Back
Poster Session C
Systemic lupus erythematosus (SLE)
Session: (1440–1485) SLE – Diagnosis, Manifestations, and Outcomes Poster II: Manifestations
1482: Latent Tuberculosis Infection and Its Associations with Clinical and Serological Parameters in Systemic Lupus Erythematosus
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- GM
Gayathri M.S., MD, MBBS
JIPMER, Puducherry
Puducherry, Puducherry, India
Abstract Poster Presenter(s)
Gayathri MS1, Chengappa Kavadichanda2, Aishwarya Gopal3, Devender Bairwa4, Molly Thabah1, Sonali Sarkar5 and Prakash Babu Narasimhan1, 1Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, Puducherry, India, 2JIPMER, Pondicherry, Puducherry, India, 3Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Pondicherry, Puducherry, India, 4Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Puducherry, Puducherry, India, 5Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, India
Background/Purpose: Latent tuberculosis infection (L-TB) detected by mycobacterium tuberculosis (TB) IFN-γ release assay (TB-IGRA), besides identifying latent infection may predict the disease status in SLE. Identifying the clinical and serological associations of LTB in lupus may be an important step in preventing progressing to overt TB in lupus. This is especially true in high endemic countries like India. This study aimed to assess the prevalence of L-TB, its association with clinical and serological parameters in SLE
Methods: This is a single center cross sectional study. Adults with SLE with no past h/o TB were recruited (n=219). Demography, disease activity indices, autoantibody profile and steroid use were noted. Presence of Latent TB was assessed in all patients using TB-IGRA. Based on the results of TB-IGRA, SLE cases were divided into 2 groups-IGRA positive and IGRA negative. The collected parameters were compared between the 2 groups. Correlation of disease activity was assessed with the IFN g levels in the unstimulated tube of TB IGRA to assess baseline immune activation in SLE.
Results: Among 219 patients, 41 had latent TB resulting in a point prevalence of 18.7 %. The average disease duration was 3 years in IGRA positive and 4.1 in IGRA negative group(p >0.05). Among antibody profile, proportion of Ro 52 was higher in IGRA positive group(43.9%)than IGRA negative group(25.3%) (p=0.014) and proportion aCLA IgM antibody higher in IGRA negative group (12.9%) than positive group (2.4%) (p=0.032). Comparison of clinical features yielded no statistically significant difference in the 2 groups. Serology revealed greater proportion of low C4 in IGRA negative as compared to the positive group(p=0.036). There was no correlation of SLE disease activity with the IFN g levels in the unstimulated tube of TB IGRA.
Conclusion: Prevalence of latent TB in SLE cases was 18.7% which is lesser than latent TB prevalence in the general population (40%). Higher association of anti-Ro 52 antibody in IGRA positive group along with higher aCLA IgM and low C4 in IGRA negative group were found whose physiological significance is unknown. IFNg levels in the unstimulated tube of TB IGRA did not seem to correlate with SLE disease activity. Further studies would be required to throw more light on the interplay between latent TB and SLE.
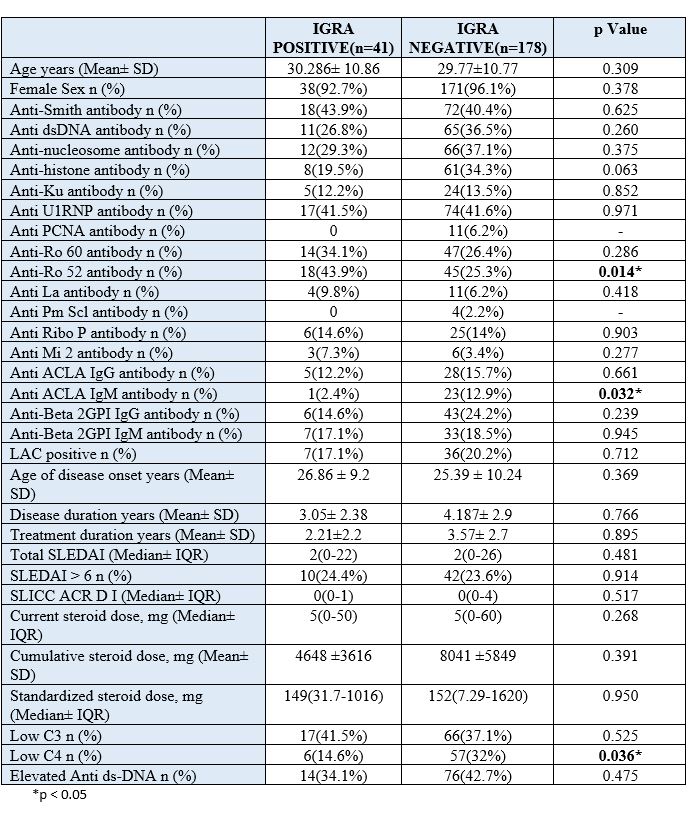 Comparison of clinical and laboratory parameters between IGRA positive and IGRA negative SLE cases
Comparison of clinical and laboratory parameters between IGRA positive and IGRA negative SLE cases
Disclosures: G. MS, None; C. Kavadichanda, None; A. Gopal, None; D. Bairwa, None; M. Thabah, None; S. Sarkar, None; P. Narasimhan, None.
Background/Purpose: Latent tuberculosis infection (L-TB) detected by mycobacterium tuberculosis (TB) IFN-γ release assay (TB-IGRA), besides identifying latent infection may predict the disease status in SLE. Identifying the clinical and serological associations of LTB in lupus may be an important step in preventing progressing to overt TB in lupus. This is especially true in high endemic countries like India. This study aimed to assess the prevalence of L-TB, its association with clinical and serological parameters in SLE
Methods: This is a single center cross sectional study. Adults with SLE with no past h/o TB were recruited (n=219). Demography, disease activity indices, autoantibody profile and steroid use were noted. Presence of Latent TB was assessed in all patients using TB-IGRA. Based on the results of TB-IGRA, SLE cases were divided into 2 groups-IGRA positive and IGRA negative. The collected parameters were compared between the 2 groups. Correlation of disease activity was assessed with the IFN g levels in the unstimulated tube of TB IGRA to assess baseline immune activation in SLE.
Results: Among 219 patients, 41 had latent TB resulting in a point prevalence of 18.7 %. The average disease duration was 3 years in IGRA positive and 4.1 in IGRA negative group(p >0.05). Among antibody profile, proportion of Ro 52 was higher in IGRA positive group(43.9%)than IGRA negative group(25.3%) (p=0.014) and proportion aCLA IgM antibody higher in IGRA negative group (12.9%) than positive group (2.4%) (p=0.032). Comparison of clinical features yielded no statistically significant difference in the 2 groups. Serology revealed greater proportion of low C4 in IGRA negative as compared to the positive group(p=0.036). There was no correlation of SLE disease activity with the IFN g levels in the unstimulated tube of TB IGRA.
Conclusion: Prevalence of latent TB in SLE cases was 18.7% which is lesser than latent TB prevalence in the general population (40%). Higher association of anti-Ro 52 antibody in IGRA positive group along with higher aCLA IgM and low C4 in IGRA negative group were found whose physiological significance is unknown. IFNg levels in the unstimulated tube of TB IGRA did not seem to correlate with SLE disease activity. Further studies would be required to throw more light on the interplay between latent TB and SLE.
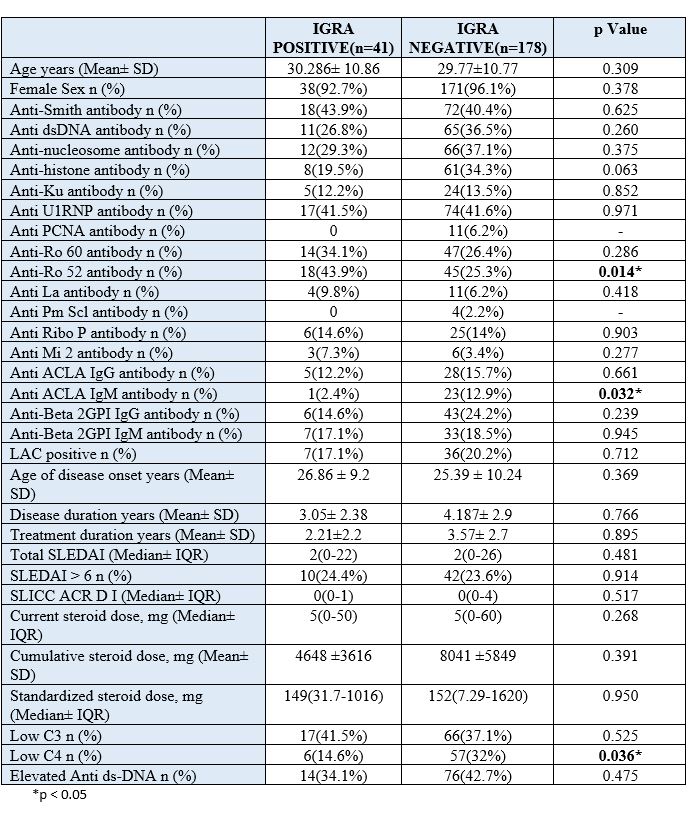 Comparison of clinical and laboratory parameters between IGRA positive and IGRA negative SLE cases
Comparison of clinical and laboratory parameters between IGRA positive and IGRA negative SLE casesDisclosures: G. MS, None; C. Kavadichanda, None; A. Gopal, None; D. Bairwa, None; M. Thabah, None; S. Sarkar, None; P. Narasimhan, None.

