Back
Poster Session C
Fibrosing rheumatic diseases (scleroderma, MCTD, IgG4-related disease, scleroderma mimics)
Session: (1166–1185) Systemic Sclerosis and Related Disorders – Basic Science Poster
1167: Towards an Autologous 3D Skin-like Tissue Harboring Patient-Derived Fibroblasts, Keratinocytes, T-cells and Macrophages
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- SS
Sasha Shenk, BS
Tufts University
Boston, MA, United States
Abstract Poster Presenter(s)
Sasha Shenk1, Jonathan Garlick1, Lev Brown2, Jamie Riesenberg2, Christian Evans2, Julia Jaffe Zweifach2, Andrew Macklin2, Tamar Abel3, Noelle Kosarek4, Mengqi Huang5, Avi Smith1, Tammara Wood3, Gretel Torres6, Patricia pioli6 and Michael Whitfield7, 1Tufts University School of Dental Medicine, Boston, MA, 2Tufts University, Boston, MA, 3Dartmouth College, Hanover, NH, 4Dartmouth Geisel School of Medicine, Lebanon, NH, 5University of Pittsburgh, Pittsburgh, PN, 6Geisel School of Medicine at Dartmouth, Lebanon, NH, 7Dartmouth Geisel School of Medicine, Department of Biomedical Data Science, Lebanon, NH
Background/Purpose: Scleroderma (Systemic Sclerosis; SSc) is an autoimmune disease of unknown etiology that is characterized by vascular dysfunction, fibrosis, and inflammation. A lack of human autologous SSc disease models has created an unmet need for preclinical drug screening tissue models that can predict the success or failure of drugs designed to treat SSc. Recent advances in our lab have resulted in 3D skin-like tissue-based disease models that incorporate SSc patient-derived macrophages and fibroblasts. We now seek to develop 3D skin-like tissue models that additionally incorporate SSc patient-derived keratinocytes and T cells. We hope to more accurately recapitulate SSc patient subtypes that will be an important advancement over currently available 3D tissues.
Methods: Skin keratinocytes isolated from SSc and control patients that were tested using Colony Forming Efficiency (CFE) assays to determine their growth potential. CD4+ T cells were isolated from peripheral blood mononuclear cells (PBMCs) by magnetic bead isolation and tested for homogeneity using flow cytometry. 3D skin-like tissues (HSE= human skin equivalent) were constructed by seeding fibroblasts, keratinocytes and macrophages into a bovine collagen gel and grown at an air-liquid interface for 2 weeks. SSc-T-cells were then seeded onto a second tissue insert and HSEs were layered onto them. 3D skin-like tissues (Fig. 1) were constructed with varying combinations of SSc patient-derived cells that included: (1) fibroblasts; (2) keratinocytes with optimal proliferative potential, (3) CD4+ T cells and (4) macrophages. This created a 3D tissue that combined all four cell types from the same SSc patient to create a fully autologous, patient-specific 3D skin-like model of SSc.
Results: Morphologic analysis of the 3D tissue model showed that T-cells migrated into the tissue and remained viable as indicated by elevated levels of IL-6 only when T cells were present in the tissues (Fig. 1, D). CFE assays found that two SSc patient-derived keratinocyte strains (SF-15.2 and SF14.2) showed high CFEs of 11% and 18% that were sufficient for 3D tissue fabrication. When SSc patient-matched keratinocytes and fibroblasts were used to fabricate HSEs, these autologous tissues developed a more well-differentiated epithelium than in tissues with cells that were not autologous (Fig 2). We established that 3D tissues can incorporate 4 SSc-derived cell types that can recapitulate the cellular heterogeneity seen in SSc in vivo.
Conclusion: We have determined that that (1) fully autologous 3D skin-like tissues can be constructed with 4 different SSc patient-derived cell types, (2) SSc-derived tissues containing these multiple cells from the same person with SSc (autologous tissues) result in improved tissue morphology and phenotype when compared to tissues constructed with cells from different SSc patient skins, (3) these multiple cell types contribute to intercellular cross-talk needed to optimize skin tissue architecture to study SSc. These autologous 3D tissues will streamline screening of promising candidate drugs designed to improve treatment of SSc so they can safely and efficiently enter human clinical trials.
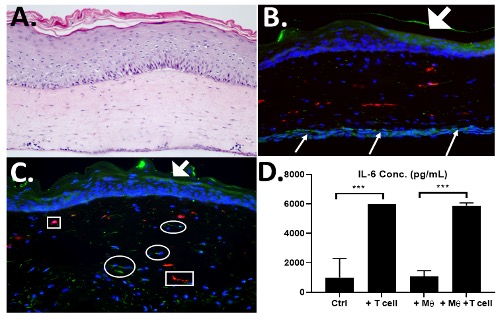 Figure 1. T cells in skin equivalents are functional- A) H&E image of 3D skin containing patient-derived fibroblasts, Macrophages and T cells. B) IHC staining for CD206-Macrophages (red) CD4-T cells (green) on bottom of tissue that migrated into dermis in 4 days (C). T cell function was shown by elevation of IL-6 secretion in T cell-containing tissues when compared to control or macrophage-only containing tissues (D).
Figure 1. T cells in skin equivalents are functional- A) H&E image of 3D skin containing patient-derived fibroblasts, Macrophages and T cells. B) IHC staining for CD206-Macrophages (red) CD4-T cells (green) on bottom of tissue that migrated into dermis in 4 days (C). T cell function was shown by elevation of IL-6 secretion in T cell-containing tissues when compared to control or macrophage-only containing tissues (D).
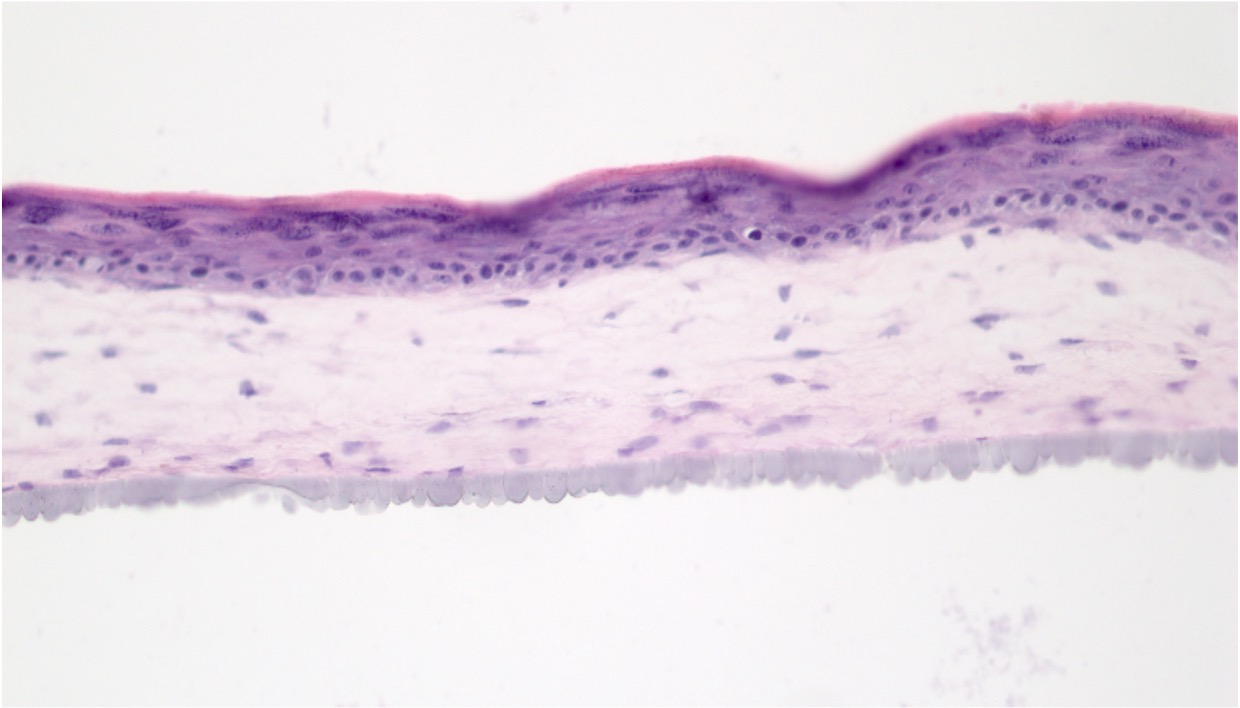 Figure 2. Fabrication of fully autologous human tissues with SSc cells- HSE skin-like tissues were constructed with patient-matched, SSc-derived keratinocytes (SK15.2) and fibroblasts (SF15.2). Tissues were grown for 2 weeks revealing well-differentiated epithelium and well-structured dermis.
Figure 2. Fabrication of fully autologous human tissues with SSc cells- HSE skin-like tissues were constructed with patient-matched, SSc-derived keratinocytes (SK15.2) and fibroblasts (SF15.2). Tissues were grown for 2 weeks revealing well-differentiated epithelium and well-structured dermis.
Disclosures: S. Shenk, None; J. Garlick, None; L. Brown, None; J. Riesenberg, None; C. Evans, None; J. Jaffe Zweifach, None; A. Macklin, None; T. Abel, None; N. Kosarek, None; M. Huang, None; A. Smith, None; T. Wood, None; G. Torres, None; P. pioli, None; M. Whitfield, Corbus Pharmaceuticals, Celdara Medical LLC, Bristol-Myers Squibb(BMS).
Background/Purpose: Scleroderma (Systemic Sclerosis; SSc) is an autoimmune disease of unknown etiology that is characterized by vascular dysfunction, fibrosis, and inflammation. A lack of human autologous SSc disease models has created an unmet need for preclinical drug screening tissue models that can predict the success or failure of drugs designed to treat SSc. Recent advances in our lab have resulted in 3D skin-like tissue-based disease models that incorporate SSc patient-derived macrophages and fibroblasts. We now seek to develop 3D skin-like tissue models that additionally incorporate SSc patient-derived keratinocytes and T cells. We hope to more accurately recapitulate SSc patient subtypes that will be an important advancement over currently available 3D tissues.
Methods: Skin keratinocytes isolated from SSc and control patients that were tested using Colony Forming Efficiency (CFE) assays to determine their growth potential. CD4+ T cells were isolated from peripheral blood mononuclear cells (PBMCs) by magnetic bead isolation and tested for homogeneity using flow cytometry. 3D skin-like tissues (HSE= human skin equivalent) were constructed by seeding fibroblasts, keratinocytes and macrophages into a bovine collagen gel and grown at an air-liquid interface for 2 weeks. SSc-T-cells were then seeded onto a second tissue insert and HSEs were layered onto them. 3D skin-like tissues (Fig. 1) were constructed with varying combinations of SSc patient-derived cells that included: (1) fibroblasts; (2) keratinocytes with optimal proliferative potential, (3) CD4+ T cells and (4) macrophages. This created a 3D tissue that combined all four cell types from the same SSc patient to create a fully autologous, patient-specific 3D skin-like model of SSc.
Results: Morphologic analysis of the 3D tissue model showed that T-cells migrated into the tissue and remained viable as indicated by elevated levels of IL-6 only when T cells were present in the tissues (Fig. 1, D). CFE assays found that two SSc patient-derived keratinocyte strains (SF-15.2 and SF14.2) showed high CFEs of 11% and 18% that were sufficient for 3D tissue fabrication. When SSc patient-matched keratinocytes and fibroblasts were used to fabricate HSEs, these autologous tissues developed a more well-differentiated epithelium than in tissues with cells that were not autologous (Fig 2). We established that 3D tissues can incorporate 4 SSc-derived cell types that can recapitulate the cellular heterogeneity seen in SSc in vivo.
Conclusion: We have determined that that (1) fully autologous 3D skin-like tissues can be constructed with 4 different SSc patient-derived cell types, (2) SSc-derived tissues containing these multiple cells from the same person with SSc (autologous tissues) result in improved tissue morphology and phenotype when compared to tissues constructed with cells from different SSc patient skins, (3) these multiple cell types contribute to intercellular cross-talk needed to optimize skin tissue architecture to study SSc. These autologous 3D tissues will streamline screening of promising candidate drugs designed to improve treatment of SSc so they can safely and efficiently enter human clinical trials.
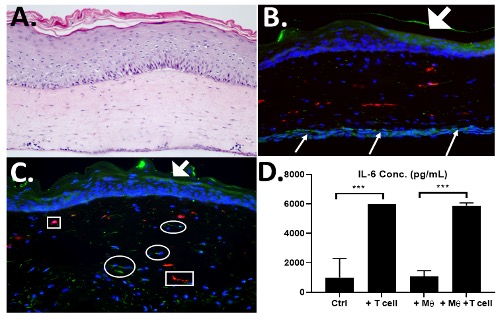 Figure 1. T cells in skin equivalents are functional- A) H&E image of 3D skin containing patient-derived fibroblasts, Macrophages and T cells. B) IHC staining for CD206-Macrophages (red) CD4-T cells (green) on bottom of tissue that migrated into dermis in 4 days (C). T cell function was shown by elevation of IL-6 secretion in T cell-containing tissues when compared to control or macrophage-only containing tissues (D).
Figure 1. T cells in skin equivalents are functional- A) H&E image of 3D skin containing patient-derived fibroblasts, Macrophages and T cells. B) IHC staining for CD206-Macrophages (red) CD4-T cells (green) on bottom of tissue that migrated into dermis in 4 days (C). T cell function was shown by elevation of IL-6 secretion in T cell-containing tissues when compared to control or macrophage-only containing tissues (D). 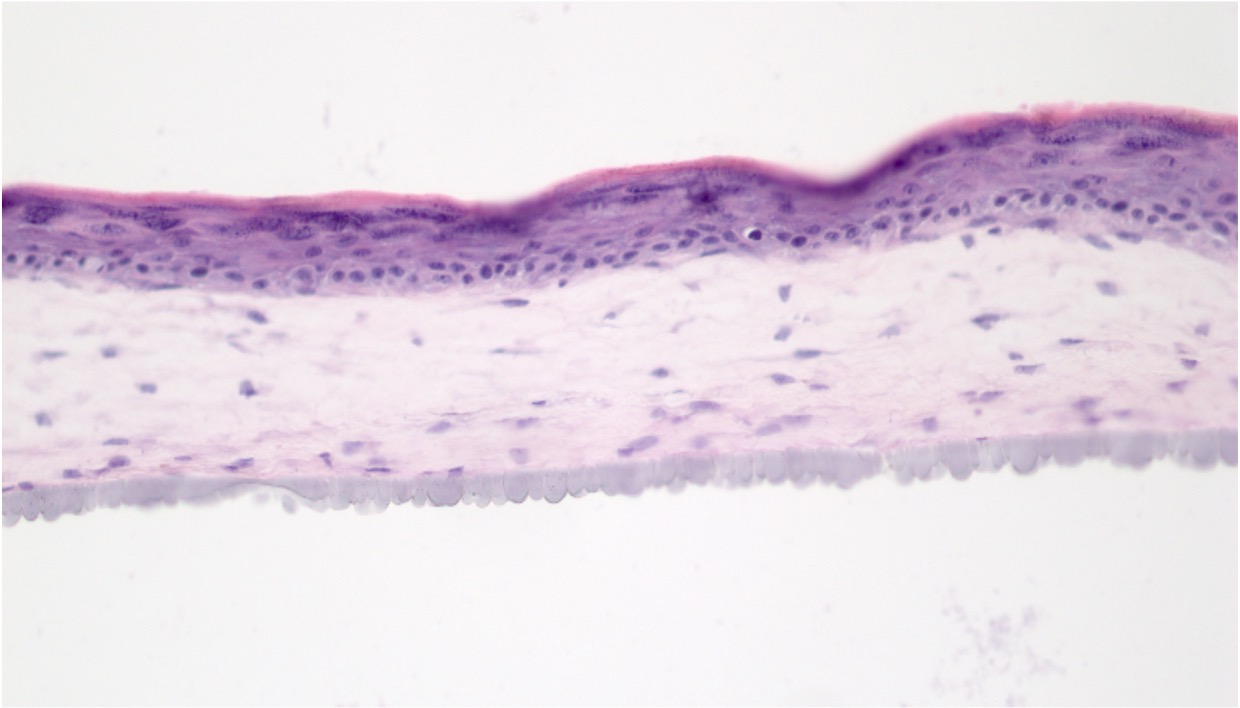 Figure 2. Fabrication of fully autologous human tissues with SSc cells- HSE skin-like tissues were constructed with patient-matched, SSc-derived keratinocytes (SK15.2) and fibroblasts (SF15.2). Tissues were grown for 2 weeks revealing well-differentiated epithelium and well-structured dermis.
Figure 2. Fabrication of fully autologous human tissues with SSc cells- HSE skin-like tissues were constructed with patient-matched, SSc-derived keratinocytes (SK15.2) and fibroblasts (SF15.2). Tissues were grown for 2 weeks revealing well-differentiated epithelium and well-structured dermis.Disclosures: S. Shenk, None; J. Garlick, None; L. Brown, None; J. Riesenberg, None; C. Evans, None; J. Jaffe Zweifach, None; A. Macklin, None; T. Abel, None; N. Kosarek, None; M. Huang, None; A. Smith, None; T. Wood, None; G. Torres, None; P. pioli, None; M. Whitfield, Corbus Pharmaceuticals, Celdara Medical LLC, Bristol-Myers Squibb(BMS).

