Back
Poster Session C
Rheumatoid arthritis (RA)
Session: (1387–1416) RA – Diagnosis, Manifestations, and Outcomes Poster III
1403: Herpes Zoster in Rheumatoid Arthritis: Prospective Single University Center Study
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- LD
Lucia Cristina Dominguez Casas, MD
Hospital Universtario San Agustin
Oviedo, Spain
Abstract Poster Presenter(s)
Lucia Cristina Dominguez Casas1, Mª Paz Rodriguez Cundin2, Trinidad Dierssen Sotos3, Nuria Vegas Revenga4, Alfonso Corrales5, Miguel Ángel González-Gay6 and Ricardo Blanco7, 1Hospital Universtario San Agustin, Oviedo, Spain, 2Hospital Universitario Marqués de Valdecilla, Santander, Spain, 3Universidad de Cantabria, Santander, Spain, 4Hospital Galdakao- Usansolo, Galdakao, Spain, 5Research Group on Genetic Epidemiology and Atherosclerosis in Systemic Diseases and in Metabolic Bone Diseases of the Musculoskeletal System, IDIVAL; and Department of Rheumatology, Hospital Universitario Marqués de Valdecilla, Santander, Spain, 6Department of Medicine and Psychiatry, Universidad de Cantabria; Rheumatology Division, Hospital Universitario Marqués de Valdecilla; Research group on genetic epidemiology and atherosclerosis in systemic diseases and in metabolic diseases of the musculoskeletal system, IDIVAL, Santander, Spain. Cardiovascular Pathophysiology and Genomics Research Unit, School of Physiology, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa, 7Hospital Universitario Marqués de Valdecilla, IDIVAL, Santander, Spain
Background/Purpose: Patients with Rheumatoid arthritis (RA) have an increased risk of infections due to the disease itself, and/or immunosuppressive therapy. The risk of herpes zoster (HZ) including disseminated HZ is also increased (1).
Our objective in this study was to asses in an unselected series of RA patients theprevalence, general features and predictive factors of HZ.
Methods: Study of 393 RA patients included in the prospective vaccination program of the Preventive Medicine and Rheumatology department of a University hospital, from October 2011 to October 2016. The minimum follow-up was of 12 months; therefore, it was made until December 2020.
HZ vaccination is not included in our vaccination program.
RA was diagnosed according to the ACR/EULAR 2010 criteria. HZ was diagnosed if presented: characteristic skin rash and blisters, paresthesia and local pain, in one (localized) or more dermatomes (generalized).
Information on patients and HZ characteristics was retrieved from the hospital and general physician records.
Results: We studied 393 patients (310 women), mean age 61.5±11.9 years. They were followed-up during a mean period of 82.6±15.2 months(range; 50 months-9 years). HZ infection was observed in 31 of 393 patients (7.9%) (26 women); mean age 67.5±11.6ys.
Prevalence of HZ in this period (122months) was 7.88% with an annual incidence rate of 0.73/100 patients/year.
A comparison between patients with and without HZ was performed (Table 1).
HZ locations were intercostal (n=6), dorsal (5), abdominal (3), lumbar (3), facial (3), cervical (1), gluteus (1), submmamary fold (1), intermmamary fold (1) and upper extremity (1).
Main HZ complications were post-herpetic neuralgia (n=7), visual alteration in facial HZ (n=1) and disseminated HZ(n=1). HZ treatment was anitiviral agents (n=23) (brivudine=7; acyclovir 6; famciclovir6; valaciclovir4), topic (n=2) and none (n=6).
Predictive factors for HZ(Figure 1) were older age ( >65 years), hypertension and treatment with high prednisone dose and antiTNF.
Conclusion: HZ is a relative frequent complication of RA. In our series, although are usually localized, post-herpetic neuralgia is relatively frequent. Probably to include HZ vaccine in our vaccination program of RA may be useful.
References: [1] Robert Harrington et al., J Inflamm Res, 2020 14;13:519-531
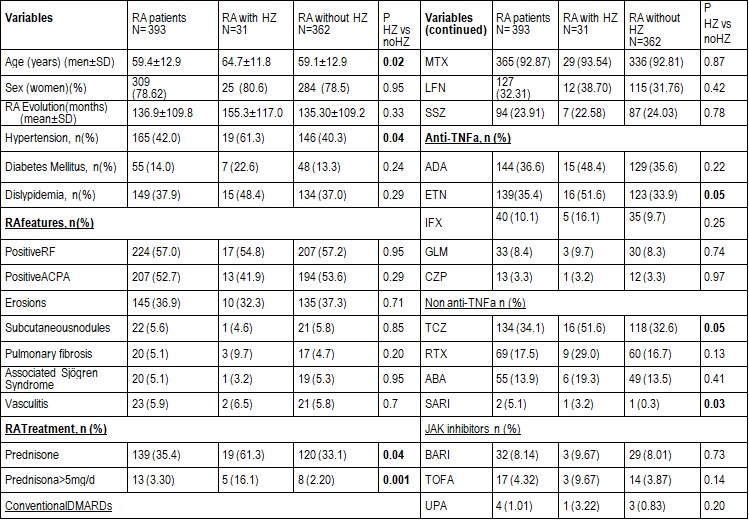 TABLE. Main features of different groups
TABLE. Main features of different groups
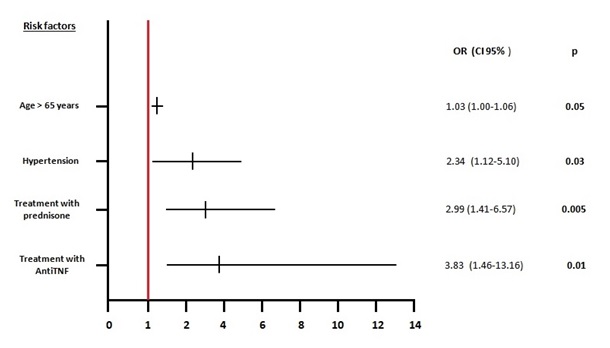 Figure. Predictive factor for Herpes zoster
Figure. Predictive factor for Herpes zoster
Disclosures: L. Dominguez Casas, None; M. Rodriguez Cundin, None; T. Dierssen Sotos, None; N. Vegas Revenga, None; A. Corrales, None; M. González-Gay, AbbVie/Abbott, Merck/MSD, Janssen, Roche, AbbVie/Abbott, Roche, Sanofi, Eli Lilly, Celgene, Sobi, Merck/MSD; R. Blanco, Eli Lilly, Pfizer, Roche, Janssen, MSD, AbbVie, Amgen, AstraZeneca, Bristol Myers Squibb, Galapagos, Novartis, Sanofi.
Background/Purpose: Patients with Rheumatoid arthritis (RA) have an increased risk of infections due to the disease itself, and/or immunosuppressive therapy. The risk of herpes zoster (HZ) including disseminated HZ is also increased (1).
Our objective in this study was to asses in an unselected series of RA patients theprevalence, general features and predictive factors of HZ.
Methods: Study of 393 RA patients included in the prospective vaccination program of the Preventive Medicine and Rheumatology department of a University hospital, from October 2011 to October 2016. The minimum follow-up was of 12 months; therefore, it was made until December 2020.
HZ vaccination is not included in our vaccination program.
RA was diagnosed according to the ACR/EULAR 2010 criteria. HZ was diagnosed if presented: characteristic skin rash and blisters, paresthesia and local pain, in one (localized) or more dermatomes (generalized).
Information on patients and HZ characteristics was retrieved from the hospital and general physician records.
Results: We studied 393 patients (310 women), mean age 61.5±11.9 years. They were followed-up during a mean period of 82.6±15.2 months(range; 50 months-9 years). HZ infection was observed in 31 of 393 patients (7.9%) (26 women); mean age 67.5±11.6ys.
Prevalence of HZ in this period (122months) was 7.88% with an annual incidence rate of 0.73/100 patients/year.
A comparison between patients with and without HZ was performed (Table 1).
HZ locations were intercostal (n=6), dorsal (5), abdominal (3), lumbar (3), facial (3), cervical (1), gluteus (1), submmamary fold (1), intermmamary fold (1) and upper extremity (1).
Main HZ complications were post-herpetic neuralgia (n=7), visual alteration in facial HZ (n=1) and disseminated HZ(n=1). HZ treatment was anitiviral agents (n=23) (brivudine=7; acyclovir 6; famciclovir6; valaciclovir4), topic (n=2) and none (n=6).
Predictive factors for HZ(Figure 1) were older age ( >65 years), hypertension and treatment with high prednisone dose and antiTNF.
Conclusion: HZ is a relative frequent complication of RA. In our series, although are usually localized, post-herpetic neuralgia is relatively frequent. Probably to include HZ vaccine in our vaccination program of RA may be useful.
References: [1] Robert Harrington et al., J Inflamm Res, 2020 14;13:519-531
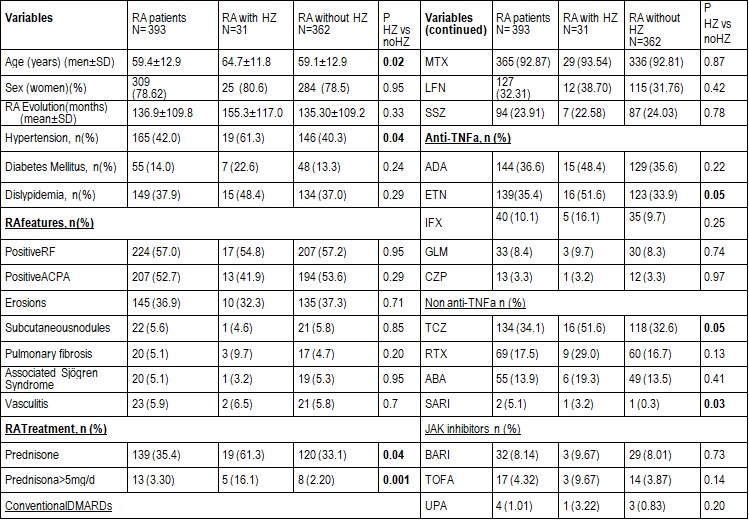 TABLE. Main features of different groups
TABLE. Main features of different groups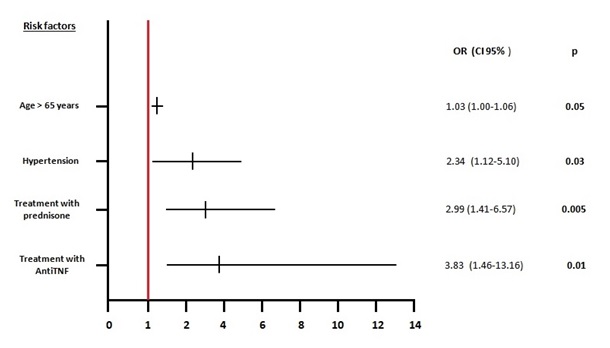 Figure. Predictive factor for Herpes zoster
Figure. Predictive factor for Herpes zosterDisclosures: L. Dominguez Casas, None; M. Rodriguez Cundin, None; T. Dierssen Sotos, None; N. Vegas Revenga, None; A. Corrales, None; M. González-Gay, AbbVie/Abbott, Merck/MSD, Janssen, Roche, AbbVie/Abbott, Roche, Sanofi, Eli Lilly, Celgene, Sobi, Merck/MSD; R. Blanco, Eli Lilly, Pfizer, Roche, Janssen, MSD, AbbVie, Amgen, AstraZeneca, Bristol Myers Squibb, Galapagos, Novartis, Sanofi.

