Back
Poster Session C
Systemic lupus erythematosus (SLE)
Session: (1440–1485) SLE – Diagnosis, Manifestations, and Outcomes Poster II: Manifestations
1455: Immune Thrombocytopenic Purpura and Subsequent Development of Systemic Lupus Erythematosus
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- GA
Gelsomina Alle, MD
Hospital Italiano de Buenos Aires
Buenos Aires, Argentina
Abstract Poster Presenter(s)
Gelsomina Alle1, Marina Scolnik1, VALERIA SCAGLIONI1, John Fredy Jaramillo Gallego1, Mayra Alejandra Tobar Jaramillo1, Rodolfo Alvarado1, Enrique R Soriano2 and Javier Eduardo Rosa1, 1Hospital Italiano de Buenos Aires, Buenos Aires, Argentina, 2Rheumatology Unit and University Institute, Hospital Italiano de Buenos Aires, Buenos Aires, Argentina
Background/Purpose: The aim of this study is to assess the incidence of Systemic Lupus Erythematosus (SLE) in a cohort of patients with Immune Thrombocytopenic Purpura (ITP), and to identify predictors for its development.
Methods: Retrospective cohort study. We included all patients with ITP treated in a University Hospital between 2000 and 2018, with at least one year of follow-up. Patients with SLE or other secondary causes of ITP were excluded. Demographic, clinical, laboratory and treatment data were recorded at diagnosis of ITP and at the end of follow-up. Patients meeting SLE classification criteria (ACR 1997 / SLICC 2012) during the follow-up were identified, and the density incidence of SLE was calculated. Patients with ITP were grouped according to the development or non-development of SLE, and comparisons between groups were made. Univariate analysis was performed to identify factors associated with the future development of SLE.
Results: 186 patients were included, 64.5% (95%) women, with a median age of 27.2 years (IQR 6.3-63.9). After a follow-up of 1801.4 person/years (py), 10 patients (5.4%) developed SLE, with a median time of 22.9 months (IQR 9.8-60.9) between ITP diagnosis and development of SLE. The incidence density of SLE was 5.6/1000 py (95% CI 2.9-9.9/1000 py). The characteristics of both groups are shown in Table 1.
At diagnosis of ITP, only 31 patients (16.7%) were assessed by a rheumatologist. Patients who developed SLE had significantly higher proportion of chronic ITP (80% vs 40.3%; p=0.01), lower proportion of complete response (10% vs 54.6%; p=0.006), and more relapses (60% vs 30.6%; p=0.05). The median duration of ITP in patients with SLE was significantly longer (67.5 vs 4 months, p< 0.001).
The presence of positive ANA (p< 0.001), nuclear homogeneous pattern (p< 0.001), ANA titres ≥1/640 (p=0.02), hypocomplementemia (p< 0.001), lupus anticoagulant (p< 0.001), polyclonal hypergammaglobulinemia (p< 0.001), leukopenia (p=0.006) and hemolytic anemia (p=0.005) were significantly associated with the future development of SLE.
Conclusion: In this cohort of patients with ITP, the incidence density of SLE was 5.6/1000 py. The most refractory course of the disease, as well as the presence of homogeneous pattern and high titre ANA, hypocomplementemia, lupus anticoagulant, polyclonal hypergammaglobulinemia and other cytopenias were significantly associated with the subsequent development of SLE.
.jpg) Baseline characteristics at ITP diagnosis and comparison between groups
Baseline characteristics at ITP diagnosis and comparison between groups
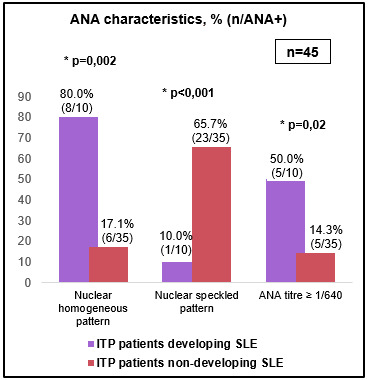 ANA characteristics at ITP diagnosis
ANA characteristics at ITP diagnosis
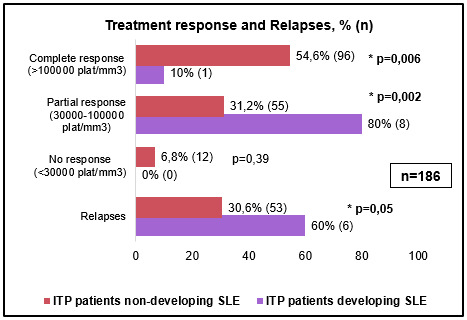 Treatment response and Relapses
Treatment response and Relapses
Disclosures: G. Alle, None; M. Scolnik, AbbVie/Abbott, Amgen, Bristol-Myers Squibb(BMS), Eli Lilly, Janssen, Pfizer, GlaxoSmithKlein(GSK), Roche; V. SCAGLIONI, None; J. Jaramillo Gallego, None; M. Tobar Jaramillo, None; R. Alvarado, None; E. Soriano, AbbVie, Amgen, Bristol-Myers Squibb(BMS), Eli Lilly, Janssen, Novartis, Pfizer, UCB, Roche; J. Rosa, Eli Lilly, AbbVie/Abbott, Bristol-Myers Squibb(BMS), Amgen, Novartis, Pfizer.
Background/Purpose: The aim of this study is to assess the incidence of Systemic Lupus Erythematosus (SLE) in a cohort of patients with Immune Thrombocytopenic Purpura (ITP), and to identify predictors for its development.
Methods: Retrospective cohort study. We included all patients with ITP treated in a University Hospital between 2000 and 2018, with at least one year of follow-up. Patients with SLE or other secondary causes of ITP were excluded. Demographic, clinical, laboratory and treatment data were recorded at diagnosis of ITP and at the end of follow-up. Patients meeting SLE classification criteria (ACR 1997 / SLICC 2012) during the follow-up were identified, and the density incidence of SLE was calculated. Patients with ITP were grouped according to the development or non-development of SLE, and comparisons between groups were made. Univariate analysis was performed to identify factors associated with the future development of SLE.
Results: 186 patients were included, 64.5% (95%) women, with a median age of 27.2 years (IQR 6.3-63.9). After a follow-up of 1801.4 person/years (py), 10 patients (5.4%) developed SLE, with a median time of 22.9 months (IQR 9.8-60.9) between ITP diagnosis and development of SLE. The incidence density of SLE was 5.6/1000 py (95% CI 2.9-9.9/1000 py). The characteristics of both groups are shown in Table 1.
At diagnosis of ITP, only 31 patients (16.7%) were assessed by a rheumatologist. Patients who developed SLE had significantly higher proportion of chronic ITP (80% vs 40.3%; p=0.01), lower proportion of complete response (10% vs 54.6%; p=0.006), and more relapses (60% vs 30.6%; p=0.05). The median duration of ITP in patients with SLE was significantly longer (67.5 vs 4 months, p< 0.001).
The presence of positive ANA (p< 0.001), nuclear homogeneous pattern (p< 0.001), ANA titres ≥1/640 (p=0.02), hypocomplementemia (p< 0.001), lupus anticoagulant (p< 0.001), polyclonal hypergammaglobulinemia (p< 0.001), leukopenia (p=0.006) and hemolytic anemia (p=0.005) were significantly associated with the future development of SLE.
Conclusion: In this cohort of patients with ITP, the incidence density of SLE was 5.6/1000 py. The most refractory course of the disease, as well as the presence of homogeneous pattern and high titre ANA, hypocomplementemia, lupus anticoagulant, polyclonal hypergammaglobulinemia and other cytopenias were significantly associated with the subsequent development of SLE.
.jpg) Baseline characteristics at ITP diagnosis and comparison between groups
Baseline characteristics at ITP diagnosis and comparison between groups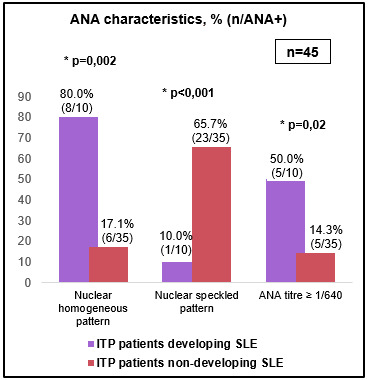 ANA characteristics at ITP diagnosis
ANA characteristics at ITP diagnosis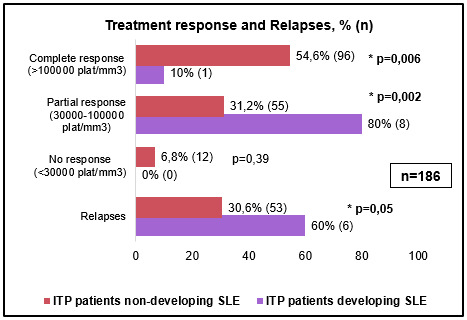 Treatment response and Relapses
Treatment response and RelapsesDisclosures: G. Alle, None; M. Scolnik, AbbVie/Abbott, Amgen, Bristol-Myers Squibb(BMS), Eli Lilly, Janssen, Pfizer, GlaxoSmithKlein(GSK), Roche; V. SCAGLIONI, None; J. Jaramillo Gallego, None; M. Tobar Jaramillo, None; R. Alvarado, None; E. Soriano, AbbVie, Amgen, Bristol-Myers Squibb(BMS), Eli Lilly, Janssen, Novartis, Pfizer, UCB, Roche; J. Rosa, Eli Lilly, AbbVie/Abbott, Bristol-Myers Squibb(BMS), Amgen, Novartis, Pfizer.

