Back
Poster Session C
Epidemiology, health policy and outcomes
Session: (1267–1303) Measures and Measurement of Healthcare Quality Poster
1299: Hitting the Target Together: Supporting Shared Decision-Making with Juvenile Idiopathic Arthritis (JIA) Patients Followed in the Out-Patient Rheumatology Setting at the Hospital for Sick Children
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- JM
Jo Anne Marcuz, PT
The Hospital for Sick Children
Toronto, ON, Canada
Abstract Poster Presenter(s)
Jo-Anne Marcuz1, Brian Feldman2, Y. Ingrid Goh3, Niina Kim4, Piya Lahiry5, Deborah Levy2, Elizaveta Limenis6, Jeanine McColl7, Christine O'Brien8, Susan Paetkau4, Shirley Tse2, Kristi Whitney8 and Ronald Laxer2, 1Division of Rheumatology and Department of Rehabilitation, The Hospital for Sick Children; University of Toronto, Toronto, ON, Canada, 2Division of Rheumatology, The Hospital for Sick Children; Child Health Evaluative Services, SickKids Research Institute; Department of Paediatrics, University of Toronto, Toronto, ON, Canada, 3Division of Rheumatology, The Hospital for Sick Children; Child Health Evaluative Services, SickKids Research Institute, Toronto, ON, Canada, 4The Hospital for Sick Children, Toronto, ON, Canada, 5Division of Rheumatology, The Hospital for Sick Children; Department of Pediatrics, University of Toronto, Toronto, ON, Canada, 6Division of Rheumatology, The Hospital for Sick Children; Department of Paediatrics, University of Toronto, Toronto, ON, Canada, 7Division of Rheumatology, The Hospital for Sick Children; University of Toronto, Toronto, ON, Canada, 8Division of Rheumatology and Department of Rehabilitation, The Hospital for Sick Children, Toronto, ON, Canada
Background/Purpose: Juvenile Idiopathic Arthritis (JIA) is the most common chronic rheumatic disease in children with significant morbidity that extends into adulthood. Despite advances in effective JIA treatment over the last 15-20 years, research on treatment adherence, patient satisfaction, clinical outcomes, and self-management show a need to focus on the integration of shared decision-making (SDM). However, implementing SDM has several real and perceived barriers that hinder the success of this patient-centred, evidence-based care. The Pediatric Rheumatology Care and Outcomes Improvement Network (PR-COIN) has established a 3-step process to implementing treat to target (T2T): 1) standardized assessment and review of the clinical Juvenile Arthritis Disease Activity Score (cJADAS), a composite score of the physician global assessment (PGA), active joint count (AJC), and patient global assessment (PtGA); 2) setting a treatment target using SDM with the patient, with the cJADAS as a foundational tool; and 3) utilizing clinical decision supports. Our target was to increase completion and review of the cJADAS to >80% and implementation of T2T to 50% with JIA patients by June 2, 2022.
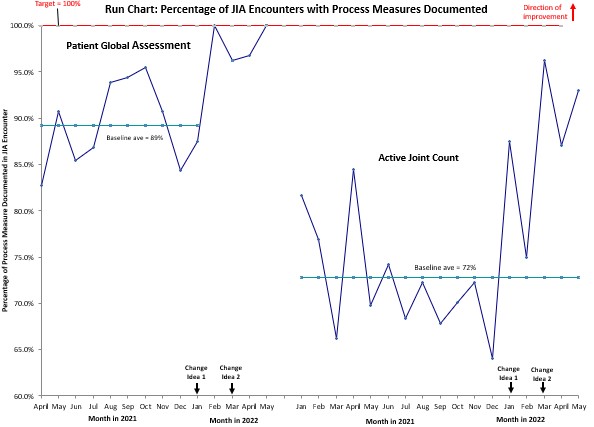
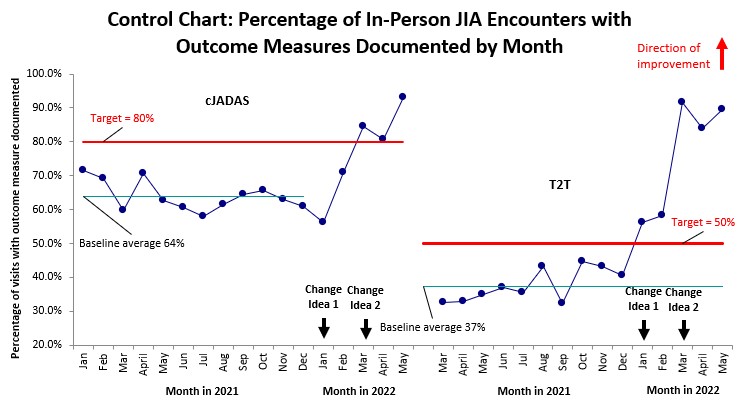
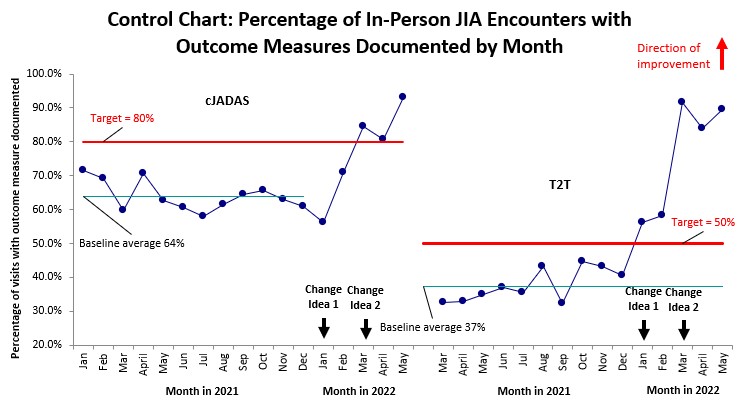
Methods: A nonrandomized, prospective, interrupted time series quality improvement project guided by the Model for Improvement (MFI) framework was initiated in January 2022 and is ongoing. In-person encounters with JIA patients who had an established diagnosis followed in two specific clinics were chosen to measure improvement.Thorough root cause analysis and development of a driver diagram led to several potential change interventions. Iterative plan-do-study-act (PDSA) cycles were then conducted, and data tracked and analyzed using run charts and control charts. Established rules were followed to determine if nonrandom signals of change and variation due to special cause were found when analyzing the data.
Results: Preliminary results up to and including May 2022 illustrate improvement in all measures. Change interventions introduced to date include (1) creation of a standard approach to JIA encounters that highlight the steps to support T2T and (2) automation of the PtGA score entry by increasing on-line completion of the patient reported outcome.There were no startup costs for this project since materials were covered under the clinical operations budget and activities did not significantly extend beyond team members' current clinical roles.
Conclusion: Preliminary results suggest successful implementation of T2T. The next steps include supporting sustainability and scaling this practice to other clinics. Although no costs were incurred, SDM has been shown in the literature to improve adherence, clinical outcomes, and enhance self-management skills, which can translate to healthcare savings in out-patient care and decreased economic burden and productivity loss in the future for pediatric patients.
.jpg) PGA = physician global assessment; PtGA = patient global assessment; AJC = active joint count; cJADAS = clinical juvenile arthritis disease activity score; T2T = treat to target (specifically “new target” documented).
PGA = physician global assessment; PtGA = patient global assessment; AJC = active joint count; cJADAS = clinical juvenile arthritis disease activity score; T2T = treat to target (specifically “new target” documented).
Disclosures: J. Marcuz, None; B. Feldman, Pfizer, AB2-Bio, Janssen; Y. Goh, None; N. Kim, None; P. Lahiry, None; D. Levy, None; E. Limenis, None; J. McColl, None; C. O'Brien, None; S. Paetkau, None; S. Tse, None; K. Whitney, None; R. Laxer, Eli Lilly, Novartis, sanofi, sobi.
Background/Purpose: Juvenile Idiopathic Arthritis (JIA) is the most common chronic rheumatic disease in children with significant morbidity that extends into adulthood. Despite advances in effective JIA treatment over the last 15-20 years, research on treatment adherence, patient satisfaction, clinical outcomes, and self-management show a need to focus on the integration of shared decision-making (SDM). However, implementing SDM has several real and perceived barriers that hinder the success of this patient-centred, evidence-based care. The Pediatric Rheumatology Care and Outcomes Improvement Network (PR-COIN) has established a 3-step process to implementing treat to target (T2T): 1) standardized assessment and review of the clinical Juvenile Arthritis Disease Activity Score (cJADAS), a composite score of the physician global assessment (PGA), active joint count (AJC), and patient global assessment (PtGA); 2) setting a treatment target using SDM with the patient, with the cJADAS as a foundational tool; and 3) utilizing clinical decision supports. Our target was to increase completion and review of the cJADAS to >80% and implementation of T2T to 50% with JIA patients by June 2, 2022.
Methods: A nonrandomized, prospective, interrupted time series quality improvement project guided by the Model for Improvement (MFI) framework was initiated in January 2022 and is ongoing. In-person encounters with JIA patients who had an established diagnosis followed in two specific clinics were chosen to measure improvement.Thorough root cause analysis and development of a driver diagram led to several potential change interventions. Iterative plan-do-study-act (PDSA) cycles were then conducted, and data tracked and analyzed using run charts and control charts. Established rules were followed to determine if nonrandom signals of change and variation due to special cause were found when analyzing the data.
Results: Preliminary results up to and including May 2022 illustrate improvement in all measures. Change interventions introduced to date include (1) creation of a standard approach to JIA encounters that highlight the steps to support T2T and (2) automation of the PtGA score entry by increasing on-line completion of the patient reported outcome.There were no startup costs for this project since materials were covered under the clinical operations budget and activities did not significantly extend beyond team members' current clinical roles.
Conclusion: Preliminary results suggest successful implementation of T2T. The next steps include supporting sustainability and scaling this practice to other clinics. Although no costs were incurred, SDM has been shown in the literature to improve adherence, clinical outcomes, and enhance self-management skills, which can translate to healthcare savings in out-patient care and decreased economic burden and productivity loss in the future for pediatric patients.
.jpg) PGA = physician global assessment; PtGA = patient global assessment; AJC = active joint count; cJADAS = clinical juvenile arthritis disease activity score; T2T = treat to target (specifically “new target” documented).
PGA = physician global assessment; PtGA = patient global assessment; AJC = active joint count; cJADAS = clinical juvenile arthritis disease activity score; T2T = treat to target (specifically “new target” documented).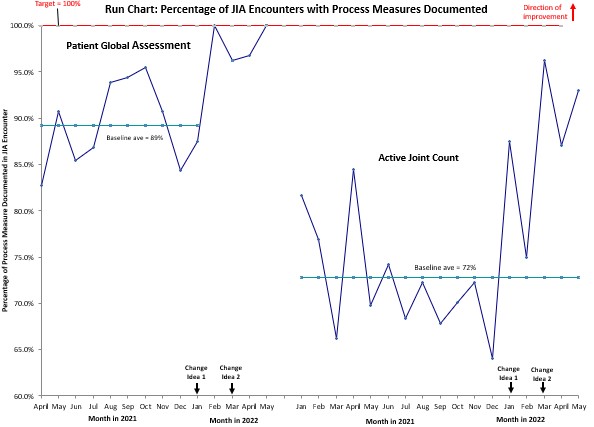
Disclosures: J. Marcuz, None; B. Feldman, Pfizer, AB2-Bio, Janssen; Y. Goh, None; N. Kim, None; P. Lahiry, None; D. Levy, None; E. Limenis, None; J. McColl, None; C. O'Brien, None; S. Paetkau, None; S. Tse, None; K. Whitney, None; R. Laxer, Eli Lilly, Novartis, sanofi, sobi.

