Back
Poster Session C
Metabolic bone disease
Session: (1304–1331) Osteoporosis and Metabolic Bone Disease – Basic and Clinical Science Poster
1322: Follow up of Incidentally Noted Vertebral Compression Fractures
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- JY
Jason Yang, MD, PhD
University of Massachusetts T.H. Chan Medical School
Worcester, MA, United States
Abstract Poster Presenter(s)
Jason Yang1, Alexia Hwang1, Megan Brochu2, Krista Sabina2, Meridith Malysz2, Bruce Weinstein3 and Jonathan Cheah1, 1UMass Chan Medical School, Worcester, MA, 2UMass Memorial Health, Worcester, MA, 3UMass Memorial Health, UMass Chan Medical School, Worcester, MA
Background/Purpose: Vertebral compression fractures (VCFs) in general represent a clinical diagnosis of osteoporosis, predisposing to an increased risk of additional fractures. However, a significant number of clinically important VCFs are asymptomatic and are only discovered on imaging studies performed for other reasons. As a result, subsequent diagnosis and management of osteoporosis in this patient group is often lacking. The aim of this study is to identify the management outcome of VCFs on CT and MRI scans within a single academic primary care practice.
Methods: CT and MRI scans of individuals aged 50 and over between October 2020 and October 2021 were reviewed from a single academic primary care primary care practice if they contained the term 'vertebral compression' in the text of the formal radiology report. Using the scan as the index event, the subsequent six months of the electronic medical record was reviewed for the number of interactions between the individual and the primary care office, as well as for an existing or new formal diagnosis of osteoporosis and what subsequent management regarding bone health and fracture risk reduction was initiated.
Results: 77 individuals (mean age 74 years, 49 female) and 122 CT/MRI scans indicated VCFs in the formal radiology report (Table 1). 18 (15%) of these scans were ordered by the primary care practice and 64 (52%) of the indications of the investigation was a musculoskeletal (MSK) complaint. 52 (43%) studies were specifically of the thoracic or lumbar spine.
44 (57%) individuals had a pre-existing diagnosis of osteoporosis. Of the 33 who did not, in the subsequent six months, there was a mean of 1.7 follow up visits. Six (18%) had a dual energy x-ray absorptiometry scan ordered and six individuals (18%) were started on therapy for fracture risk reduction. The majority of individuals without a pre-existing diagnosis of osteoporosis who were subsequently prescribed therapies for future fracture risk reduction were those who underwent an imaging study specifically of the thoracic or lumbar spine (43%) or where the indication of the study was musculoskeletal (36%).
Conclusion: The majority of individuals who had an advanced imaging test which identified a VCF had a pre-existing diagnosis of osteoporosis. However, in those that did not, further assessment and initiation of therapy for future fracture risk reduction was low. Future work will aim to identify specific interventions to better enable further investigation and management of those with incidentally noted VCFs, but without a pre-existing diagnosis of osteoporosis.
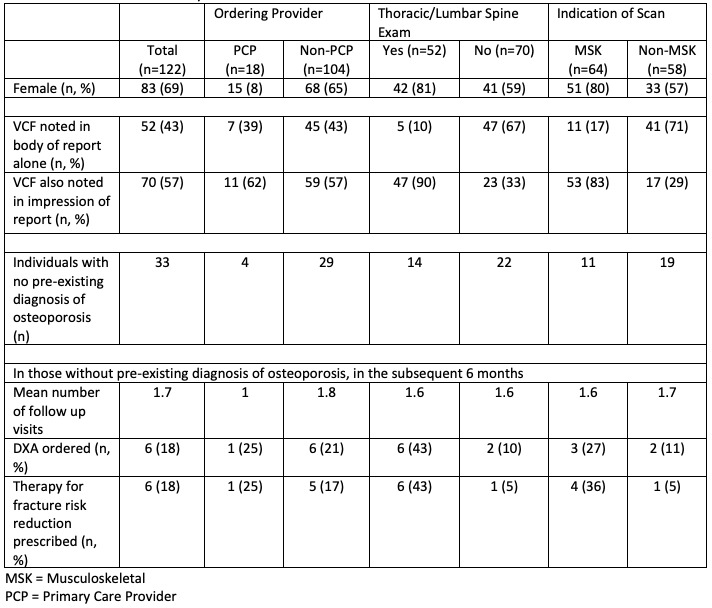 Table 1: Characteristics of CT/MRI scans reviewed
Table 1: Characteristics of CT/MRI scans reviewed
Disclosures: J. Yang, None; A. Hwang, None; M. Brochu, None; K. Sabina, None; M. Malysz, None; B. Weinstein, None; J. Cheah, None.
Background/Purpose: Vertebral compression fractures (VCFs) in general represent a clinical diagnosis of osteoporosis, predisposing to an increased risk of additional fractures. However, a significant number of clinically important VCFs are asymptomatic and are only discovered on imaging studies performed for other reasons. As a result, subsequent diagnosis and management of osteoporosis in this patient group is often lacking. The aim of this study is to identify the management outcome of VCFs on CT and MRI scans within a single academic primary care practice.
Methods: CT and MRI scans of individuals aged 50 and over between October 2020 and October 2021 were reviewed from a single academic primary care primary care practice if they contained the term 'vertebral compression' in the text of the formal radiology report. Using the scan as the index event, the subsequent six months of the electronic medical record was reviewed for the number of interactions between the individual and the primary care office, as well as for an existing or new formal diagnosis of osteoporosis and what subsequent management regarding bone health and fracture risk reduction was initiated.
Results: 77 individuals (mean age 74 years, 49 female) and 122 CT/MRI scans indicated VCFs in the formal radiology report (Table 1). 18 (15%) of these scans were ordered by the primary care practice and 64 (52%) of the indications of the investigation was a musculoskeletal (MSK) complaint. 52 (43%) studies were specifically of the thoracic or lumbar spine.
44 (57%) individuals had a pre-existing diagnosis of osteoporosis. Of the 33 who did not, in the subsequent six months, there was a mean of 1.7 follow up visits. Six (18%) had a dual energy x-ray absorptiometry scan ordered and six individuals (18%) were started on therapy for fracture risk reduction. The majority of individuals without a pre-existing diagnosis of osteoporosis who were subsequently prescribed therapies for future fracture risk reduction were those who underwent an imaging study specifically of the thoracic or lumbar spine (43%) or where the indication of the study was musculoskeletal (36%).
Conclusion: The majority of individuals who had an advanced imaging test which identified a VCF had a pre-existing diagnosis of osteoporosis. However, in those that did not, further assessment and initiation of therapy for future fracture risk reduction was low. Future work will aim to identify specific interventions to better enable further investigation and management of those with incidentally noted VCFs, but without a pre-existing diagnosis of osteoporosis.
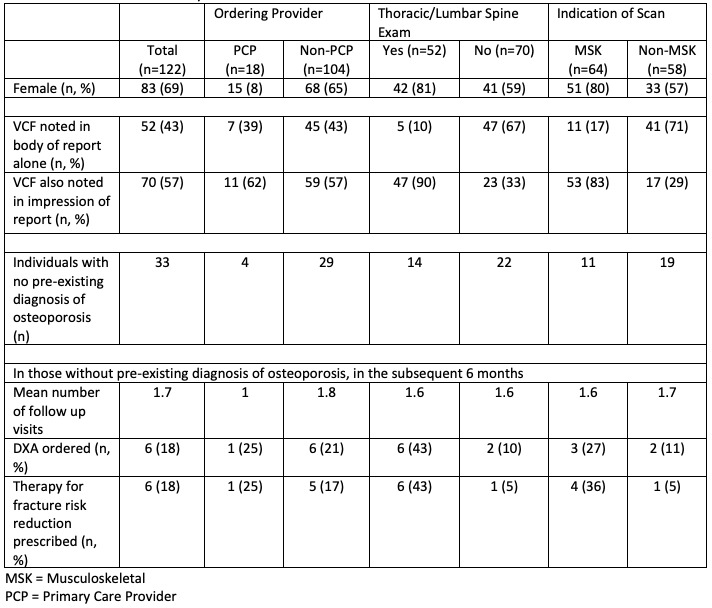 Table 1: Characteristics of CT/MRI scans reviewed
Table 1: Characteristics of CT/MRI scans reviewedDisclosures: J. Yang, None; A. Hwang, None; M. Brochu, None; K. Sabina, None; M. Malysz, None; B. Weinstein, None; J. Cheah, None.

