Back
Late-Breaking Abstract Session
Session: Late-Breaking Abstracts (L01–L06)
L01: Impact of Glucocorticoid Dosing and Anti-Osteoporotic Treatment on Bone Health in Patients with Inflammatory Rheumatic Musculoskeletal Diseases: A Longitudinal Cohort Study
Monday, November 14, 2022
9:00 AM – 9:10 AM Eastern Time
Location: Exhibit Hall A
.png)
Giovanni Adami, MD
University of Verona, Italy
Verona, Verona, Italy
Presenting Author(s)
Giovanni Adami, Angelo Fassio, Davide Bertelle, Camilla Benini, Davide Gatti and Maurizio Rossini, Rheumatology Unit, University of Verona, Verona, Italy
Background/Purpose: The recently published GLORIA (Glucocorticoid LOw-dose in RheumatoId Arthritis) trial has opened the debate around the benefits of glucocorticoids (GCs) in older patients with inflammatory diseases.
Methods: We conducted a longitudinal cohort study on women with iRMD. Glucocorticoid intake was recorded as 0 to 2.5 mg/day pred eq mean dose, 2.5 mg to 5 mg pred eq mean dose or ≥5 mg/day pred eq mean dose. Inflammatory Rheumatic Musculoskeletal Diseases (iRMD) included: rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), psoriatic arthritis (PsA), systemic sclerosis and other rheumatic diseases pooled together (vasculitides, polymyalgia rheumatica, spondylarthritis etc.). Bone mineral density and fracture were assessed prospectively and compared to a 2:1 propensity score matched (PSM) cohort of healthy women. Kaplan-Meier curves with log-rank test were made for iRMD (stratified for glucocorticoid use and dosage) and matched cohort respectively. Multivariable Cox regression survival models were also employed to analyze the effect of GCs on fracture.
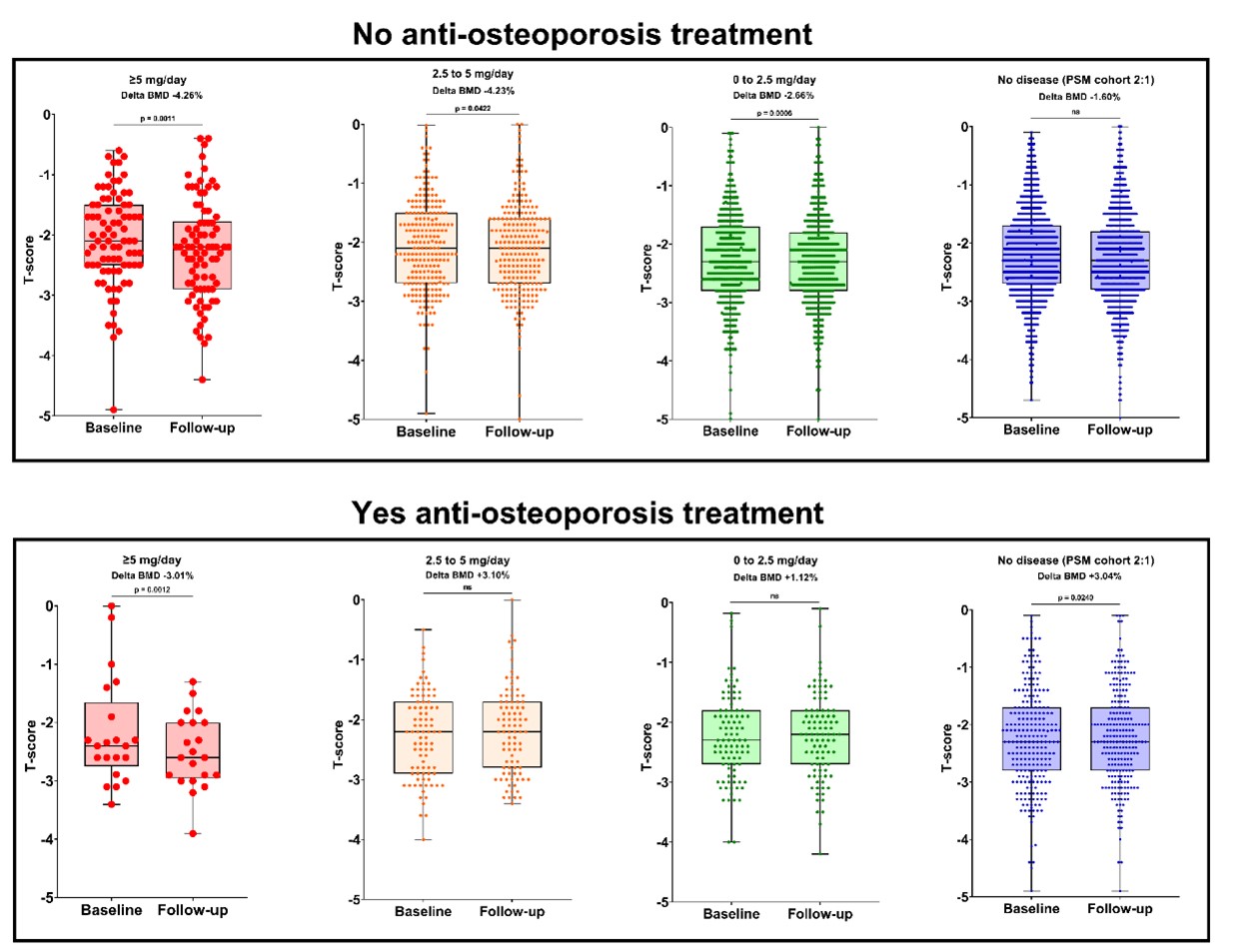
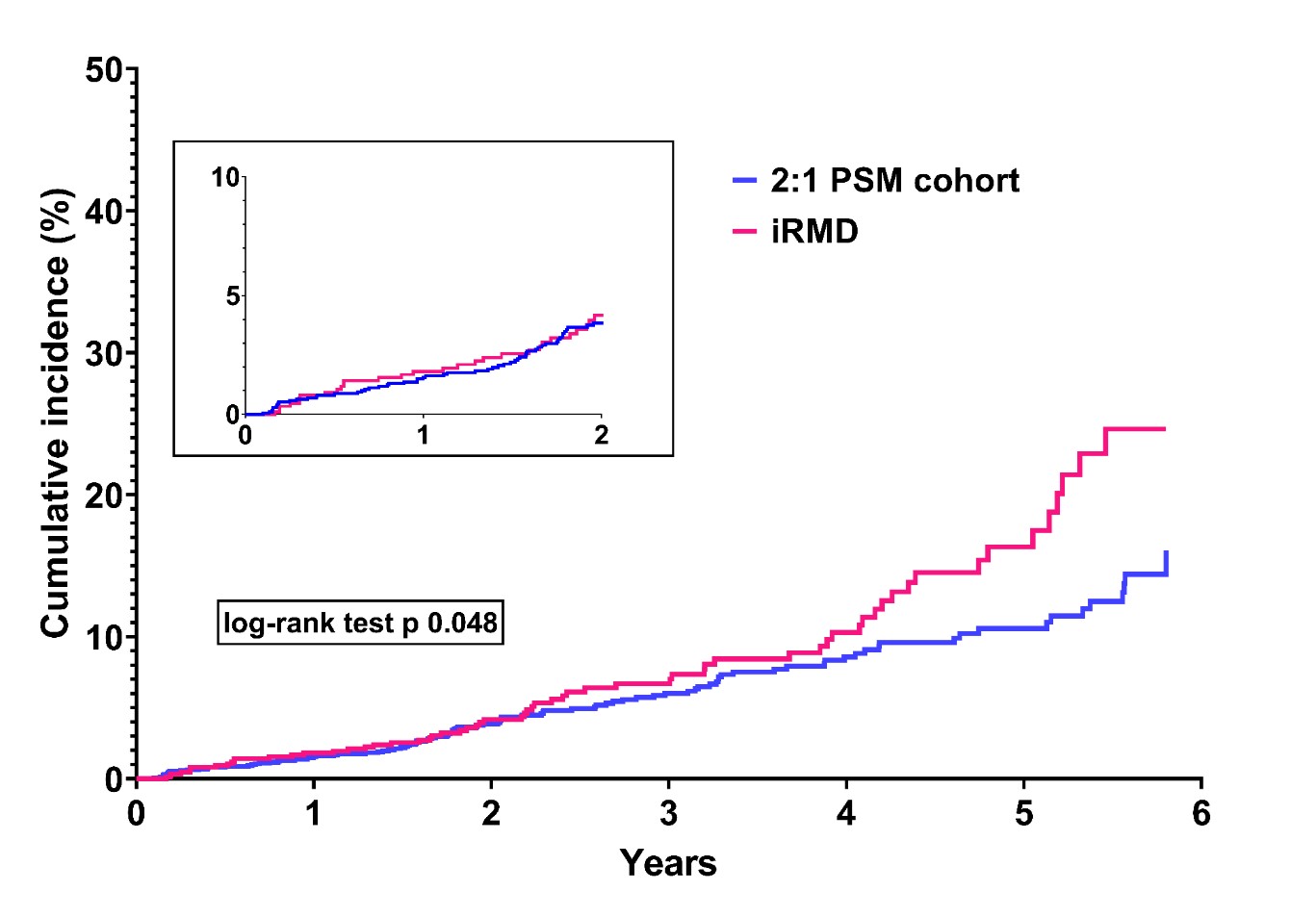
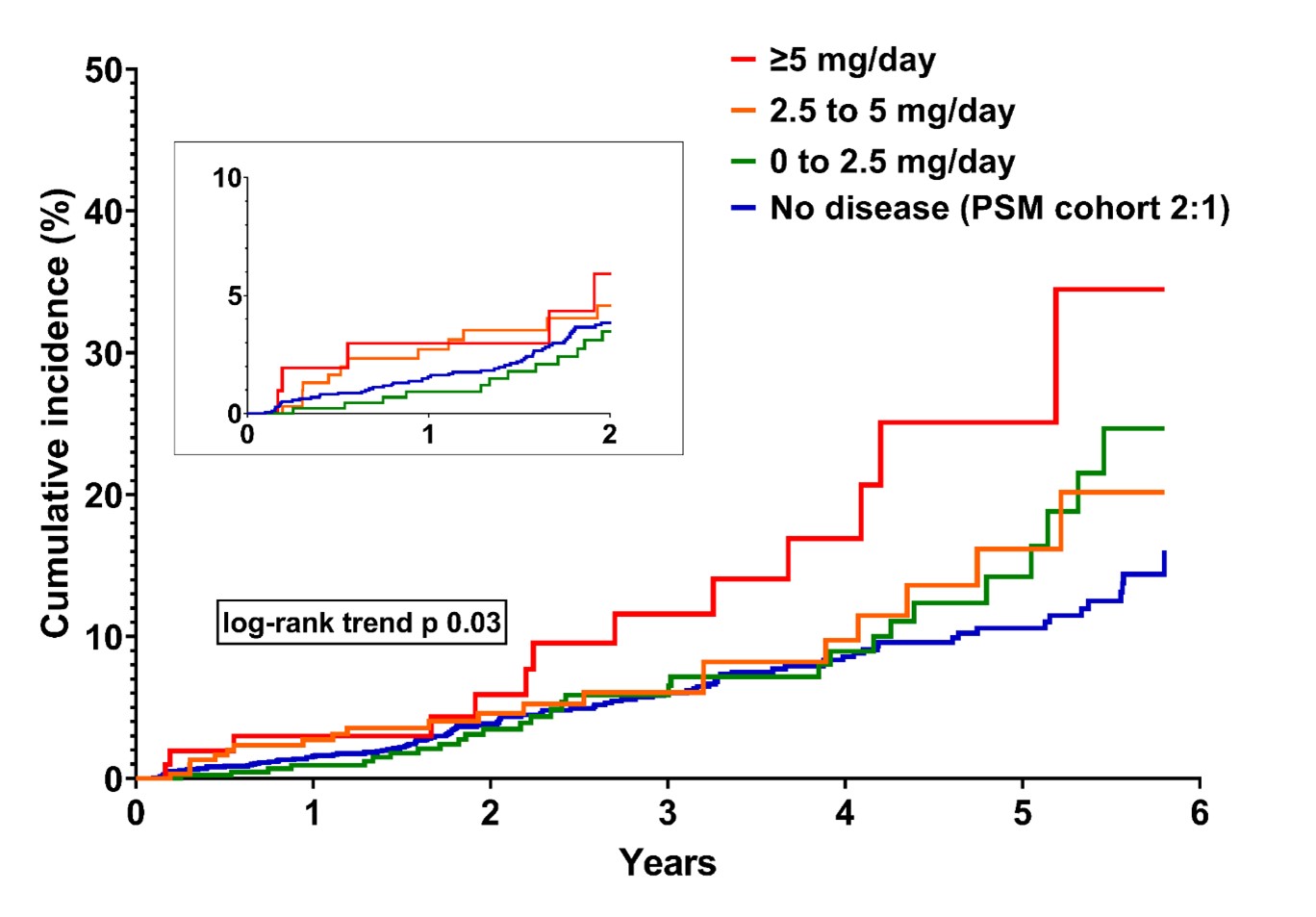
Results: 884 women with iRMD (largely RA) and 1,766 controls (age, T-score and the % 10-year fracture risk matched) were included in the study and followed up to 6 years. BMD levels decreased significantly in all GCs users not receiving anti-osteoporosis treatment (-4.26% p 0.0011, -4.23% p 0.0422, -2.66% p 0.0006 for ≥5 mg/day, 2.5 mg to 5 mg and 0 to 2.5 mg/day, respectively) figure 1. Anti-osteoporotic treatment increased BMD to a greater extent in patients receiving less than 5 mg/day of prednisone. A total of 21, 12 and 29 fractures were reported for patients receiving ≥5 mg/day, 2.5 mg to 5 mg and 0 to 2.5 mg/day respectively, corresponding to a crude fracture rate of 4.8 fractures per 100 person-year, 2.8 fractures per 100 person-year and 2.5 fractures per 100 person-year respectively. 103 fractures were registered in the PSM cohort (crude fracture rate of 2.2 fractures per 100 person-year). Fracture incidence was higher in patients with iRMD compared to controls. GC use ≥5 mg/day was associated with a 2-fold higher risk of fracture of any kind compared to all other doses and controls (aHR 2.37, 95% CI 1.33-4.23). Kaplan-Meier curves for the cumulative incidence of fracture are reported in figure 2 and figure 3.
Conclusion: GC doses as low as 2.5 mg/day were associated with BMD loss in iRMD but this effect was preventable with anti-osteoporotic drugs. The latter finding might support anti-osteoporotic treatment initiation in patients taking very low-dose GCs, in direct contrast with most guidelines of GIOP.
Disclosures: G. Adami, Eli Lilly, UCB, Amgen, Bristol-Myers Squibb(BMS), Galapagos, Fresenius Kabi; A. Fassio, None; D. Bertelle, None; C. Benini, None; D. Gatti, None; M. Rossini, None.
Background/Purpose: The recently published GLORIA (Glucocorticoid LOw-dose in RheumatoId Arthritis) trial has opened the debate around the benefits of glucocorticoids (GCs) in older patients with inflammatory diseases.
Methods: We conducted a longitudinal cohort study on women with iRMD. Glucocorticoid intake was recorded as 0 to 2.5 mg/day pred eq mean dose, 2.5 mg to 5 mg pred eq mean dose or ≥5 mg/day pred eq mean dose. Inflammatory Rheumatic Musculoskeletal Diseases (iRMD) included: rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), psoriatic arthritis (PsA), systemic sclerosis and other rheumatic diseases pooled together (vasculitides, polymyalgia rheumatica, spondylarthritis etc.). Bone mineral density and fracture were assessed prospectively and compared to a 2:1 propensity score matched (PSM) cohort of healthy women. Kaplan-Meier curves with log-rank test were made for iRMD (stratified for glucocorticoid use and dosage) and matched cohort respectively. Multivariable Cox regression survival models were also employed to analyze the effect of GCs on fracture.
Results: 884 women with iRMD (largely RA) and 1,766 controls (age, T-score and the % 10-year fracture risk matched) were included in the study and followed up to 6 years. BMD levels decreased significantly in all GCs users not receiving anti-osteoporosis treatment (-4.26% p 0.0011, -4.23% p 0.0422, -2.66% p 0.0006 for ≥5 mg/day, 2.5 mg to 5 mg and 0 to 2.5 mg/day, respectively) figure 1. Anti-osteoporotic treatment increased BMD to a greater extent in patients receiving less than 5 mg/day of prednisone. A total of 21, 12 and 29 fractures were reported for patients receiving ≥5 mg/day, 2.5 mg to 5 mg and 0 to 2.5 mg/day respectively, corresponding to a crude fracture rate of 4.8 fractures per 100 person-year, 2.8 fractures per 100 person-year and 2.5 fractures per 100 person-year respectively. 103 fractures were registered in the PSM cohort (crude fracture rate of 2.2 fractures per 100 person-year). Fracture incidence was higher in patients with iRMD compared to controls. GC use ≥5 mg/day was associated with a 2-fold higher risk of fracture of any kind compared to all other doses and controls (aHR 2.37, 95% CI 1.33-4.23). Kaplan-Meier curves for the cumulative incidence of fracture are reported in figure 2 and figure 3.
Conclusion: GC doses as low as 2.5 mg/day were associated with BMD loss in iRMD but this effect was preventable with anti-osteoporotic drugs. The latter finding might support anti-osteoporotic treatment initiation in patients taking very low-dose GCs, in direct contrast with most guidelines of GIOP.
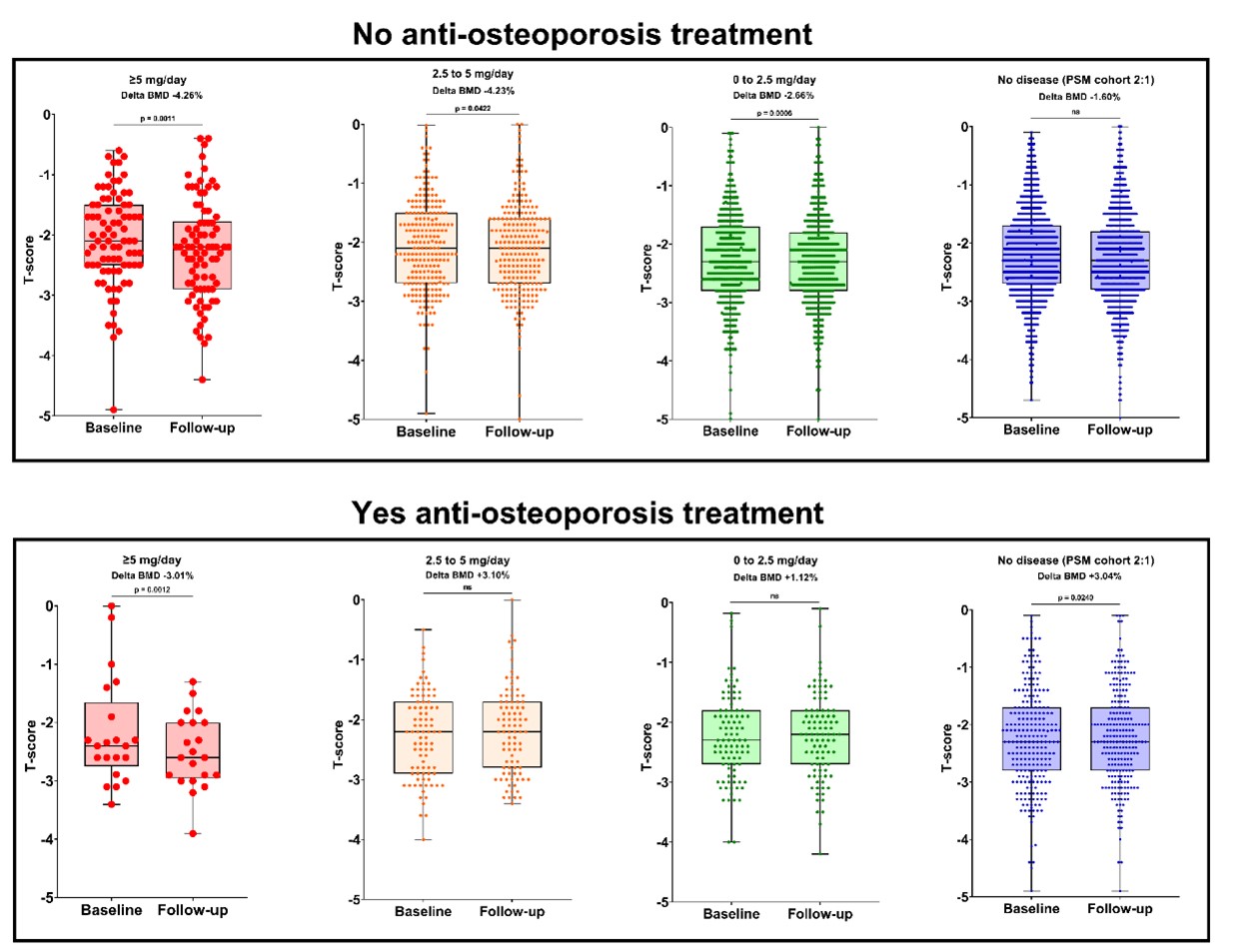
Figure 1. Bone mineral density changes in patients with iRMD and controls
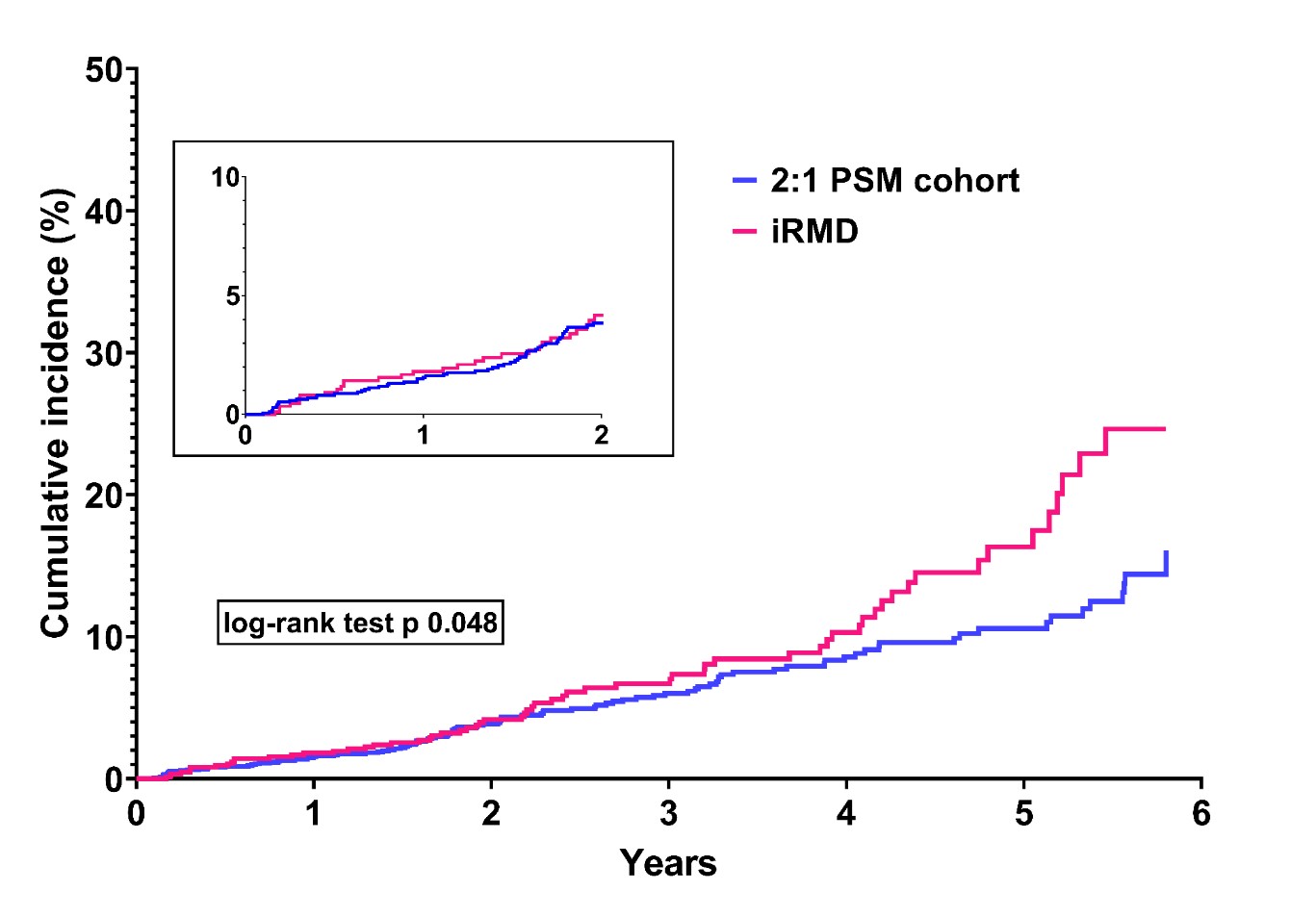
Figure 2. Kaplan-Meier curves for cumulative incidence of fragility fracture in patients with iRMD and controls
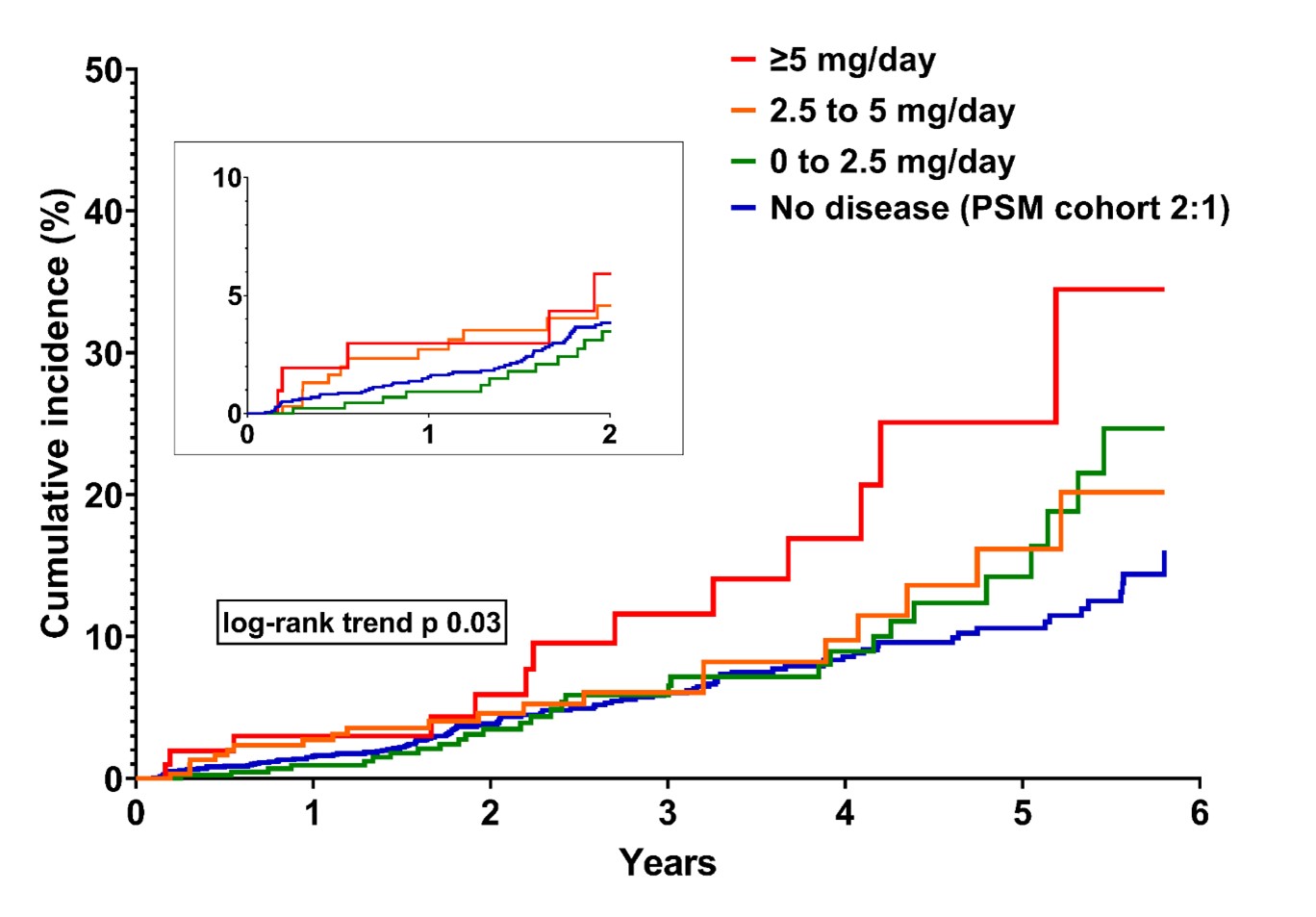
Figure 3. Kaplan-Meier curves for cumulative incidence of fragility fracture in patients with iRMD and controls stratified by glucocorticoid dose
Disclosures: G. Adami, Eli Lilly, UCB, Amgen, Bristol-Myers Squibb(BMS), Galapagos, Fresenius Kabi; A. Fassio, None; D. Bertelle, None; C. Benini, None; D. Gatti, None; M. Rossini, None.

