- EC
Erin Chew, MD
Vanderbilt University Medical Center
Nashville, TN, United States
Abstract Poster Presenter(s)
Erin Chew1, Bibin Varghese1, Christopher Chew2, Tracy Frech1, Quinn Wells1 and April Barnado1, 1Vanderbilt University Medical Center, Nashville, TN, 2University of North Carolina at Chapel Hill, Chapel Hill, NC
Background/Purpose: Cardiac magnetic resonance imaging (cMRI) is the gold standard modality for evaluation of cardiac anatomy, function, and characterization of myocardial tissues. cMRI has been proposed to be helpful in SLE patients to distinguish between myocardial inflammation, suspected infiltration, perfusion abnormalities, and fibrosis. No practice guidelines currently exist to provide specific recommendations for cMRI in SLE patients. Using a large, de-identified electronic health record (EHR), we examined ordering practices of cMRI in SLE patients and its impact on clinical care.
Methods: SLE patients were identified from a de-identified EHR with over 3.4 million subjects with over 30 years of follow-up using a previously validated algorithm. Within this SLE cohort (n = 3494), we used CPT codes 75552-75565 to identify SLE patients with cMRIs (Figure 1). Demographic and clinical information were obtained from chart review.
Results: There were 73 SLE patients (90% female, 53% white) who underwent cMRI between 2005 and 2020. Of the cohort, 67 (92%) had cardiopulmonary symptoms while 6 (8%) patients were asymptomatic. Of the patients with symptoms, all had prior electrocardiograms and 82% had transthoracic echocardiogram (TTE), 12% stress test, 16% left heart catherization, and 11% right heart catherization prior to a cMRI. Indications for ordering cMRI are displayed in Table 1. Of the 42 cMRIs ordered to evaluate myocardial pathology or unclear cardiopulmonary symptoms, 31 (74%) were ordered to follow up on pathology seen on TTE and 11 (26%) to evaluate for pathology not seen on TTE. There were 12 cMRIs that raised concern for a pathologic process not previously considered, of which 3 led to biopsies and final diagnosis of either amyloid or myocarditis. Of 18 patients who underwent cMRI to evaluate severity of valvular pathology, 13 (72%) avoided a planned valve repair. Of the 73 total cMRI ordered, 26 (35%) led to management changes including 2 patients requiring valve repair, 6 patients requiring medication changes, 5 patients requiring further diagnostic work up, 13 patients avoiding planned valve repair (Figure 2). Only 15% of cMRIs were performed with the newer quantitative parametric mapping techniques.
Conclusion: In the majority of SLE patients, cMRIs were ordered to distinguish between myocarditis/pericarditis, infiltrative disease, cardiomyopathy, and ischemia as the underlying cause for cardiopulmonary symptoms. Although cMRIs are not commonly ordered in this patient population, the results of cMRIs changed management in a significant number of SLE patients. cMRIs were ordered to assess the degree of valvular pathology and were particularly helpful for avoiding surgical valve intervention. Advances in cMRI technology have increased diagnostic utility with future studies needed to determine its role in guiding immunosuppressive therapies for myocardial pathology.
.jpg) Figure 1. Flow chart of SLE patients with cardiac MRIs. Potential SLE cases were selected from the de-identified electronic health record using ≥ 4 ICD-9 (710.0) or ICD-10-CM SLE (M32.1, M32.8, M32.9) codes and a positive ANA (titer ≥ 1:160) while excluding codes for dermatomyositis and systemic sclerosis. Of these potential SLE cases, we applied CPT codes for cardiac MRI (75552-75565) to identify SLE cases with cMRI.
Figure 1. Flow chart of SLE patients with cardiac MRIs. Potential SLE cases were selected from the de-identified electronic health record using ≥ 4 ICD-9 (710.0) or ICD-10-CM SLE (M32.1, M32.8, M32.9) codes and a positive ANA (titer ≥ 1:160) while excluding codes for dermatomyositis and systemic sclerosis. Of these potential SLE cases, we applied CPT codes for cardiac MRI (75552-75565) to identify SLE cases with cMRI.
.jpg)
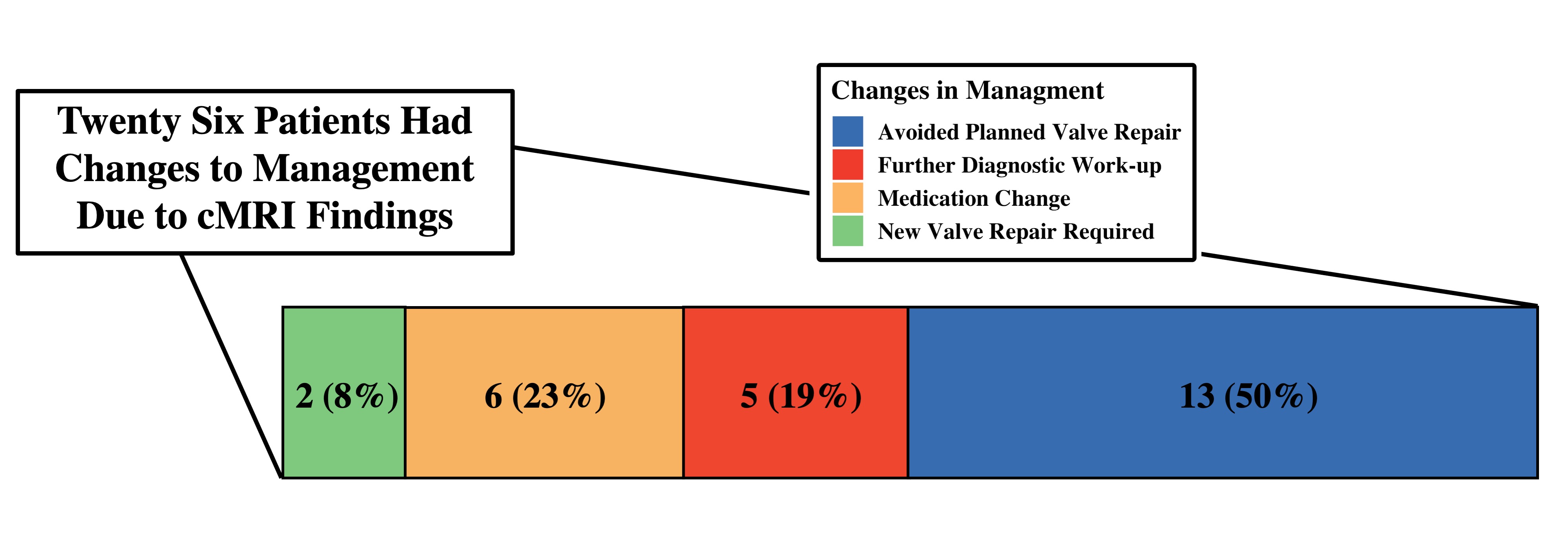 Figure 2. Management Changes in Response to cMRI Findings. Of the 73 SLE patients with cardiac MRI, 26 (35%) had changes in their management with reasons noted above.
Figure 2. Management Changes in Response to cMRI Findings. Of the 73 SLE patients with cardiac MRI, 26 (35%) had changes in their management with reasons noted above.
Disclosures: E. Chew, None; B. Varghese, None; C. Chew, None; T. Frech, None; Q. Wells, None; A. Barnado, None.
Background/Purpose: Cardiac magnetic resonance imaging (cMRI) is the gold standard modality for evaluation of cardiac anatomy, function, and characterization of myocardial tissues. cMRI has been proposed to be helpful in SLE patients to distinguish between myocardial inflammation, suspected infiltration, perfusion abnormalities, and fibrosis. No practice guidelines currently exist to provide specific recommendations for cMRI in SLE patients. Using a large, de-identified electronic health record (EHR), we examined ordering practices of cMRI in SLE patients and its impact on clinical care.
Methods: SLE patients were identified from a de-identified EHR with over 3.4 million subjects with over 30 years of follow-up using a previously validated algorithm. Within this SLE cohort (n = 3494), we used CPT codes 75552-75565 to identify SLE patients with cMRIs (Figure 1). Demographic and clinical information were obtained from chart review.
Results: There were 73 SLE patients (90% female, 53% white) who underwent cMRI between 2005 and 2020. Of the cohort, 67 (92%) had cardiopulmonary symptoms while 6 (8%) patients were asymptomatic. Of the patients with symptoms, all had prior electrocardiograms and 82% had transthoracic echocardiogram (TTE), 12% stress test, 16% left heart catherization, and 11% right heart catherization prior to a cMRI. Indications for ordering cMRI are displayed in Table 1. Of the 42 cMRIs ordered to evaluate myocardial pathology or unclear cardiopulmonary symptoms, 31 (74%) were ordered to follow up on pathology seen on TTE and 11 (26%) to evaluate for pathology not seen on TTE. There were 12 cMRIs that raised concern for a pathologic process not previously considered, of which 3 led to biopsies and final diagnosis of either amyloid or myocarditis. Of 18 patients who underwent cMRI to evaluate severity of valvular pathology, 13 (72%) avoided a planned valve repair. Of the 73 total cMRI ordered, 26 (35%) led to management changes including 2 patients requiring valve repair, 6 patients requiring medication changes, 5 patients requiring further diagnostic work up, 13 patients avoiding planned valve repair (Figure 2). Only 15% of cMRIs were performed with the newer quantitative parametric mapping techniques.
Conclusion: In the majority of SLE patients, cMRIs were ordered to distinguish between myocarditis/pericarditis, infiltrative disease, cardiomyopathy, and ischemia as the underlying cause for cardiopulmonary symptoms. Although cMRIs are not commonly ordered in this patient population, the results of cMRIs changed management in a significant number of SLE patients. cMRIs were ordered to assess the degree of valvular pathology and were particularly helpful for avoiding surgical valve intervention. Advances in cMRI technology have increased diagnostic utility with future studies needed to determine its role in guiding immunosuppressive therapies for myocardial pathology.
.jpg) Figure 1. Flow chart of SLE patients with cardiac MRIs. Potential SLE cases were selected from the de-identified electronic health record using ≥ 4 ICD-9 (710.0) or ICD-10-CM SLE (M32.1, M32.8, M32.9) codes and a positive ANA (titer ≥ 1:160) while excluding codes for dermatomyositis and systemic sclerosis. Of these potential SLE cases, we applied CPT codes for cardiac MRI (75552-75565) to identify SLE cases with cMRI.
Figure 1. Flow chart of SLE patients with cardiac MRIs. Potential SLE cases were selected from the de-identified electronic health record using ≥ 4 ICD-9 (710.0) or ICD-10-CM SLE (M32.1, M32.8, M32.9) codes and a positive ANA (titer ≥ 1:160) while excluding codes for dermatomyositis and systemic sclerosis. Of these potential SLE cases, we applied CPT codes for cardiac MRI (75552-75565) to identify SLE cases with cMRI. .jpg)
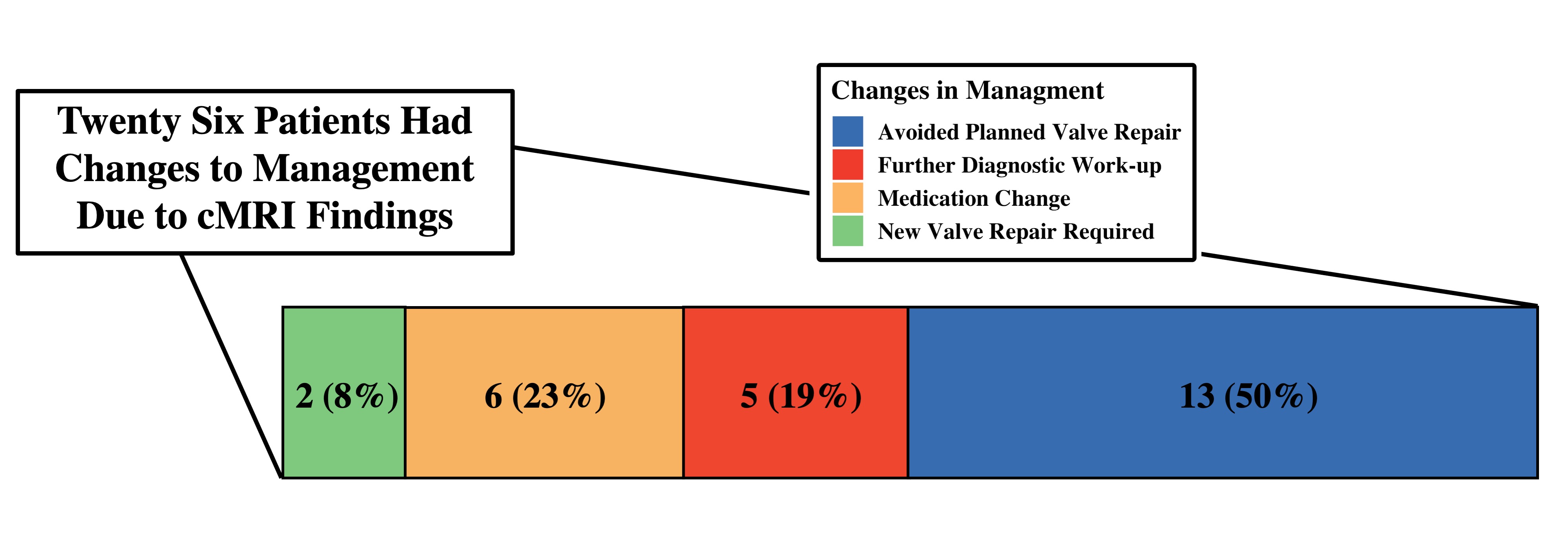 Figure 2. Management Changes in Response to cMRI Findings. Of the 73 SLE patients with cardiac MRI, 26 (35%) had changes in their management with reasons noted above.
Figure 2. Management Changes in Response to cMRI Findings. Of the 73 SLE patients with cardiac MRI, 26 (35%) had changes in their management with reasons noted above. Disclosures: E. Chew, None; B. Varghese, None; C. Chew, None; T. Frech, None; Q. Wells, None; A. Barnado, None.

