Back
Poster Session A
Vasculitis
Session: (0458–0497) Vasculitis – Non-ANCA-Associated and Related Disorders Poster I: Giant Cell Arteritis
0469: Factors Associated with Corticosteroid Dosing in the Management of Giant Cell Arteritis
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- LK
Loukas Kakoullis, MD, MPH
Mount Auburn Hospital
Watertown, MA, United States
Abstract Poster Presenter(s)
Loukas Kakoullis and Shiv Sehra, Mount Auburn Hospital, Cambridge, MA
Background/Purpose: Corticosteroids are the cornerstone of therapy in patients with giant cell arteritis (GCA). Tapering regiments vary considerably in both dose and duration, while relapses of the disease are common during the tapering of corticosteroids. We sought to evaluate parameters affecting the tapering corticosteroid dose in patients with GCA and the risk of recurrence during the corticosteroid treatment.
Methods: This study was a retrospective cohort of patients with GCA followed at Mount Auburn Hospital, Cambridge, MA, between 2017-2022. Inclusion criteria were the availability of data since the initial evaluation for GCA and through at least 3 months of follow up. Data were extracted from chart reviews and included patient demographics, clinical and laboratory parameters, treatment onset and duration, and episodes of recurrence. Statistical analysis was conducted using IBM SPSS for Windows, Version 27.
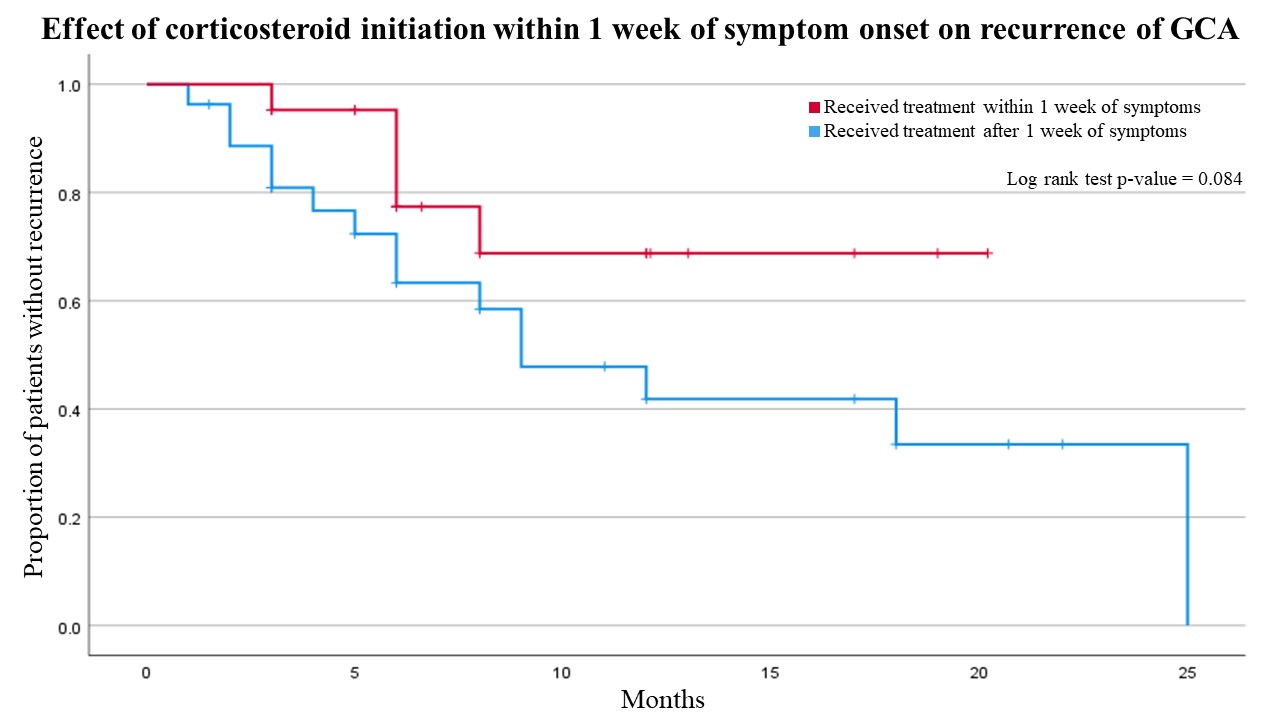
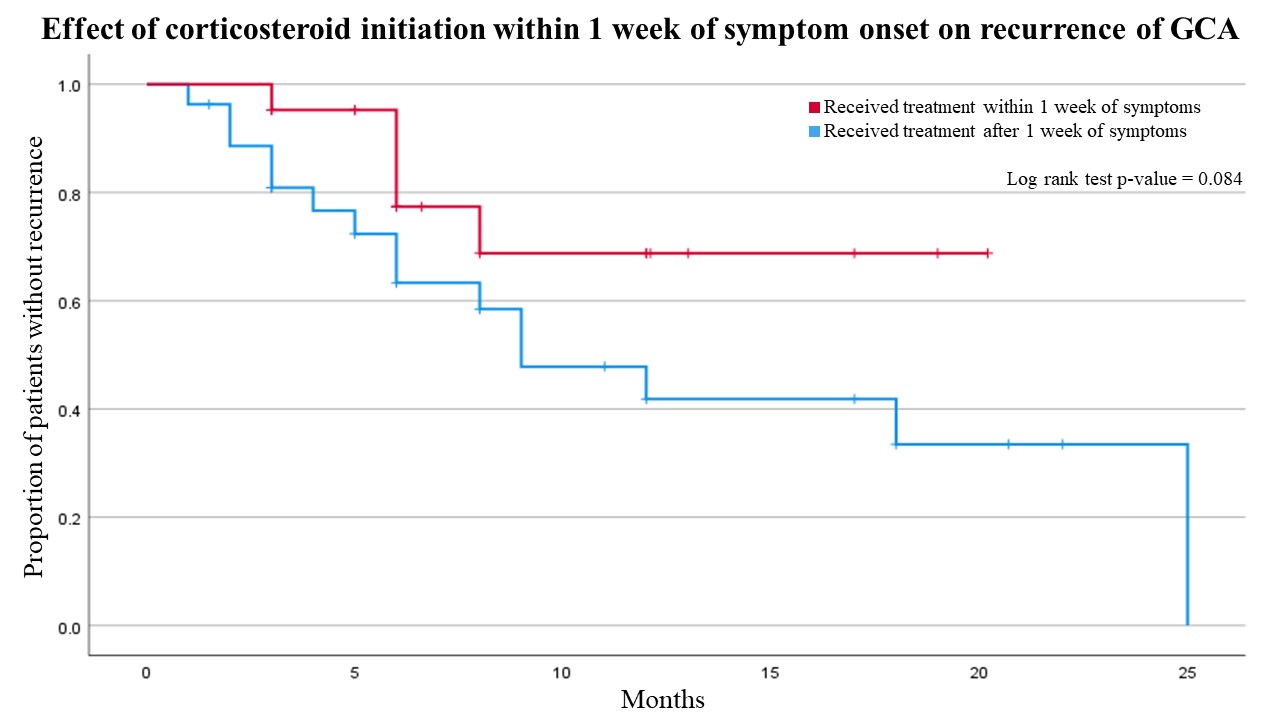
Results: Of the 215 records screened based on ICD 10 codes, 50 patients (mean age 75.44, 70% female) were noted to have a true diagnosis of GCA and fulfilled inclusion criteria. Median time between onset of symptoms and steroid administration was 8 days, while the mean dose of prednisone at months 1, 3 and 6 was 39.29 mg, 20.07 mg, and 10.02 mg, respectively. Recurrence of the disease during the first steroid taper was noted in 22 (44%) patients, at a median time of 6 months. Analysis demonstrated that the presence of recurrence during the first steroid taper was negatively correlated with the initiation of treatment within one week of symptom onset (r = -0.353, p = 0.014). In addition, patients who received steroids within one week of symptom onset had significantly reduced odds ratio (OR) of having a recurrence during the first prednisone taper (OR = 0.216; 95% CI = 0.061-0.764; p = 0.017), while the effect was maintained even after adjusting for patient demographic parameters, presence of specific symptoms or baseline markers of inflammation (OR = 0.096; 95% CI = 0.014-0.652; p = 0.017). Kaplan-Meier analysis (Figure 1) showed that early initiation of treatment was associated with longer recurrence-free survival, but this difference did not achieve statistical significance (15.8 vs 13.3 months; p-value = 0.084).Patients with a positive biopsy were found to receive significantly higher doses of prednisone at the 1-month timepoint compared to patients without (mean dose 45.71 vs 34.46, p = 0.00049); however, this difference did not persist at the subsequent time points. Furthermore, patients with a negative biopsy were significantly more likely to be receive prednisone at 40 mg or less at the 1-month timepoint (OR = 11.11; 95% CI = 2.54 - 48.66, p = 0.001), an effect maintained even after adjusting for confounding factors (OR = 8.98; 95% CI = 1.32 – 61.06, p = 0.025), while receiving the reduced dose had no correlation with the development of recurrence.
Conclusion: While early initiation of corticosteroids is critical in order to limit complications, this study demonstrates that it is also associated with reduced odds of recurrence during the first taper of corticosteroids.
Disclosures: L. Kakoullis, None; S. Sehra, None.
Background/Purpose: Corticosteroids are the cornerstone of therapy in patients with giant cell arteritis (GCA). Tapering regiments vary considerably in both dose and duration, while relapses of the disease are common during the tapering of corticosteroids. We sought to evaluate parameters affecting the tapering corticosteroid dose in patients with GCA and the risk of recurrence during the corticosteroid treatment.
Methods: This study was a retrospective cohort of patients with GCA followed at Mount Auburn Hospital, Cambridge, MA, between 2017-2022. Inclusion criteria were the availability of data since the initial evaluation for GCA and through at least 3 months of follow up. Data were extracted from chart reviews and included patient demographics, clinical and laboratory parameters, treatment onset and duration, and episodes of recurrence. Statistical analysis was conducted using IBM SPSS for Windows, Version 27.
Results: Of the 215 records screened based on ICD 10 codes, 50 patients (mean age 75.44, 70% female) were noted to have a true diagnosis of GCA and fulfilled inclusion criteria. Median time between onset of symptoms and steroid administration was 8 days, while the mean dose of prednisone at months 1, 3 and 6 was 39.29 mg, 20.07 mg, and 10.02 mg, respectively. Recurrence of the disease during the first steroid taper was noted in 22 (44%) patients, at a median time of 6 months. Analysis demonstrated that the presence of recurrence during the first steroid taper was negatively correlated with the initiation of treatment within one week of symptom onset (r = -0.353, p = 0.014). In addition, patients who received steroids within one week of symptom onset had significantly reduced odds ratio (OR) of having a recurrence during the first prednisone taper (OR = 0.216; 95% CI = 0.061-0.764; p = 0.017), while the effect was maintained even after adjusting for patient demographic parameters, presence of specific symptoms or baseline markers of inflammation (OR = 0.096; 95% CI = 0.014-0.652; p = 0.017). Kaplan-Meier analysis (Figure 1) showed that early initiation of treatment was associated with longer recurrence-free survival, but this difference did not achieve statistical significance (15.8 vs 13.3 months; p-value = 0.084).Patients with a positive biopsy were found to receive significantly higher doses of prednisone at the 1-month timepoint compared to patients without (mean dose 45.71 vs 34.46, p = 0.00049); however, this difference did not persist at the subsequent time points. Furthermore, patients with a negative biopsy were significantly more likely to be receive prednisone at 40 mg or less at the 1-month timepoint (OR = 11.11; 95% CI = 2.54 - 48.66, p = 0.001), an effect maintained even after adjusting for confounding factors (OR = 8.98; 95% CI = 1.32 – 61.06, p = 0.025), while receiving the reduced dose had no correlation with the development of recurrence.
Conclusion: While early initiation of corticosteroids is critical in order to limit complications, this study demonstrates that it is also associated with reduced odds of recurrence during the first taper of corticosteroids.
Disclosures: L. Kakoullis, None; S. Sehra, None.

