Back
Poster Session C
Vasculitis
Session: (1543–1578) Vasculitis – Non-ANCA-Associated and Related Disorders Poster II
1545: Increased Neutrophil Activation in Patients with Polymyalgia Rheumatica
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- DM
Despoina Michailidou, MD
University of Washington
Seattle, WA, United States
Abstract Poster Presenter(s)
Despina Michailidou1, Linda Johansson2, Runa Kuley1, TING WANG1, Payton Hermanson1, Solbritt Rantapää-Dahlqvist2 and Christian Lood1, 1Division of Rheumatology, University of Washington, Seattle, WA, 2Department of Public Health and Clinical Medicine, Rheumatology, Umeå University, Umeå, Sweden
Background/Purpose: Neutrophils are important in host defense. However, neutrophil activation has also been involved in the immunopathogenesis of several autoimmune diseases due to their many cytotoxic and inflammatory effector mechanisms. The purpose of this study was to assess whether neutrophil activation occurs in polymyalgia rheumatica (PMR) by evaluating circulating levels of calprotectin and neutrophil extracellular traps (NETs).
Methods: Levels of calprotectin and NETs, as assessed by myeloperoxidase (MPO)-DNA complexes, were measured in the plasma of healthy individuals (n=30) and patients with PMR (n=60) using ELISA. PMR patients were enrolled at time-point of active disease, as well as following glucocorticoid therapy (Table 1).
Results: Levels of calprotectin and NETs were elevated in patients with PMR as compared to healthy subjects (Table 2). The neutrophil activation marker, calprotectin, significantly decreased after corticosteroid therapy (p< 0.001) (Table 3), and was higher in patients with active PMR without overlapping GCA compared to patients with overlapping disease (p=0.014). Interestingly, musculoskeletal involvement as defined by pain and stiffness in shoulder and pelvic girdles was associated with elevated levels of calprotectin (p=0.036) before initiation of corticosteroid therapy.
Conclusion: Neutrophil activation occurs in patients with PMR and was associated with musculoskeletal involvement. Plasma calprotectin could be a reliable biomarker of treatment response in patients with PMR. However, NETs are not a sensitive predictive biomarker for reduction of systemic inflammation in PMR.
.jpg) Table 1. Baseline demographic characteristics of patients with PMR
Table 1. Baseline demographic characteristics of patients with PMR
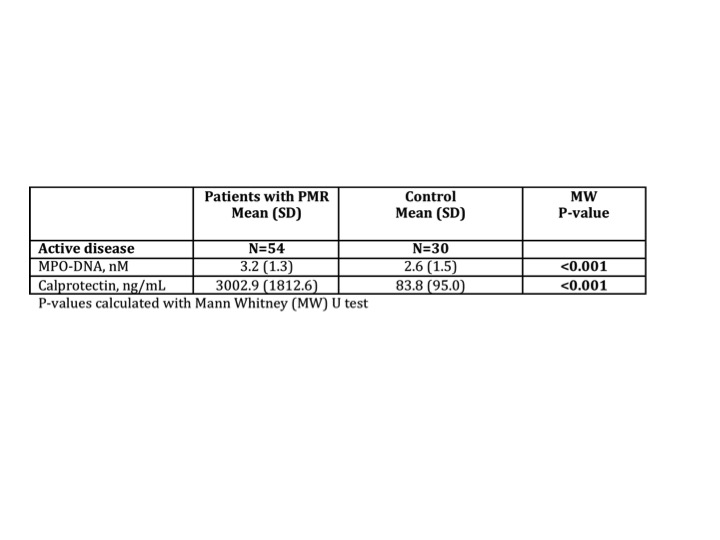 Table 2. Mean concentration of neutrophil markers, in patients with active PMR before corticosteroid therapy compared to healthy controls
Table 2. Mean concentration of neutrophil markers, in patients with active PMR before corticosteroid therapy compared to healthy controls
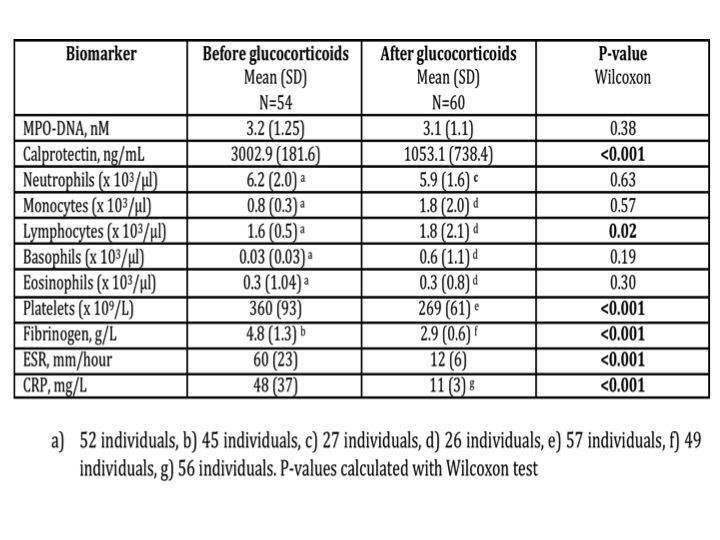 Table 3. Mean concentration of neutrophil markers, blood cell counts, and acute phase reactants before and after glucocorticoid treatment in patients with PMR.
Table 3. Mean concentration of neutrophil markers, blood cell counts, and acute phase reactants before and after glucocorticoid treatment in patients with PMR.
Disclosures: D. Michailidou, Chemocentryx, Pfizer US Pharmaceuticals Group; L. Johansson, None; R. Kuley, None; T. WANG, None; P. Hermanson, None; S. Rantapää-Dahlqvist, None; C. Lood, Eli Lilly, Gilead Sciences, Pfizer, Bristol-Myers Squibb(BMS), Redd Pharma, Horizon Diagnostic, Exagen Diagnostic.
Background/Purpose: Neutrophils are important in host defense. However, neutrophil activation has also been involved in the immunopathogenesis of several autoimmune diseases due to their many cytotoxic and inflammatory effector mechanisms. The purpose of this study was to assess whether neutrophil activation occurs in polymyalgia rheumatica (PMR) by evaluating circulating levels of calprotectin and neutrophil extracellular traps (NETs).
Methods: Levels of calprotectin and NETs, as assessed by myeloperoxidase (MPO)-DNA complexes, were measured in the plasma of healthy individuals (n=30) and patients with PMR (n=60) using ELISA. PMR patients were enrolled at time-point of active disease, as well as following glucocorticoid therapy (Table 1).
Results: Levels of calprotectin and NETs were elevated in patients with PMR as compared to healthy subjects (Table 2). The neutrophil activation marker, calprotectin, significantly decreased after corticosteroid therapy (p< 0.001) (Table 3), and was higher in patients with active PMR without overlapping GCA compared to patients with overlapping disease (p=0.014). Interestingly, musculoskeletal involvement as defined by pain and stiffness in shoulder and pelvic girdles was associated with elevated levels of calprotectin (p=0.036) before initiation of corticosteroid therapy.
Conclusion: Neutrophil activation occurs in patients with PMR and was associated with musculoskeletal involvement. Plasma calprotectin could be a reliable biomarker of treatment response in patients with PMR. However, NETs are not a sensitive predictive biomarker for reduction of systemic inflammation in PMR.
.jpg) Table 1. Baseline demographic characteristics of patients with PMR
Table 1. Baseline demographic characteristics of patients with PMR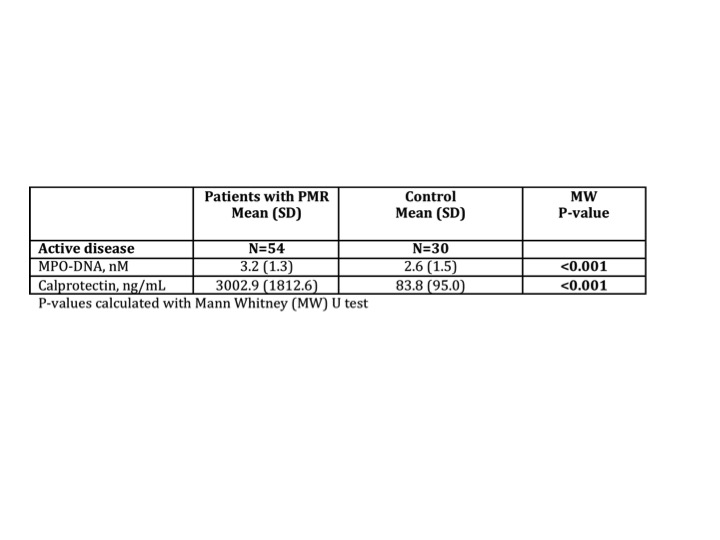 Table 2. Mean concentration of neutrophil markers, in patients with active PMR before corticosteroid therapy compared to healthy controls
Table 2. Mean concentration of neutrophil markers, in patients with active PMR before corticosteroid therapy compared to healthy controls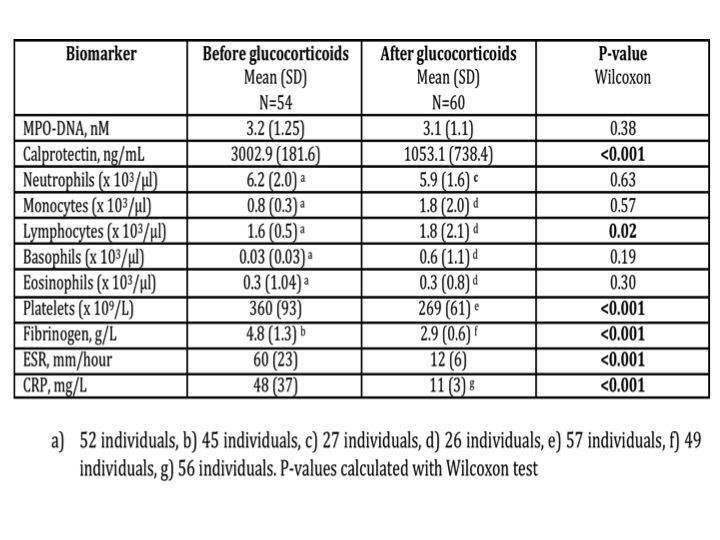 Table 3. Mean concentration of neutrophil markers, blood cell counts, and acute phase reactants before and after glucocorticoid treatment in patients with PMR.
Table 3. Mean concentration of neutrophil markers, blood cell counts, and acute phase reactants before and after glucocorticoid treatment in patients with PMR.Disclosures: D. Michailidou, Chemocentryx, Pfizer US Pharmaceuticals Group; L. Johansson, None; R. Kuley, None; T. WANG, None; P. Hermanson, None; S. Rantapää-Dahlqvist, None; C. Lood, Eli Lilly, Gilead Sciences, Pfizer, Bristol-Myers Squibb(BMS), Redd Pharma, Horizon Diagnostic, Exagen Diagnostic.

