Back
Poster Session C
Epidemiology, health policy and outcomes
Session: (1267–1303) Measures and Measurement of Healthcare Quality Poster
1295: Targeting Barriers That Prevent Contraception Counseling in an Academic Rheumatology Practice
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- TS
Tara Skorupa, MD
Beth Israel Deaconess Medical Center
Boston, MA, United States
Abstract Poster Presenter(s)
Tara Skorupa1, Kristin Sturm2, Aaron Lazorwitz2, Guiset Carvajal Bedoya3, Ju Young Kwag2, JoAnn Zell2 and Kristen Demoruelle2, 1University of Colorado, Aurora, CO, 2University of Colorado Anschutz Medical Campus, Aurora, CO, 3Billings Clinic, Billings, MT
Background/Purpose: Systemic autoimmune diseases disproportionately affect females of childbearing potential. Many of the medications used to treat systemic autoimmune diseases have suspected or confirmed teratogenic effects. As such, contraception counseling to prevent unplanned pregnancy is a cornerstone for optimal rheumatology clinical care. Yet, studies report inadequate rates of contraception counseling by rheumatology providers. In this study, we evaluated provider-reported barriers to contraception counseling as well as the effectiveness of several clinical interventions initiated to improve contraception counseling.
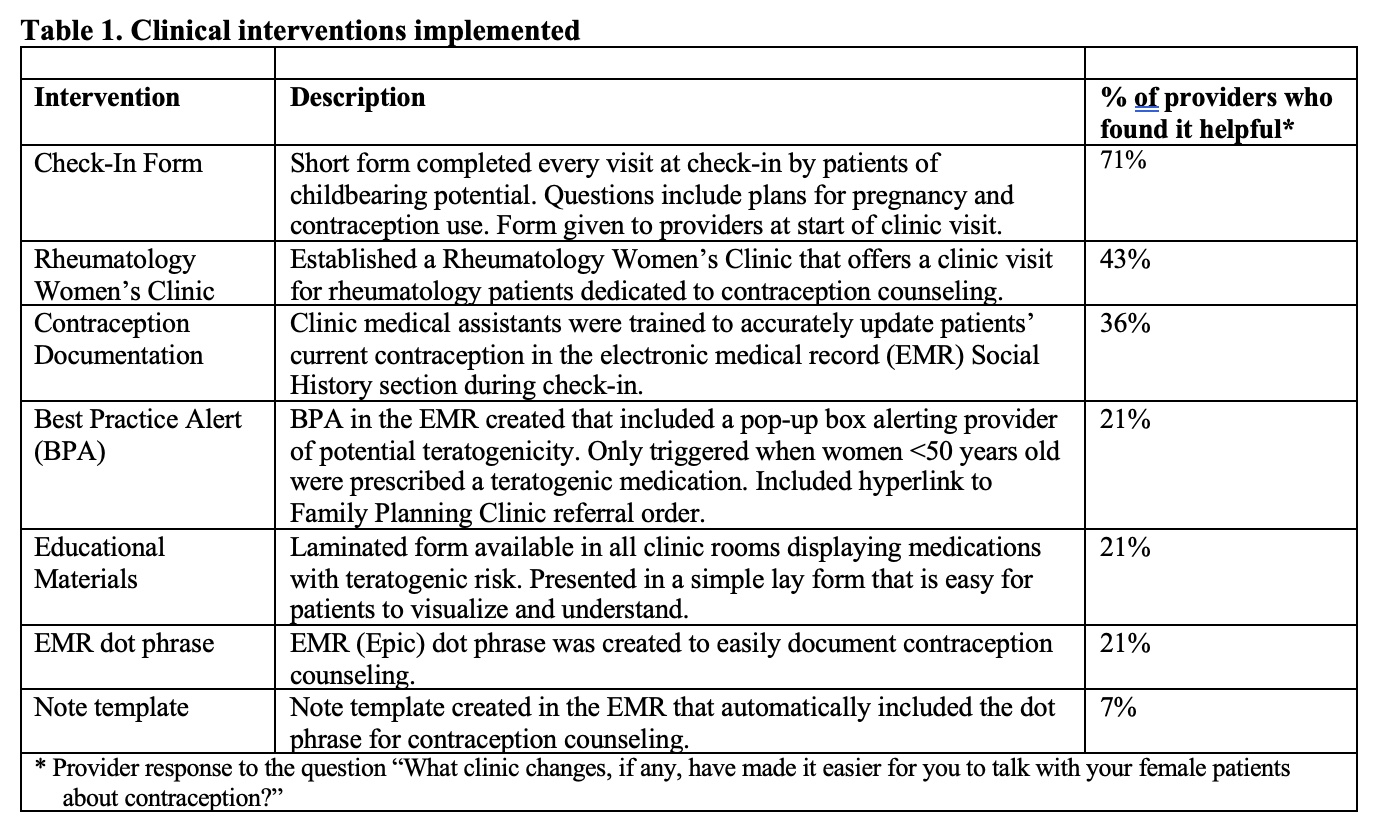
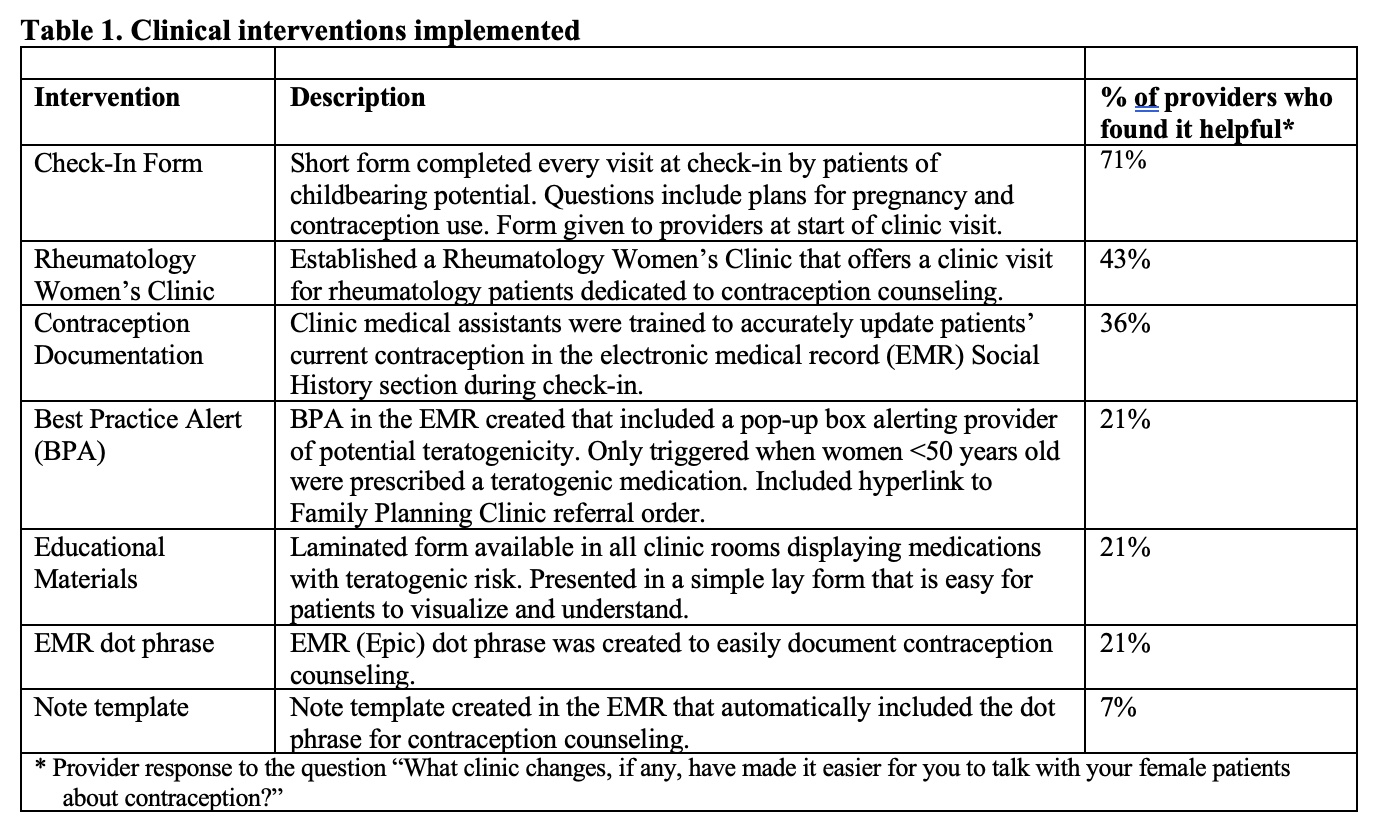
Methods: We administered an anonymous online questionnaire to outpatient rheumatology clinical providers at an academic clinical practice (N=14) asking, "What barriers do you encounter that make it difficult to talk with your female patients about contraception?". In April 2021, we initiated six clinical interventions designed to improve feasibility and effectiveness of contraception counseling (see Table 1). A follow-up questionnaire was completed by providers 11 months after these clinical interventions. We also quantified the number of clinical referrals ordered by rheumatology providers to our affiliated Family Planning clinic, which provides contraception counseling and administers contraception for medically complicated patients.
Results: The frequency of provider-reported contraception counseling increased between pre- and post-intervention surveys, and there was an increase in provider comfort level asking patients about contraception use (Table 2). Providers reporting they were 'comfortable' or 'very comfortable' asking female patients about their contraception use increased from 79% to 100%. The intervention perceived by providers to be the most beneficial was the Check-in Form followed by the option for a Rheumatology Women's Clinic visit (Table 1). There was a significant change in referral patterns to the Family Planning clinic. Specifically, in the two years prior to our clinical interventions (04/2019-03/2021), the total number of Family Planning clinic referrals was 9 (0.4/month), and in the 12 months after the clinical intervention (04/2021-03/2022), the number of referrals increased to 35 (2.9/month, p=0.02). Despite these interventions, barriers still exist, with the most prevalent barriers identified by providers being time constraints and patient acuity (Table 2).
Conclusion: We identified several clinical interventions that rheumatology providers found helpful to improve their comfort level when talking to female patients about contraception, particularly a quick and simple Check-In Form given to patients of childbearing potential. Our interventions increased referrals to a Family Planning clinic by a remarkable 725%. However, future studies are needed to evaluate whether the increased referral pattern resulted in increased use of effective contraception by rheumatology patients. Despite some of the positive changes we identified with our clinical interventions, barriers remain for rheumatology providers to provide effective contraception counseling to their patients.
.jpg)
Disclosures: T. Skorupa, None; K. Sturm, None; A. Lazorwitz, None; G. Carvajal Bedoya, None; J. Kwag, None; J. Zell, None; K. Demoruelle, Boehringer-Ingelheim, Pfizer.
Background/Purpose: Systemic autoimmune diseases disproportionately affect females of childbearing potential. Many of the medications used to treat systemic autoimmune diseases have suspected or confirmed teratogenic effects. As such, contraception counseling to prevent unplanned pregnancy is a cornerstone for optimal rheumatology clinical care. Yet, studies report inadequate rates of contraception counseling by rheumatology providers. In this study, we evaluated provider-reported barriers to contraception counseling as well as the effectiveness of several clinical interventions initiated to improve contraception counseling.
Methods: We administered an anonymous online questionnaire to outpatient rheumatology clinical providers at an academic clinical practice (N=14) asking, "What barriers do you encounter that make it difficult to talk with your female patients about contraception?". In April 2021, we initiated six clinical interventions designed to improve feasibility and effectiveness of contraception counseling (see Table 1). A follow-up questionnaire was completed by providers 11 months after these clinical interventions. We also quantified the number of clinical referrals ordered by rheumatology providers to our affiliated Family Planning clinic, which provides contraception counseling and administers contraception for medically complicated patients.
Results: The frequency of provider-reported contraception counseling increased between pre- and post-intervention surveys, and there was an increase in provider comfort level asking patients about contraception use (Table 2). Providers reporting they were 'comfortable' or 'very comfortable' asking female patients about their contraception use increased from 79% to 100%. The intervention perceived by providers to be the most beneficial was the Check-in Form followed by the option for a Rheumatology Women's Clinic visit (Table 1). There was a significant change in referral patterns to the Family Planning clinic. Specifically, in the two years prior to our clinical interventions (04/2019-03/2021), the total number of Family Planning clinic referrals was 9 (0.4/month), and in the 12 months after the clinical intervention (04/2021-03/2022), the number of referrals increased to 35 (2.9/month, p=0.02). Despite these interventions, barriers still exist, with the most prevalent barriers identified by providers being time constraints and patient acuity (Table 2).
Conclusion: We identified several clinical interventions that rheumatology providers found helpful to improve their comfort level when talking to female patients about contraception, particularly a quick and simple Check-In Form given to patients of childbearing potential. Our interventions increased referrals to a Family Planning clinic by a remarkable 725%. However, future studies are needed to evaluate whether the increased referral pattern resulted in increased use of effective contraception by rheumatology patients. Despite some of the positive changes we identified with our clinical interventions, barriers remain for rheumatology providers to provide effective contraception counseling to their patients.
.jpg)
Disclosures: T. Skorupa, None; K. Sturm, None; A. Lazorwitz, None; G. Carvajal Bedoya, None; J. Kwag, None; J. Zell, None; K. Demoruelle, Boehringer-Ingelheim, Pfizer.

