Back
Poster Session C
Imaging
Session: (1228–1266) Imaging of Rheumatic Diseases Poster
1255: Rheumatologists Overcall Sacroiliitis on X-ray and MRI in Axial Spondyloarthritis Patients: Data from the BelGian Inflammatory Arthritis and SpoNdylitis cohorT (Be-GIANT)
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- AD
Ann-Sophie De Craemer, MD
Ghent University Hospital
Gent, Belgium
Abstract Poster Presenter(s)
Ann-Sophie Kathleen De Craemer1, Manouk de Hooge2, Thomas Renson3, Liselotte Deroo4, Gaelle Varkas3, Liesbet Van Praet5, Rik Joos6, Jan Lenaerts7, Mieke Devinck8, Lieve Gyselbrecht9, isabelle peene3, Kristof Thevissen10, Philippe Carron3, Filip Van den bosch11 and Dirk Elewaut12, 1Ghent University Hospital, Gent, Belgium, 2Ghent University Hospital, Luxembourg, Luxembourg, 3Ghent University Hospital, Ghent, Belgium, 4Ghent University, Gent, Belgium, 5AZ Maria Middelares, Ghent, Belgium, 6Ghent University Hospital, Basel, Switzerland, 7Reuma Instituut Hasselt, Hasselt, Belgium, 8AZ Sint-Lucas, Brugge, Belgium, 9ASZ Aalst, Aalst, Belgium, 10Reumacentrum Genk, Genk, Belgium, 11Department of Internal Medicine and Paediatrics, Ghent University and VIB Centre for Inflammation Research, Ghent, Belgium, 12Department of Rheumatology, Ghent University Hospital, Belgium, VIB-UGent Center for Inflammation Research, Ghent University, Heusden, Belgium
Background/Purpose: To investigate (1) agreement between local and central reading of sacroiliac joint images (X-ray and magnetic resonance imaging [MRI]) from axial spondylarthritis (axSpA) patients, and (2) to explore potential differences between patients diagnosed in an academic hospital compared to community centres.
Methods: The BelGian Inflammatory Arthritis and spoNdylitis cohort (Be-GIANT) includes newly diagnosed biological-naïve axSpA patients, that fulfil the ASAS classification criteria, at the outpatient clinic of an academic hospital and eight community centres in Flanders. X-ray and MRI of the sacroiliac joints (SIJ) of patients enrolled between November 2010 and August 2020 were assessed by the local rheumatologist ('local reading') and two calibrated central readers ('central reading') for definite radiographic sacroiliitis according to the modified New York criteria (X-SIJ) and active sacroiliitis according to the ASAS/OMERACT definition of a positive MRI (MRI-SIJ). Central readers resolved discrepant cases by consensus. Inter-reader reliability was assessed with Cohen's Kappa, and % overall, positive and negative agreement.
Results: Among the 271 included patients (n=205 academic hospital, n=66 community hospital), 231 X-SIJ and 208 MRI-SIJ were available for central reading (Table 1). Central readers disagreed with local readers on 30/231 (13%) X-SIJ images (κ=0.44, moderate); 4/231 (1.7%) were reclassified as radiographic sacroiliitis and 26/231 (11.3%) as not showing radiographic sacroiliitis. Overall agreement was higher between central readers and academic rheumatologists compared to community rheumatologists (90.5% vs. 70.7%, p< 0.001). 53/208 (25.4%) MRI-SIJ images were reclassified by central readers (κ=0.36, fair); the majority as negative for active sacroiliitis (51/208, 24.5%). Central readers agreed on the assessment of MRI-SIJ in a higher proportion with academic rheumatologists versus community rheumatologists (77.2% vs. 63.4%, p=0.07).
Conclusion: In newly diagnosed axSpA patients, the prevalence of radiographic sacroiliitis is low. Sacroiliitis on MRI is overcalled by rheumatologists both in academic and non-academic settings, leaving opportunities for educational interventions.
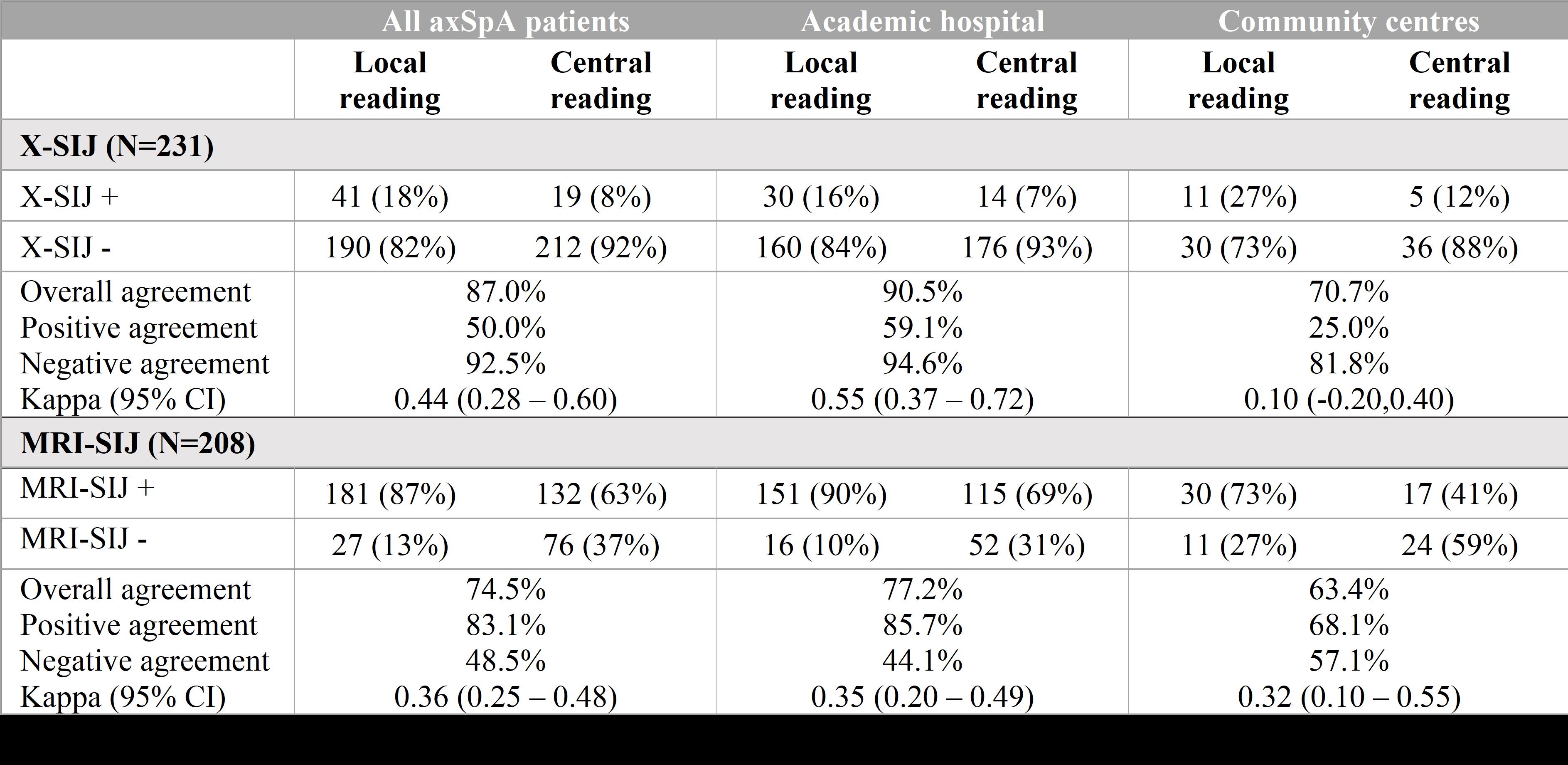 Table 1: Agreement between local and central readers on X-SIJ and MRI-SIJ of axSpA patients in academic and community centers.
Table 1: Agreement between local and central readers on X-SIJ and MRI-SIJ of axSpA patients in academic and community centers.
Disclosures: A. De Craemer, None; M. de Hooge, None; T. Renson, None; L. Deroo, None; G. Varkas, None; L. Van Praet, None; R. Joos, None; J. Lenaerts, None; M. Devinck, None; L. Gyselbrecht, None; i. peene, None; K. Thevissen, None; P. Carron, Biogen, AbbVie/Abbott, Eli Lilly, Fresenius Kabi, Galapagos, Merck/MSD, Pfizer, Sanofi, UCB; F. Van den bosch, AbbVie, Lilly, Galapagos, Janssen, Merck, Novartis, Pfizer, UCB, Amgen, Bristol-Myers Squibb(BMS), Celgene; D. Elewaut, AbbVie, Eli Lilly, Galapagos, Novartis, UCB Pharma.
Background/Purpose: To investigate (1) agreement between local and central reading of sacroiliac joint images (X-ray and magnetic resonance imaging [MRI]) from axial spondylarthritis (axSpA) patients, and (2) to explore potential differences between patients diagnosed in an academic hospital compared to community centres.
Methods: The BelGian Inflammatory Arthritis and spoNdylitis cohort (Be-GIANT) includes newly diagnosed biological-naïve axSpA patients, that fulfil the ASAS classification criteria, at the outpatient clinic of an academic hospital and eight community centres in Flanders. X-ray and MRI of the sacroiliac joints (SIJ) of patients enrolled between November 2010 and August 2020 were assessed by the local rheumatologist ('local reading') and two calibrated central readers ('central reading') for definite radiographic sacroiliitis according to the modified New York criteria (X-SIJ) and active sacroiliitis according to the ASAS/OMERACT definition of a positive MRI (MRI-SIJ). Central readers resolved discrepant cases by consensus. Inter-reader reliability was assessed with Cohen's Kappa, and % overall, positive and negative agreement.
Results: Among the 271 included patients (n=205 academic hospital, n=66 community hospital), 231 X-SIJ and 208 MRI-SIJ were available for central reading (Table 1). Central readers disagreed with local readers on 30/231 (13%) X-SIJ images (κ=0.44, moderate); 4/231 (1.7%) were reclassified as radiographic sacroiliitis and 26/231 (11.3%) as not showing radiographic sacroiliitis. Overall agreement was higher between central readers and academic rheumatologists compared to community rheumatologists (90.5% vs. 70.7%, p< 0.001). 53/208 (25.4%) MRI-SIJ images were reclassified by central readers (κ=0.36, fair); the majority as negative for active sacroiliitis (51/208, 24.5%). Central readers agreed on the assessment of MRI-SIJ in a higher proportion with academic rheumatologists versus community rheumatologists (77.2% vs. 63.4%, p=0.07).
Conclusion: In newly diagnosed axSpA patients, the prevalence of radiographic sacroiliitis is low. Sacroiliitis on MRI is overcalled by rheumatologists both in academic and non-academic settings, leaving opportunities for educational interventions.
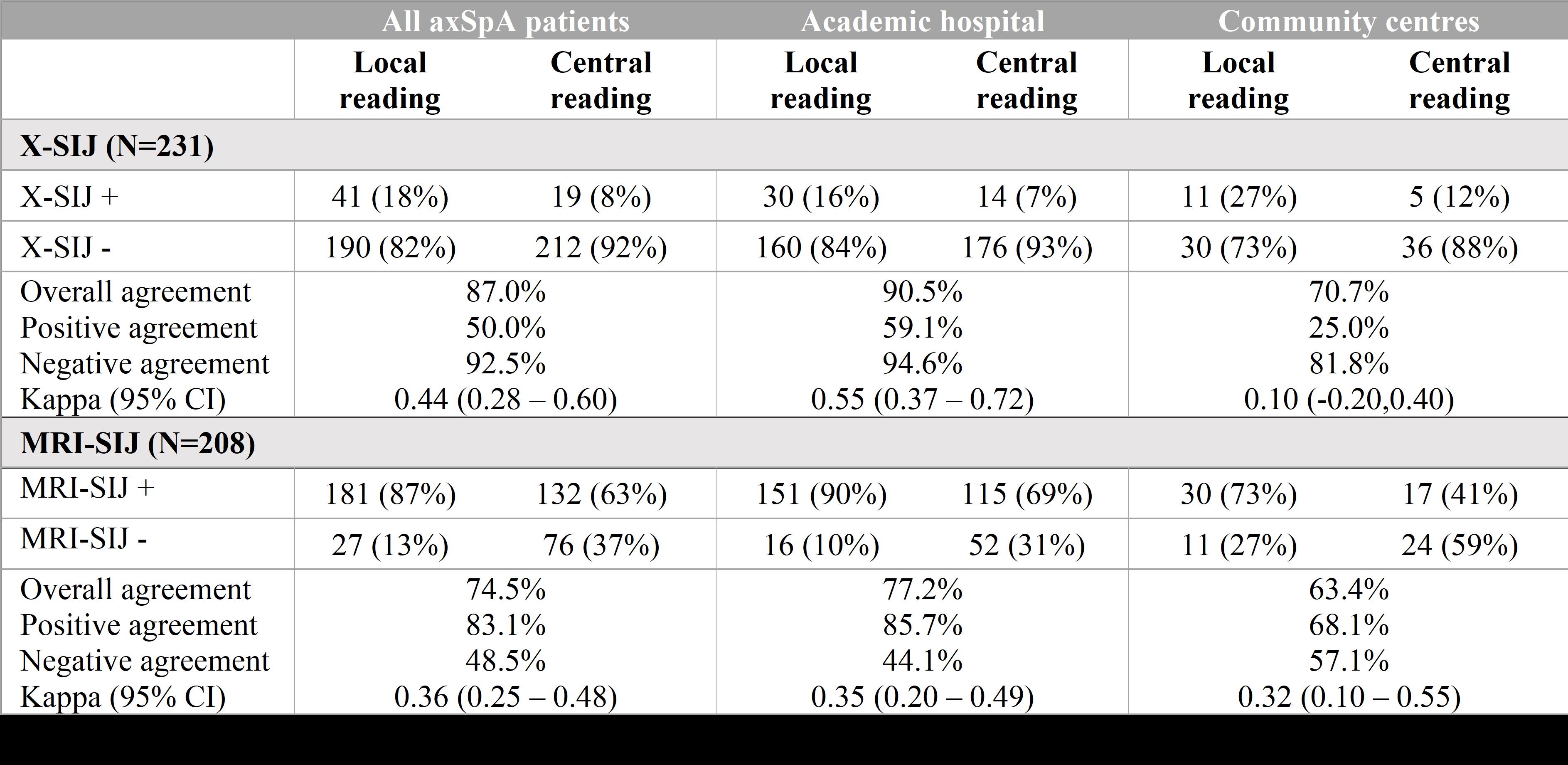 Table 1: Agreement between local and central readers on X-SIJ and MRI-SIJ of axSpA patients in academic and community centers.
Table 1: Agreement between local and central readers on X-SIJ and MRI-SIJ of axSpA patients in academic and community centers. Disclosures: A. De Craemer, None; M. de Hooge, None; T. Renson, None; L. Deroo, None; G. Varkas, None; L. Van Praet, None; R. Joos, None; J. Lenaerts, None; M. Devinck, None; L. Gyselbrecht, None; i. peene, None; K. Thevissen, None; P. Carron, Biogen, AbbVie/Abbott, Eli Lilly, Fresenius Kabi, Galapagos, Merck/MSD, Pfizer, Sanofi, UCB; F. Van den bosch, AbbVie, Lilly, Galapagos, Janssen, Merck, Novartis, Pfizer, UCB, Amgen, Bristol-Myers Squibb(BMS), Celgene; D. Elewaut, AbbVie, Eli Lilly, Galapagos, Novartis, UCB Pharma.

