Back
Poster Session C
Systemic lupus erythematosus (SLE)
Session: (1440–1485) SLE – Diagnosis, Manifestations, and Outcomes Poster II: Manifestations
1450: Impact of Time to Remission, Flares and Time on Immunosuppressives on the Estimated Glomerular Filtration Rate in Lupus Nephritis
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- KT
Konstantinos Tselios, MD, PhD
McMaster University
Hamilton, ON, Canada
Abstract Poster Presenter(s)
KONSTANTINOS TSELIOS1, Dafna Gladman2, Jiandong Su3 and Murray Urowitz4, 1McMaster University, Population Health Research Institute, Hamilton, ON, Canada, 2Toronto Western Hospital, Schroeder Arthritis Institute, Toronto, ON, Canada, 3Schroeder Arthritis Institute, Krembil Research Institute, University Health Network and University of Toronto, Toronto, ON, Canada, 4University of Toronto, University Health Network, Schroeder Arthritis Institute, Toronto, ON, Canada
Background/Purpose: Time to complete remission, subsequent flares and time on immunosuppressives after complete remission are major determinants of the progression to advanced chronic kidney disease in lupus nephritis (LN). However, the impact of these factors on the rate of glomerular filtration rate (GFR) deterioration is not known.
Objective: To determine the impact of time to remission, flares and time on immunosuppressives after remission on the estimated GFR in LN.
Methods: Patients with LN based on biopsy or abnormal proteinuria ( >0.5g/day) with or without hematuria or pyuria or casts for two consecutive visits were retrieved from the Toronto Lupus Clinic long-term longitudinal database. Individuals with advanced chronic kidney disease at baseline (eGFR≦29ml/min/1.73m2) were excluded. All patients were followed for at least 5 years. The primary outcome was any decrease of the estimated GFR on an annual basis (slope). Remission was defined as proteinuria< 0.5g/24h, inactive urinary sediment and serum creatinine ≤120% of the baseline value. Flare was defined as any abnormal proteinuria ( >0.5g/day) or increase in serum creatinine (SCR) from normal to abnormal or >120% of the baseline value after remission. Slopes of eGFR changes (standard error) were calculated using Ordinary Least Square method in each complete remission/flare group. Linear Mixed model was performed to account for factors associated with deterioration of eGFR.
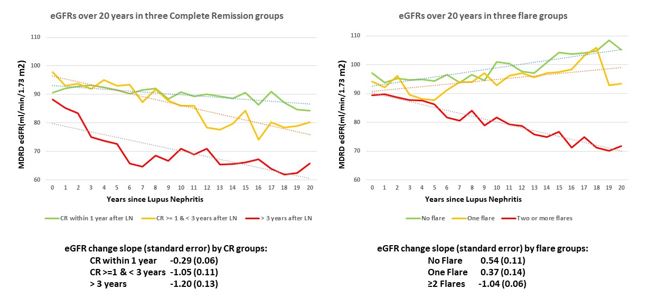
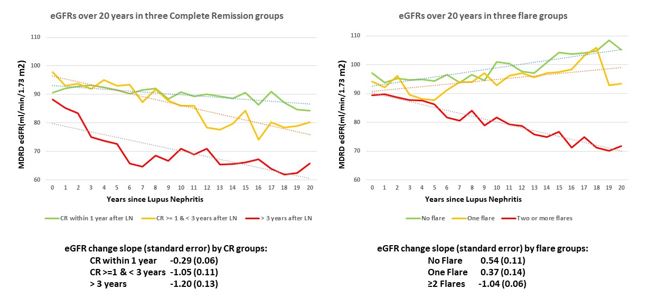
Results: Out of 418 eligible patients, 209 (50%) achieved remission within the first year from LN diagnosis, 102 (24.4%) within the 2nd and 3rd years, 70 (16.7%) after 3 years and 37 (8.9%) never achieved remission. Regarding flares, 82 patients (19.6%) never flared, 75 (18%) had one flare and 261 (62.4%) had two or more flares. The trajectory and annual slope of eGFR according to time to remission and number of flares is shown in the Figure.
Regression analysis (linear mixed model) for the outcome of eGFR was performed to adjust for other variables that impact eGFR (Table).
Conclusion: Complete remission after 3 years or no remission is associated with a significant decrease in eGFR, while remission during the 2nd and 3rd year from LN diagnosis is not associated with significant decrease of renal function over time. Patients with one flare did not have significant impact on their renal function. Patients with 2 or more flares had a significant decrease of eGFR over 20 years, even after adjustment for other covariates. Time on immunosuppressives after complete remission is protective against eGFR decline. Our findings emphasize the importance of rapid remission and flare prevention by prolonged maintenance treatment with immunosuppressives to optimize renal outcomes.
.jpg)
Disclosures: K. TSELIOS, AstraZeneca, GlaxoSmithKlein(GSK); D. Gladman, AbbVie, Amgen, Eli Lilly, Janssen, Gilead, Novartis, Pfizer, Bristol-Myers Squibb(BMS), Galapagos, UCB Pharma, Celgene; J. Su, None; M. Urowitz, None.
Background/Purpose: Time to complete remission, subsequent flares and time on immunosuppressives after complete remission are major determinants of the progression to advanced chronic kidney disease in lupus nephritis (LN). However, the impact of these factors on the rate of glomerular filtration rate (GFR) deterioration is not known.
Objective: To determine the impact of time to remission, flares and time on immunosuppressives after remission on the estimated GFR in LN.
Methods: Patients with LN based on biopsy or abnormal proteinuria ( >0.5g/day) with or without hematuria or pyuria or casts for two consecutive visits were retrieved from the Toronto Lupus Clinic long-term longitudinal database. Individuals with advanced chronic kidney disease at baseline (eGFR≦29ml/min/1.73m2) were excluded. All patients were followed for at least 5 years. The primary outcome was any decrease of the estimated GFR on an annual basis (slope). Remission was defined as proteinuria< 0.5g/24h, inactive urinary sediment and serum creatinine ≤120% of the baseline value. Flare was defined as any abnormal proteinuria ( >0.5g/day) or increase in serum creatinine (SCR) from normal to abnormal or >120% of the baseline value after remission. Slopes of eGFR changes (standard error) were calculated using Ordinary Least Square method in each complete remission/flare group. Linear Mixed model was performed to account for factors associated with deterioration of eGFR.
Results: Out of 418 eligible patients, 209 (50%) achieved remission within the first year from LN diagnosis, 102 (24.4%) within the 2nd and 3rd years, 70 (16.7%) after 3 years and 37 (8.9%) never achieved remission. Regarding flares, 82 patients (19.6%) never flared, 75 (18%) had one flare and 261 (62.4%) had two or more flares. The trajectory and annual slope of eGFR according to time to remission and number of flares is shown in the Figure.
Regression analysis (linear mixed model) for the outcome of eGFR was performed to adjust for other variables that impact eGFR (Table).
Conclusion: Complete remission after 3 years or no remission is associated with a significant decrease in eGFR, while remission during the 2nd and 3rd year from LN diagnosis is not associated with significant decrease of renal function over time. Patients with one flare did not have significant impact on their renal function. Patients with 2 or more flares had a significant decrease of eGFR over 20 years, even after adjustment for other covariates. Time on immunosuppressives after complete remission is protective against eGFR decline. Our findings emphasize the importance of rapid remission and flare prevention by prolonged maintenance treatment with immunosuppressives to optimize renal outcomes.
.jpg)
Disclosures: K. TSELIOS, AstraZeneca, GlaxoSmithKlein(GSK); D. Gladman, AbbVie, Amgen, Eli Lilly, Janssen, Gilead, Novartis, Pfizer, Bristol-Myers Squibb(BMS), Galapagos, UCB Pharma, Celgene; J. Su, None; M. Urowitz, None.

