Back
Poster Session C
Metabolic bone disease
Session: (1304–1331) Osteoporosis and Metabolic Bone Disease – Basic and Clinical Science Poster
1308: Prevalence and Therapeutic Practices of Osteoporosis in Sarcoidosis in the United States: A Nationwide Registry Study
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- DA
Diala Alawneh, MD
University of Illinois at Chicago
Chicago, IL, United States
Abstract Poster Presenter(s)
Diala Alawneh1, Moustafa Younis2, Romesa Hassan1, Bashar Alzghoul2, Shiva Arami1, Tricha Shivas3, Mary McGowan3, Khaldoon Alawneh4, Christian Ascoli1 and Nadera Sweiss1, 1University of Illinois at Chicago, Chicago, IL, 2University of Florida, Gainesville, FL, 3Foundation for Sarcoidosis Research, Chicago, IL, 4Jordan University of Science and Technology, Irbid, Jordan
Background/Purpose: Patients with sarcoidosis are at an increased risk of developing osteoporosis due to the active inflammatory state and chronic corticosteroid use. Proper dosing of vitamin D and calcium supplements is challenging given the risk of hypercalcemia. There is no consensus regarding the optimal strategies in management of osteoporosis in sarcoidosis patients. We sought to evaluate the prevalence, risk factors and therapeutic practices in patients with osteoporosis in the United States based on a national registry questionnaire.
Methods: We conducted a retrospective study based on a national registry investigating 3,835 respondents to the Foundation for Sarcoidosis Research - Sarcoidosis Advanced Registry for Cures Questionnaire (FSR-SARC). The registry includes patient surveys completed between June 2014 and August 2019. Summary and univariate analyses were performed.
Results: A total of 516 (13.5%) patients were identified to have osteoporosis. Among these, the mean age was 47 (± 13) years; 445 (86%) were female, 398 (77%) Caucasian and 96 (19%) African American. A diagnosis of osteoporosis was made after sarcoidosis diagnosis in 214/516 patients (42%). Patients with osteoporosis were significantly older than those without osteoporosis {47 (±13) vs 44 (±12); p< 0.0001}, however there was no significant difference in prevalence with regards to sex (p=0.333) Patients with osteoporosis had the following associated disorders: vitamin D deficiency (61%), Cushing's Syndrome (6%), hyperparathyroidism (0.6%), hypothyroidism (25%), hyperthyroidism (6%), low testosterone levels (10%), diabetes (21%), hypercalciuria (3%) and obesity (37%). Patients with osteoporosis had a significantly higher proportion of vitamin D deficiency compared to patients without (61% vs 33%, OR= 3.1, 95% CI 2.6-3.8; p< 0.0001). A total of 426 (97%) received the following therapies during the course of their disease: 396 (77%) steroids, 247 (67%) cytotoxic meds and 72 (24%) TNF inhibitor. Patients with osteoporosis were actively receiving treatment of their sarcoidosis with a variety of therapies as shown in Table 1. Patients with osteoporosis were more likely to have received systemic steroids (OR=2.8; 95% CI: 2.2-3.7; p< 0.0001), inhaled steroids (OR=1.6; 95% CI: 1.3-1.9; p< 0.0001), cytotoxic meds (OR= 1.54; 95% CI: 1.2-2.0; p< 0.0001) and TNF inhibitors (OR= 1.5; 95% CI: 1.2-2.0; p< 0.0001). A total of 124 (24%) received bisphosphonate therapy and 223 (43%) received vitamin D (D2, D3 or combined Ca-vitamin D) for treatment of osteoporosis.
Conclusion: A significant proportion of patients with sarcoidosis develop osteoporosis with no sex predilection, however older patients and Caucasian were more at risk. Concurrent vitamin D deficiency was significantly associated with osteoporosis in these patients. Patients with osteoporosis were more likely to be on systemic and/or inhaled steroids along with other immunosuppressants. Only a quarter of patients with osteoporosis received bisphosphonates.
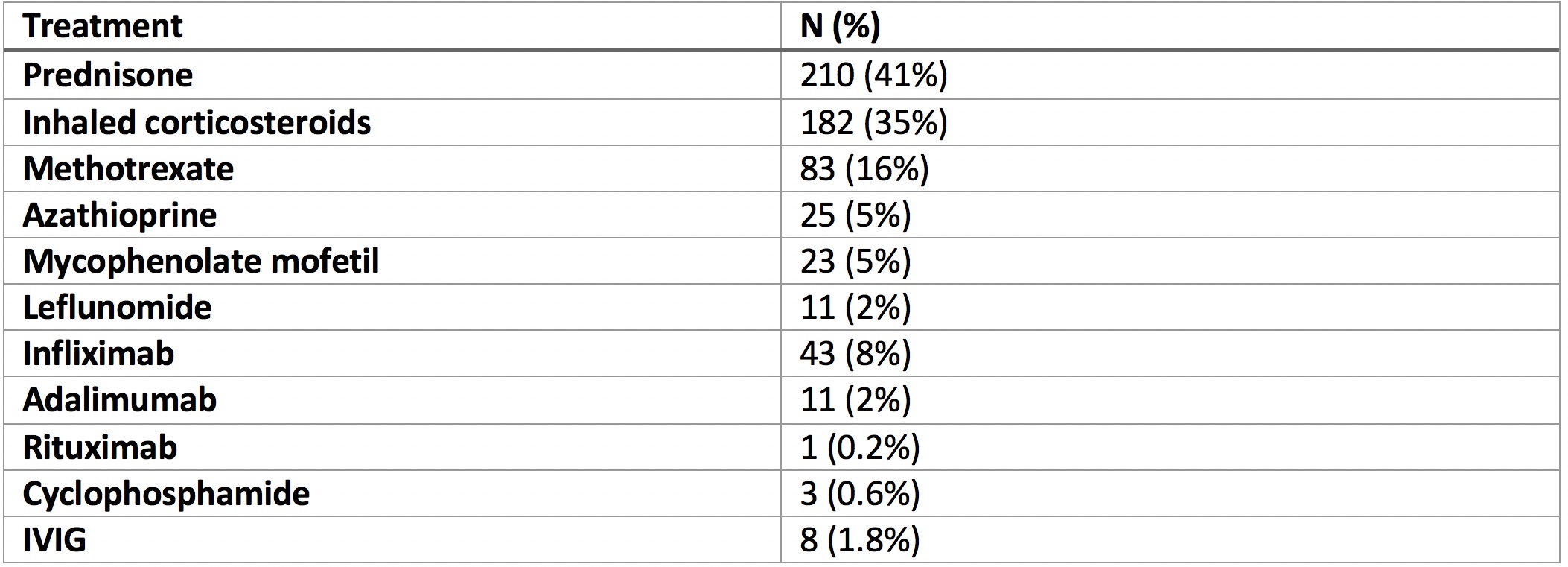 Table 1: Treatments patients with osteoporosis were actively receiving for sarcoidosis
Table 1: Treatments patients with osteoporosis were actively receiving for sarcoidosis
Disclosures: D. Alawneh, None; M. Younis, None; R. Hassan, None; B. Alzghoul, None; S. Arami, None; T. Shivas, None; M. McGowan, None; K. Alawneh, None; C. Ascoli, None; N. Sweiss, None.
Background/Purpose: Patients with sarcoidosis are at an increased risk of developing osteoporosis due to the active inflammatory state and chronic corticosteroid use. Proper dosing of vitamin D and calcium supplements is challenging given the risk of hypercalcemia. There is no consensus regarding the optimal strategies in management of osteoporosis in sarcoidosis patients. We sought to evaluate the prevalence, risk factors and therapeutic practices in patients with osteoporosis in the United States based on a national registry questionnaire.
Methods: We conducted a retrospective study based on a national registry investigating 3,835 respondents to the Foundation for Sarcoidosis Research - Sarcoidosis Advanced Registry for Cures Questionnaire (FSR-SARC). The registry includes patient surveys completed between June 2014 and August 2019. Summary and univariate analyses were performed.
Results: A total of 516 (13.5%) patients were identified to have osteoporosis. Among these, the mean age was 47 (± 13) years; 445 (86%) were female, 398 (77%) Caucasian and 96 (19%) African American. A diagnosis of osteoporosis was made after sarcoidosis diagnosis in 214/516 patients (42%). Patients with osteoporosis were significantly older than those without osteoporosis {47 (±13) vs 44 (±12); p< 0.0001}, however there was no significant difference in prevalence with regards to sex (p=0.333) Patients with osteoporosis had the following associated disorders: vitamin D deficiency (61%), Cushing's Syndrome (6%), hyperparathyroidism (0.6%), hypothyroidism (25%), hyperthyroidism (6%), low testosterone levels (10%), diabetes (21%), hypercalciuria (3%) and obesity (37%). Patients with osteoporosis had a significantly higher proportion of vitamin D deficiency compared to patients without (61% vs 33%, OR= 3.1, 95% CI 2.6-3.8; p< 0.0001). A total of 426 (97%) received the following therapies during the course of their disease: 396 (77%) steroids, 247 (67%) cytotoxic meds and 72 (24%) TNF inhibitor. Patients with osteoporosis were actively receiving treatment of their sarcoidosis with a variety of therapies as shown in Table 1. Patients with osteoporosis were more likely to have received systemic steroids (OR=2.8; 95% CI: 2.2-3.7; p< 0.0001), inhaled steroids (OR=1.6; 95% CI: 1.3-1.9; p< 0.0001), cytotoxic meds (OR= 1.54; 95% CI: 1.2-2.0; p< 0.0001) and TNF inhibitors (OR= 1.5; 95% CI: 1.2-2.0; p< 0.0001). A total of 124 (24%) received bisphosphonate therapy and 223 (43%) received vitamin D (D2, D3 or combined Ca-vitamin D) for treatment of osteoporosis.
Conclusion: A significant proportion of patients with sarcoidosis develop osteoporosis with no sex predilection, however older patients and Caucasian were more at risk. Concurrent vitamin D deficiency was significantly associated with osteoporosis in these patients. Patients with osteoporosis were more likely to be on systemic and/or inhaled steroids along with other immunosuppressants. Only a quarter of patients with osteoporosis received bisphosphonates.
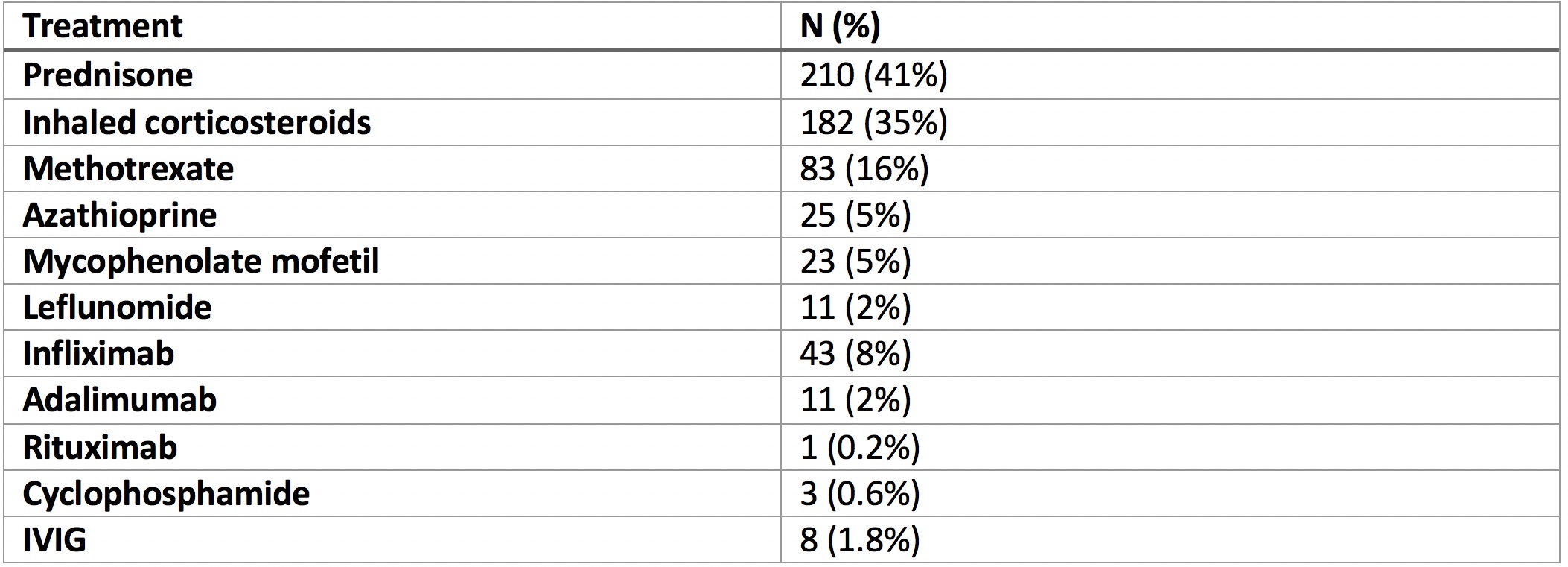 Table 1: Treatments patients with osteoporosis were actively receiving for sarcoidosis
Table 1: Treatments patients with osteoporosis were actively receiving for sarcoidosisDisclosures: D. Alawneh, None; M. Younis, None; R. Hassan, None; B. Alzghoul, None; S. Arami, None; T. Shivas, None; M. McGowan, None; K. Alawneh, None; C. Ascoli, None; N. Sweiss, None.

