Back
Poster Session C
Epidemiology, health policy and outcomes
Session: (1332–1359) Patient Outcomes, Preferences, and Attitudes Poster II
1344: Patient-reported Outcomes in Lupus Low Disease Activity State: Impact of Fatigue
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- LS
Luciana Seguro, MD, PhD
Hospital das Clinicas FMUSP
São Paulo, S�o Paulo, Brazil
Abstract Poster Presenter(s)
Rodrigo De Moura Rodrigues, Alexandre Moura dos Santos, Daniel Sampaio Cardoso, Emily Figueiredo Neves Yuki, Danieli Castro Oliveira de Andrade, Sandra Gofinet Pasoto, Eduardo Ferreira Borba Neto, Eloisa Silva Dutra de Oliveira Bonfa and Luciana Seguro, Hospital das Clinicas HCFMUSP, Faculdade de Medicina, Universidade de São Paulo, São Paulo, Brazil
Background/Purpose: Patient Reported Outcomes (PROs) can be assessed by self-administered questionnaires and can lead to better decision-making by physicians. The aim of this study was to evaluate PROs in patients with lupus low disease activity state (LLDAS) followed in a tertiary lupus specialized center.
Methods: Consecutive SLE patients (SLICC criteria) with LLDAS followed in a tertiary specialized center were included. Patients were invited to fill out the following PROs questionnaires immediately before the visit: Health Assessment Questionnaire (HAQ; score range: 0 (without any difficulty) to 3 (unable to do)); EQ5D quality of life (score range: less than 0 (poor health) to 1 (full health)), EQ5D VAS (scale range: between 100 (best imaginable health) and 0 (worst imaginable health)); Functional Assessment of Chronic Illness Therapy-Fatigue (FACIT Fatigue; score range: 0 to 52 (higher scores indicate less fatigue)); modified Morisky medication adherence scale (mMMAS; score range: 0-1: low adherence, 2-3: median adherence, 4: high adherence)). Physicians were asked to fill out SLEDAI activity index, SLICC damage index (SDI), Physician global assessment (PGA). The study was approved by the local IRB and patients read and signed the informed consent. Quantitative variables were expressed as median and interquartile [25th-75th], and qualitative variables were expressed as count and frequency (%). Correlations between variables were tested by Spearman's rank correlation test (rho). We considered it statistically significant when α ≤0.05. Statistical analysis was performed with R 4.1.2, for Windows (Vienna, Austria).
Results: 120 patients were included and 92% were female. 47% were Caucasian, 38% mestizo and 15% black. Patients had median age of 41 years [35-46] and median disease duration of 14 years [10-19]. Concerning comorbidities, 34% of patients used anti-hypertensive drugs, 3% had diabetes/pre-diabetes, 5% dyslipidemia, 7% depression, 11% osteoporosis. Median BMI was 27.10 [23.87-31.30] kg/m2. Regarding SLE treatment, median prednisone dose was 0 [0-5] mg/day; 83% used hydroxychloroquine, 24% azathioprine, 41% mycophenolate mofetil, 8% methotrexate and 3% tacrolimus. Median SLEDAI score was 0 [0-2], SDI 0 [0-1], PGA 0 [0-1]. Concerning PROs: Median HAQ score was 0.25 [0.00-0.63], EQ5D score 0.67 [0.52-0.79], EQ5D VAS 70.00 [50.00-80.00], FACIT fatigue score (subscale additional concerns) 40.00 [30.00-46.25]. 61% of patients reported high adherence level. 15% of patients had high fatigue levels (FACIT fatigue< 27). FACIT Fatigue correlated with health quality score EQ5D (rho=0.660, p< 0.001), negatively with HAQ (rho=-0.682, p< 0.001) and BMI (rho=-0.210, p=0.022).
Conclusion: The observed discordance of low disease activity and SLEDAI with fatigue suggests that physicians may not be aware of the impact of fatigue in the quality of life of inactive or low disease activity lupus patients. PROs assessment may help to recognize and improve patient care.
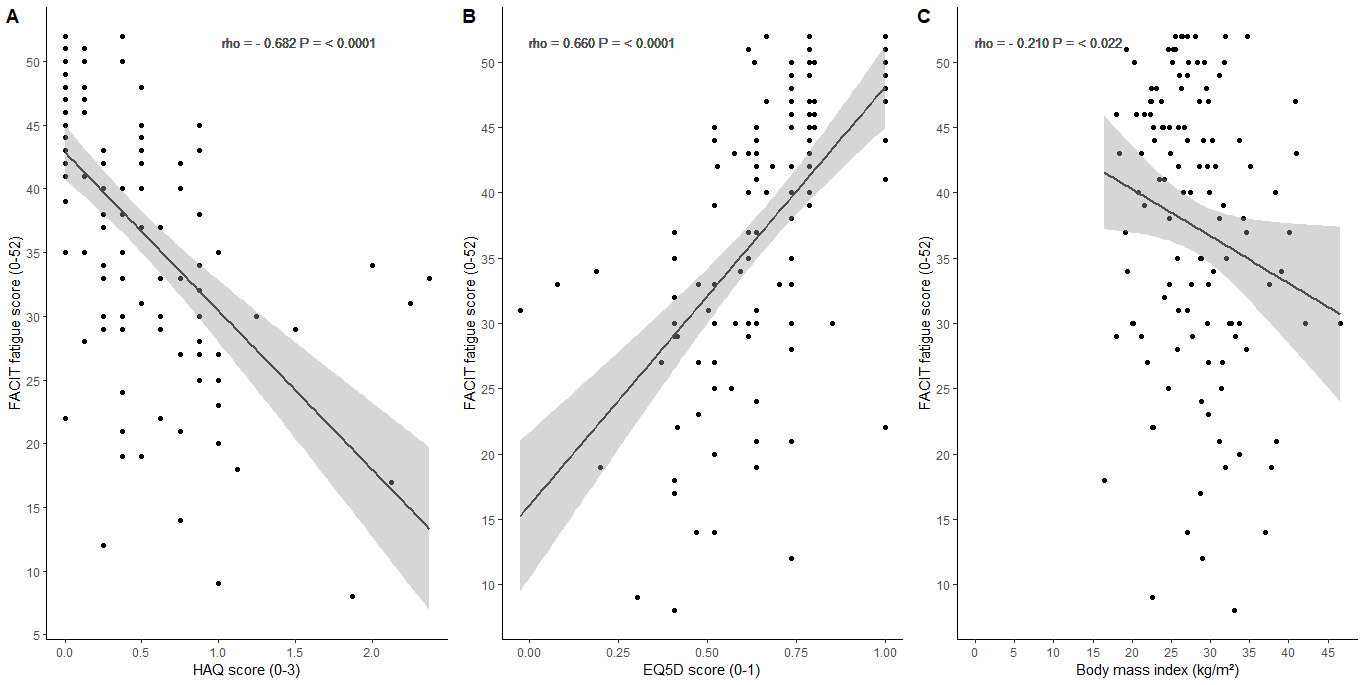 Figure 1 - Relation between FACIT fatigue score and HAQ, EQ5D and BMI, respectively.
Figure 1 - Relation between FACIT fatigue score and HAQ, EQ5D and BMI, respectively.
Disclosures: R. De Moura Rodrigues, None; A. Moura dos Santos, None; D. Sampaio Cardoso, None; E. Figueiredo Neves Yuki, None; D. Castro Oliveira de Andrade, None; S. Gofinet Pasoto, None; E. Ferreira Borba Neto, None; E. Silva Dutra de Oliveira Bonfa, None; L. Seguro, None.
Background/Purpose: Patient Reported Outcomes (PROs) can be assessed by self-administered questionnaires and can lead to better decision-making by physicians. The aim of this study was to evaluate PROs in patients with lupus low disease activity state (LLDAS) followed in a tertiary lupus specialized center.
Methods: Consecutive SLE patients (SLICC criteria) with LLDAS followed in a tertiary specialized center were included. Patients were invited to fill out the following PROs questionnaires immediately before the visit: Health Assessment Questionnaire (HAQ; score range: 0 (without any difficulty) to 3 (unable to do)); EQ5D quality of life (score range: less than 0 (poor health) to 1 (full health)), EQ5D VAS (scale range: between 100 (best imaginable health) and 0 (worst imaginable health)); Functional Assessment of Chronic Illness Therapy-Fatigue (FACIT Fatigue; score range: 0 to 52 (higher scores indicate less fatigue)); modified Morisky medication adherence scale (mMMAS; score range: 0-1: low adherence, 2-3: median adherence, 4: high adherence)). Physicians were asked to fill out SLEDAI activity index, SLICC damage index (SDI), Physician global assessment (PGA). The study was approved by the local IRB and patients read and signed the informed consent. Quantitative variables were expressed as median and interquartile [25th-75th], and qualitative variables were expressed as count and frequency (%). Correlations between variables were tested by Spearman's rank correlation test (rho). We considered it statistically significant when α ≤0.05. Statistical analysis was performed with R 4.1.2, for Windows (Vienna, Austria).
Results: 120 patients were included and 92% were female. 47% were Caucasian, 38% mestizo and 15% black. Patients had median age of 41 years [35-46] and median disease duration of 14 years [10-19]. Concerning comorbidities, 34% of patients used anti-hypertensive drugs, 3% had diabetes/pre-diabetes, 5% dyslipidemia, 7% depression, 11% osteoporosis. Median BMI was 27.10 [23.87-31.30] kg/m2. Regarding SLE treatment, median prednisone dose was 0 [0-5] mg/day; 83% used hydroxychloroquine, 24% azathioprine, 41% mycophenolate mofetil, 8% methotrexate and 3% tacrolimus. Median SLEDAI score was 0 [0-2], SDI 0 [0-1], PGA 0 [0-1]. Concerning PROs: Median HAQ score was 0.25 [0.00-0.63], EQ5D score 0.67 [0.52-0.79], EQ5D VAS 70.00 [50.00-80.00], FACIT fatigue score (subscale additional concerns) 40.00 [30.00-46.25]. 61% of patients reported high adherence level. 15% of patients had high fatigue levels (FACIT fatigue< 27). FACIT Fatigue correlated with health quality score EQ5D (rho=0.660, p< 0.001), negatively with HAQ (rho=-0.682, p< 0.001) and BMI (rho=-0.210, p=0.022).
Conclusion: The observed discordance of low disease activity and SLEDAI with fatigue suggests that physicians may not be aware of the impact of fatigue in the quality of life of inactive or low disease activity lupus patients. PROs assessment may help to recognize and improve patient care.
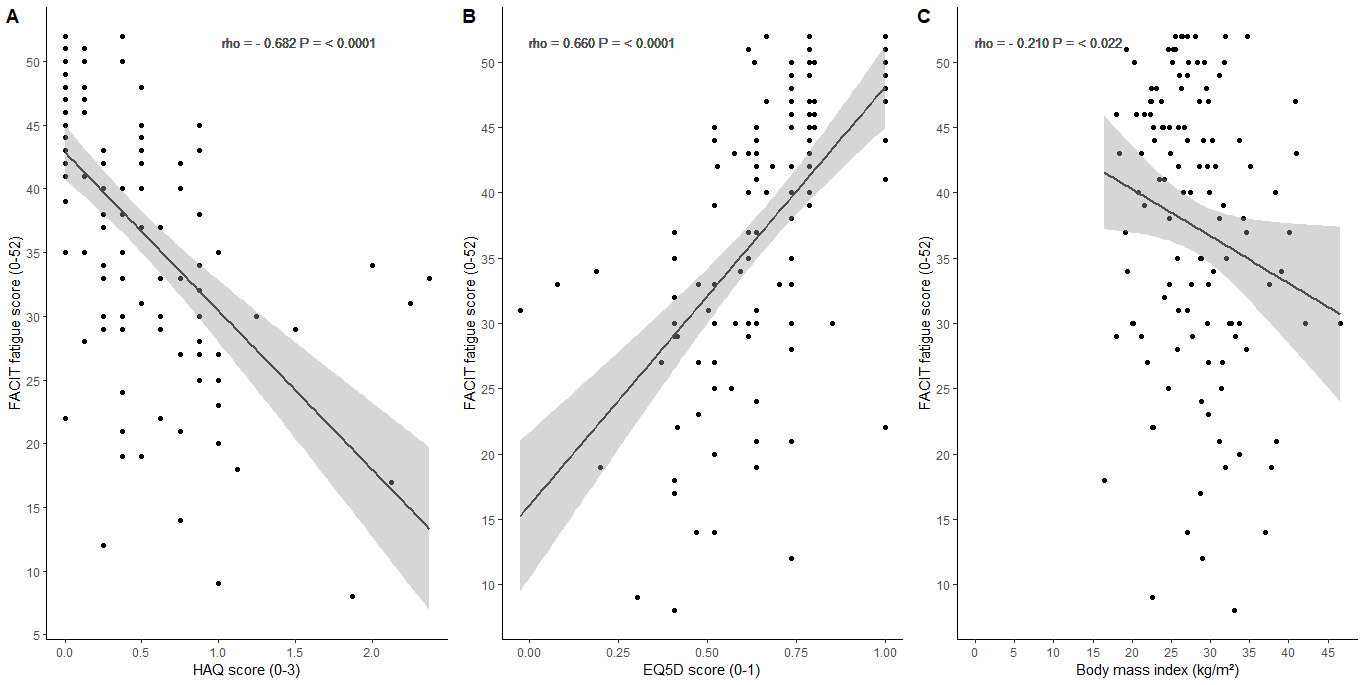 Figure 1 - Relation between FACIT fatigue score and HAQ, EQ5D and BMI, respectively.
Figure 1 - Relation between FACIT fatigue score and HAQ, EQ5D and BMI, respectively. Disclosures: R. De Moura Rodrigues, None; A. Moura dos Santos, None; D. Sampaio Cardoso, None; E. Figueiredo Neves Yuki, None; D. Castro Oliveira de Andrade, None; S. Gofinet Pasoto, None; E. Ferreira Borba Neto, None; E. Silva Dutra de Oliveira Bonfa, None; L. Seguro, None.

