Back
Poster Session C
Epidemiology, health policy and outcomes
Session: (1267–1303) Measures and Measurement of Healthcare Quality Poster
1282: Practice Patterns for Pneumocystis Jiroveci Pneumonia (PJP) Prophylaxis Among Nephrologists and Rheumatologists – an International Survey Study
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- TB
Tanmayee Bichile, MD
Allegheny Health Network
Gibsonia, PA, United States
Abstract Poster Presenter(s)
Swati Arora1, Brad Rovin2 and Tanmayee Bichile3, 1Allegheny Health Network, Pittsburgh, 2The Ohio State University, Columbus, OH, 3Allegheny Health Network, Gibsonia, PA
Background/Purpose: Patients with autoimmune disorders such as systemic lupus erythematosus (SLE), lupus nephritis (LN) and granulomatosis with polyangiitis (GPA) frequently require treatment with immunosuppressive drugs. These patients are at higher risk of developing opportunistic infections with Pneumocystis jiroveci pneumonia (PJP) when exposed to long term glucocorticoids and cytotoxic medications. Often times, the care of these patients requires a multidisciplinary team where providers may have different approaches to management. The aim of this study is to compare similarities and differences in practice patterns of providers in nephrology and rheumatology with respect to PJP prophylaxis.
Methods: After appropriate IRB approval, we used Survey Monkey™ to survey nephrologists and rheumatologists. Surveys were sent via email to providers based in the USA and internationally. All responses were anonymous and voluntary.
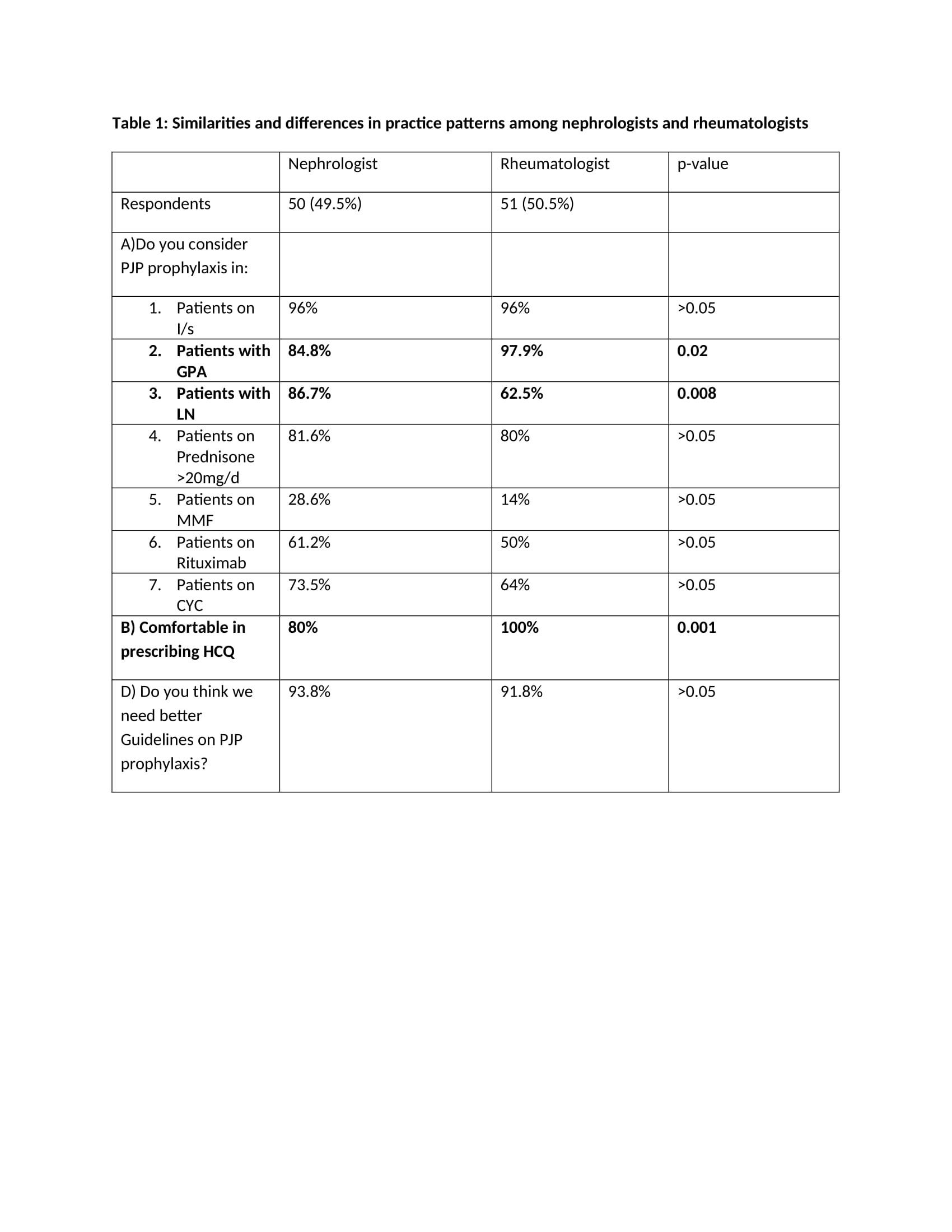
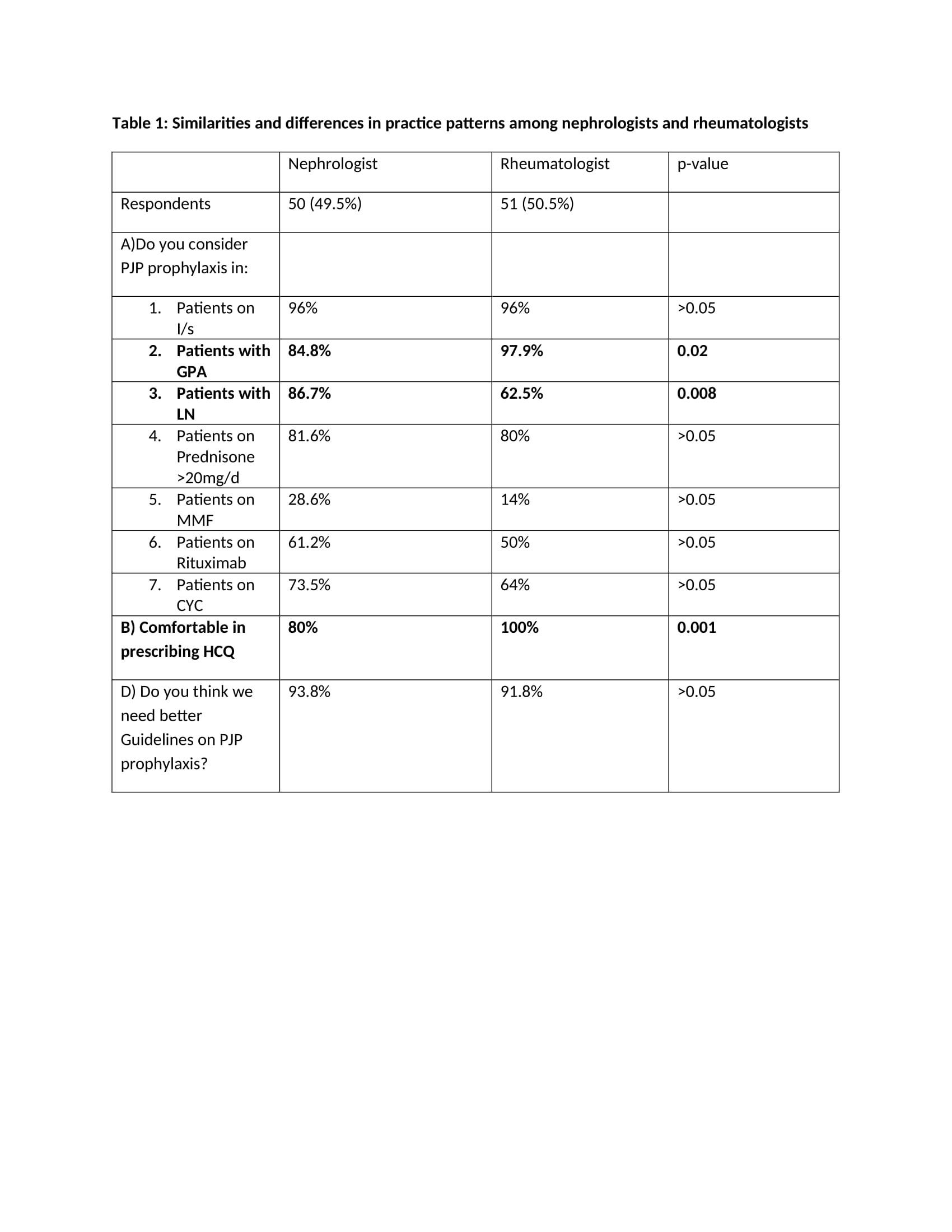
Results: We received 101 survey responses, 50.5% of respondents were rheumatologists and 49.5% were nephrologists. Females comprised 54.5% of the respondents. The majority of respondents, 69.3%, practiced at an academic institution while 21.8% were in private practice. Many providers (33.7%) had been in practice for over 20 years, while 17.8% had been in practice for less than 5 years. The majority of respondents were from North America (USA, Canada), but there were respondents from Europe, South America and Asia. Table 1 highlights the differences in response to survey questions between nephrologists and rheumatologists. With respect to PJP prophylaxis, there was no statistically significant difference in practice patterns among the two groups for patients on prednisone >20mg/d, mycophenolate mofetil (MMF), rituximab and cyclophosphamide (CYC). We did find a statistically significant (p< 0.05) difference in practice patterns among the two specialties with respect to consideration of PJP prophylaxis for patients with GPA (p value 0.02) and lupus nephritis (0.008) with rheumatologists favoring PJP prophylaxis in GPA and nephrologists in LN. There was also a statistically significant difference with comfort of prescribing hydroxychloroquine among these specialties (p value 0.001). Both groups were in favor of improved PJP prophylaxis guidelines.
Conclusion: Our survey study highlights the similarities and differences among nephrology and rheumatology providers with respect to PJP prophylaxis. There is unanimity among nephrologists and rheumatologists to use PJP prophylaxis among patients on immunosuppressive therapies such as prednisone >20mg/d, MMF, CYC, rituximab. However the uniformity of PJP prophylaxis was not observed for disease states like GPA and LN highlighting the need for further studies. There is consensus among nephrologists and rheumatologists for improved PJP prophylaxis guidelines.
Disclosures: S. Arora, Aurinia, GlaxoSmithKlein(GSK), Aurinia; B. Rovin, AstraZeneca, Aurinia, Biogen, Genetech, Janssen, Lupus Foundation of America, GlaxoSmithKlein(GSK); T. Bichile, None.
Background/Purpose: Patients with autoimmune disorders such as systemic lupus erythematosus (SLE), lupus nephritis (LN) and granulomatosis with polyangiitis (GPA) frequently require treatment with immunosuppressive drugs. These patients are at higher risk of developing opportunistic infections with Pneumocystis jiroveci pneumonia (PJP) when exposed to long term glucocorticoids and cytotoxic medications. Often times, the care of these patients requires a multidisciplinary team where providers may have different approaches to management. The aim of this study is to compare similarities and differences in practice patterns of providers in nephrology and rheumatology with respect to PJP prophylaxis.
Methods: After appropriate IRB approval, we used Survey Monkey™ to survey nephrologists and rheumatologists. Surveys were sent via email to providers based in the USA and internationally. All responses were anonymous and voluntary.
Results: We received 101 survey responses, 50.5% of respondents were rheumatologists and 49.5% were nephrologists. Females comprised 54.5% of the respondents. The majority of respondents, 69.3%, practiced at an academic institution while 21.8% were in private practice. Many providers (33.7%) had been in practice for over 20 years, while 17.8% had been in practice for less than 5 years. The majority of respondents were from North America (USA, Canada), but there were respondents from Europe, South America and Asia. Table 1 highlights the differences in response to survey questions between nephrologists and rheumatologists. With respect to PJP prophylaxis, there was no statistically significant difference in practice patterns among the two groups for patients on prednisone >20mg/d, mycophenolate mofetil (MMF), rituximab and cyclophosphamide (CYC). We did find a statistically significant (p< 0.05) difference in practice patterns among the two specialties with respect to consideration of PJP prophylaxis for patients with GPA (p value 0.02) and lupus nephritis (0.008) with rheumatologists favoring PJP prophylaxis in GPA and nephrologists in LN. There was also a statistically significant difference with comfort of prescribing hydroxychloroquine among these specialties (p value 0.001). Both groups were in favor of improved PJP prophylaxis guidelines.
Conclusion: Our survey study highlights the similarities and differences among nephrology and rheumatology providers with respect to PJP prophylaxis. There is unanimity among nephrologists and rheumatologists to use PJP prophylaxis among patients on immunosuppressive therapies such as prednisone >20mg/d, MMF, CYC, rituximab. However the uniformity of PJP prophylaxis was not observed for disease states like GPA and LN highlighting the need for further studies. There is consensus among nephrologists and rheumatologists for improved PJP prophylaxis guidelines.
Disclosures: S. Arora, Aurinia, GlaxoSmithKlein(GSK), Aurinia; B. Rovin, AstraZeneca, Aurinia, Biogen, Genetech, Janssen, Lupus Foundation of America, GlaxoSmithKlein(GSK); T. Bichile, None.

