Back
Poster Session A
Vasculitis
Session: (0458–0497) Vasculitis – Non-ANCA-Associated and Related Disorders Poster I: Giant Cell Arteritis
0479: A Prospective Study Evaluating the Utility of Ultrasound in Monitoring Newly-Diagnosed GCA
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- CK
Colm Kirby, MD
Tallaght University Hospital
DUBLIN, Dublin, Ireland
Abstract Poster Presenter(s)
Colm Kirby1, Rachael Flood1, Ronan Mullan1, Grainne Murphy2 and David Kane1, 1Tallaght University Hospital, Dublin, Ireland, 2Cork University Hospital, Cork, Ireland
Background/Purpose: In recent years, Temporal Artery US (TAUS) has become a reliable alternative to biopsy for diagnosing GCA. However, normalisation of pathologic findings have been described as early as 2 days to as late as 7 months after initiation of treatment. Additionally, use of anti-interleukin-6 therapies makes interpretation of ESR and CRP unreliable. Here, we evaluate to role of US in monitoring GCA disease activity.
Methods: We performed a prospective study of all newly diagnosed GCA patients (clinical diagnosis, verified by 2 rheumatologists after 6 months) who had a positive baseline vascular ultrasound (n= 57) presenting to our Rapid Access GCA clinic over 18 months. US of all 6 branches of the TAs and both axillary arteries was performed on all patients using a GE P9 device. Sonographic abnormalities considered indicative of vasculitis in the temporal arteries included the halo sign and non-compressible arteries with a thickened intima-media complex. In the axillary arteries, a halo sign and an intima-media thickness of >1.0mm was considered positive. To quantify the degree of vasculitis, we calculated a Halo Count (HC, number of branches with halo present) and Halo Score (HS, table 1) at each follow-up visit (1, 3, 6 ,12 months). We performed Independent and Paired Samples T-tests assess the utility of HC and HS in diagnosing and monitoring GCA.
Results: Our cohort consisted of 61% males (n=35) with a mean age of 74.4 years. Baseline HC, HS, CRP and interleukin-6 (but not ESR) correlated with physician-verified diagnosis at 6 months (p< 0.05 for all). Mean HC (Fig. 1) and HS (Fig. 2) for our cohort decreased at each study time-point (p< 0.005 for reductions between each time-point). Baseline HC and HS, but not ESR or CRP, correlated with future biologic requirement (n=19) (p< 0.05 for HC and HS).
Conclusion: Halo quantification using HC and HS can aid in diagnosing GCA with higher scores correlating with physician-verified diagnosis at 6 months. Additionally, our study shows that US may be useful in monitoring GCA disease activity and may replace conventional biomarkers for this purpose. Higher baseline HC and HS also identify which patients require future biologic therapy.
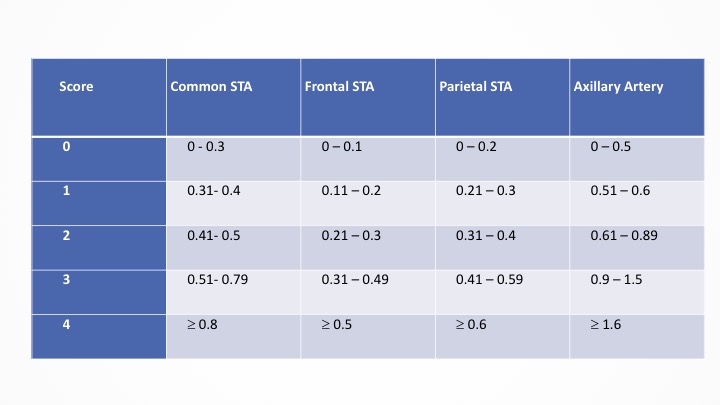 Table 1: Each arterial branch is assigned a score based on the maximal intima-media thickness (IMT) identified in that branch. IMT ranges (in millimetres) and their corresponding scores are outlined. Values for axillary arteries are multiplied by 3 to account for it having fewer branches. The scores are added to give a Total Halo Score, with a maximum value of 48. Halo scores are evaluated on serial scans to assess for wall-thickness regression. STA = Superficial Temporal Artery (5).
Table 1: Each arterial branch is assigned a score based on the maximal intima-media thickness (IMT) identified in that branch. IMT ranges (in millimetres) and their corresponding scores are outlined. Values for axillary arteries are multiplied by 3 to account for it having fewer branches. The scores are added to give a Total Halo Score, with a maximum value of 48. Halo scores are evaluated on serial scans to assess for wall-thickness regression. STA = Superficial Temporal Artery (5).
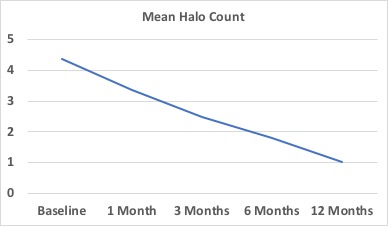 Figure 1: Mean Halo Counts decreased at each study time-point (1, 3, 6, 12 months) from baseline values in a cohort of 57 patients with GCA diagnosed on US.
Figure 1: Mean Halo Counts decreased at each study time-point (1, 3, 6, 12 months) from baseline values in a cohort of 57 patients with GCA diagnosed on US.
.jpg) Figure 2: Mean Halo Scores decreased at each study time-point (1, 3, 6, 12 months) from baseline values in a cohort of 57 patients with GCA diagnosed on US.
Figure 2: Mean Halo Scores decreased at each study time-point (1, 3, 6, 12 months) from baseline values in a cohort of 57 patients with GCA diagnosed on US.
Disclosures: C. Kirby, None; R. Flood, None; R. Mullan, None; G. Murphy, AbbVie/Abbott; D. Kane, AbbVie/Abbott.
Background/Purpose: In recent years, Temporal Artery US (TAUS) has become a reliable alternative to biopsy for diagnosing GCA. However, normalisation of pathologic findings have been described as early as 2 days to as late as 7 months after initiation of treatment. Additionally, use of anti-interleukin-6 therapies makes interpretation of ESR and CRP unreliable. Here, we evaluate to role of US in monitoring GCA disease activity.
Methods: We performed a prospective study of all newly diagnosed GCA patients (clinical diagnosis, verified by 2 rheumatologists after 6 months) who had a positive baseline vascular ultrasound (n= 57) presenting to our Rapid Access GCA clinic over 18 months. US of all 6 branches of the TAs and both axillary arteries was performed on all patients using a GE P9 device. Sonographic abnormalities considered indicative of vasculitis in the temporal arteries included the halo sign and non-compressible arteries with a thickened intima-media complex. In the axillary arteries, a halo sign and an intima-media thickness of >1.0mm was considered positive. To quantify the degree of vasculitis, we calculated a Halo Count (HC, number of branches with halo present) and Halo Score (HS, table 1) at each follow-up visit (1, 3, 6 ,12 months). We performed Independent and Paired Samples T-tests assess the utility of HC and HS in diagnosing and monitoring GCA.
Results: Our cohort consisted of 61% males (n=35) with a mean age of 74.4 years. Baseline HC, HS, CRP and interleukin-6 (but not ESR) correlated with physician-verified diagnosis at 6 months (p< 0.05 for all). Mean HC (Fig. 1) and HS (Fig. 2) for our cohort decreased at each study time-point (p< 0.005 for reductions between each time-point). Baseline HC and HS, but not ESR or CRP, correlated with future biologic requirement (n=19) (p< 0.05 for HC and HS).
Conclusion: Halo quantification using HC and HS can aid in diagnosing GCA with higher scores correlating with physician-verified diagnosis at 6 months. Additionally, our study shows that US may be useful in monitoring GCA disease activity and may replace conventional biomarkers for this purpose. Higher baseline HC and HS also identify which patients require future biologic therapy.
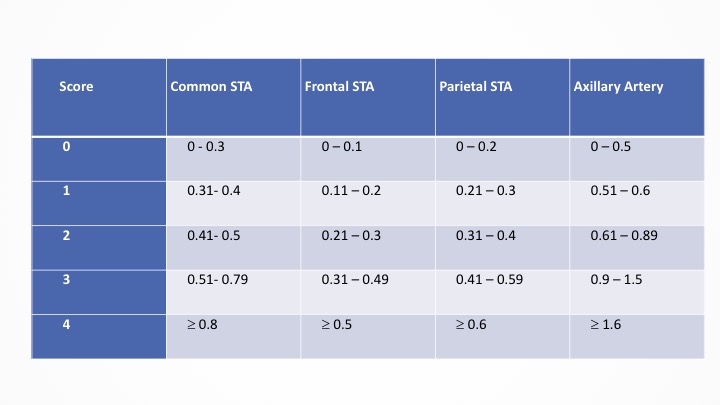 Table 1: Each arterial branch is assigned a score based on the maximal intima-media thickness (IMT) identified in that branch. IMT ranges (in millimetres) and their corresponding scores are outlined. Values for axillary arteries are multiplied by 3 to account for it having fewer branches. The scores are added to give a Total Halo Score, with a maximum value of 48. Halo scores are evaluated on serial scans to assess for wall-thickness regression. STA = Superficial Temporal Artery (5).
Table 1: Each arterial branch is assigned a score based on the maximal intima-media thickness (IMT) identified in that branch. IMT ranges (in millimetres) and their corresponding scores are outlined. Values for axillary arteries are multiplied by 3 to account for it having fewer branches. The scores are added to give a Total Halo Score, with a maximum value of 48. Halo scores are evaluated on serial scans to assess for wall-thickness regression. STA = Superficial Temporal Artery (5). 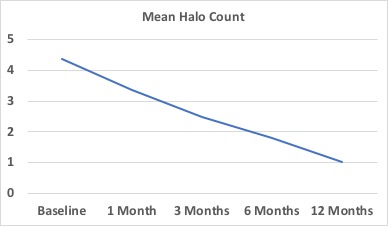 Figure 1: Mean Halo Counts decreased at each study time-point (1, 3, 6, 12 months) from baseline values in a cohort of 57 patients with GCA diagnosed on US.
Figure 1: Mean Halo Counts decreased at each study time-point (1, 3, 6, 12 months) from baseline values in a cohort of 57 patients with GCA diagnosed on US. .jpg) Figure 2: Mean Halo Scores decreased at each study time-point (1, 3, 6, 12 months) from baseline values in a cohort of 57 patients with GCA diagnosed on US.
Figure 2: Mean Halo Scores decreased at each study time-point (1, 3, 6, 12 months) from baseline values in a cohort of 57 patients with GCA diagnosed on US. Disclosures: C. Kirby, None; R. Flood, None; R. Mullan, None; G. Murphy, AbbVie/Abbott; D. Kane, AbbVie/Abbott.

