Back
Poster Session A
Patient engagement/self-management
Session: (PP01–PP22) Patient Perspectives Poster
PP20: 'It Is Due to Stress' – But Which Type of Stress? Cumulative childhood stress is a risk factor for autoimmune disease
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- MA
Melissa Allman, PhD
Michigan State University
Meridian Charter Township, MI, United StatesDisclosure: Disclosure(s): No financial relationships to disclose
Patient Poster Presenter(s)
Melissa Allman, Michigan State University, Meridian Charter Township, MI
Background/Purpose: Trauma can have profound detrimental influences on our health and well-being. I am tangibly familiar with how trauma can impact the individual due to my professional career as a (former) academic psychologist and neuroscientist, and my own story as a patient with rare autoimmune diseases (Relapsing Polychondritis, scleroderma, Sjogren's). There is an empirical literature from bench to bedside revealing childhood trauma and/or chronic stress (e.g., PTSD) increases the likelihood of autoimmune disease later in life. Yet this does not appear to have translated into clinical practice in rheumatology. The average time of diagnosis from symptom onset for autoimmune diseases is 4.5 years and during this time patients will have transferred across four doctors [1], likely because they feel dismissed. I've experienced this firsthand, having been told my symptoms were likely due to a broad spectrum of cockamamie diagnoses (ADHD, sports injury), until finally being diagnosed with rare autoimmune disease. I urge your use of patient trauma history questionnaires (e.g., Aversive Childhood Experiences) as this may overcome critical barriers that currently impede diagnosis and successful intervention strategies.
Intervention: The Aversive Childhood Experiences questionnaire [see CDC.gov] measures childhood chronic stress. With every score increase on the ACE questionnaire, risk for adult hospitalizations for autoimmune disease increases 20% [2, 3]. Despite the known mechanisms between inflammation and the stress response, I was never asked about chronic stress/trauma despite my PTSD dx; I have an ACE score of 6, which was dismissed by my rheumatologist. My autoimmune disease process took hold about 5 years ago when I began dealing with my childhood trauma. I am like the 80% of autoimmune patients whose onset of illness was precipitated by high emotional stress [4]. With the exception of Sjogren's, I was told it's due to stress (I was recommended tai chi over immunosuppressants by one rheumatologist).
Maintenance: The most effective physician to advance my healthcare has taken seriously my own trauma and autoimmune disease connection. For example, believing that the deterioration of my hip cartilage (bought on by a flare caused by emotional stress from my PTSD) and then evidenced on MRI was autoimmune in nature, and not because I must have had a sports-type injury and forgotten (as I was told by another physician). This led to my referral and diagnosis of RP.
Quality of Life: The fact childhood trauma and chronic stress may be an indicator for autoimmune disease is neglected when interacting with rheumatologists, and yet they are relatively quick to label our symptoms as due to acute stress, or other psychological aspects (e.g., health anxiety)-- particularly when they can't explain them or we return normal diagnostic test results (this can be harmful to both our body and mind, and led to a delay in my diagnosis and treatment). 'It is due to stress' – but which type of stress? Please consider any developmental trauma history in your patients as it is an indicator for an increased risk of underlying autoimmune disease.
References:
1. [1] AARDA
2. [2] Psychosom Med, 2009, 17: 243-50.
3. [3] PNAS, 2017, 104: 1319-24.
4. [4] Autoimm. Rev, 2008, 7: 209-13.
 Used with permission
Used with permission
 Used with permission
Used with permission
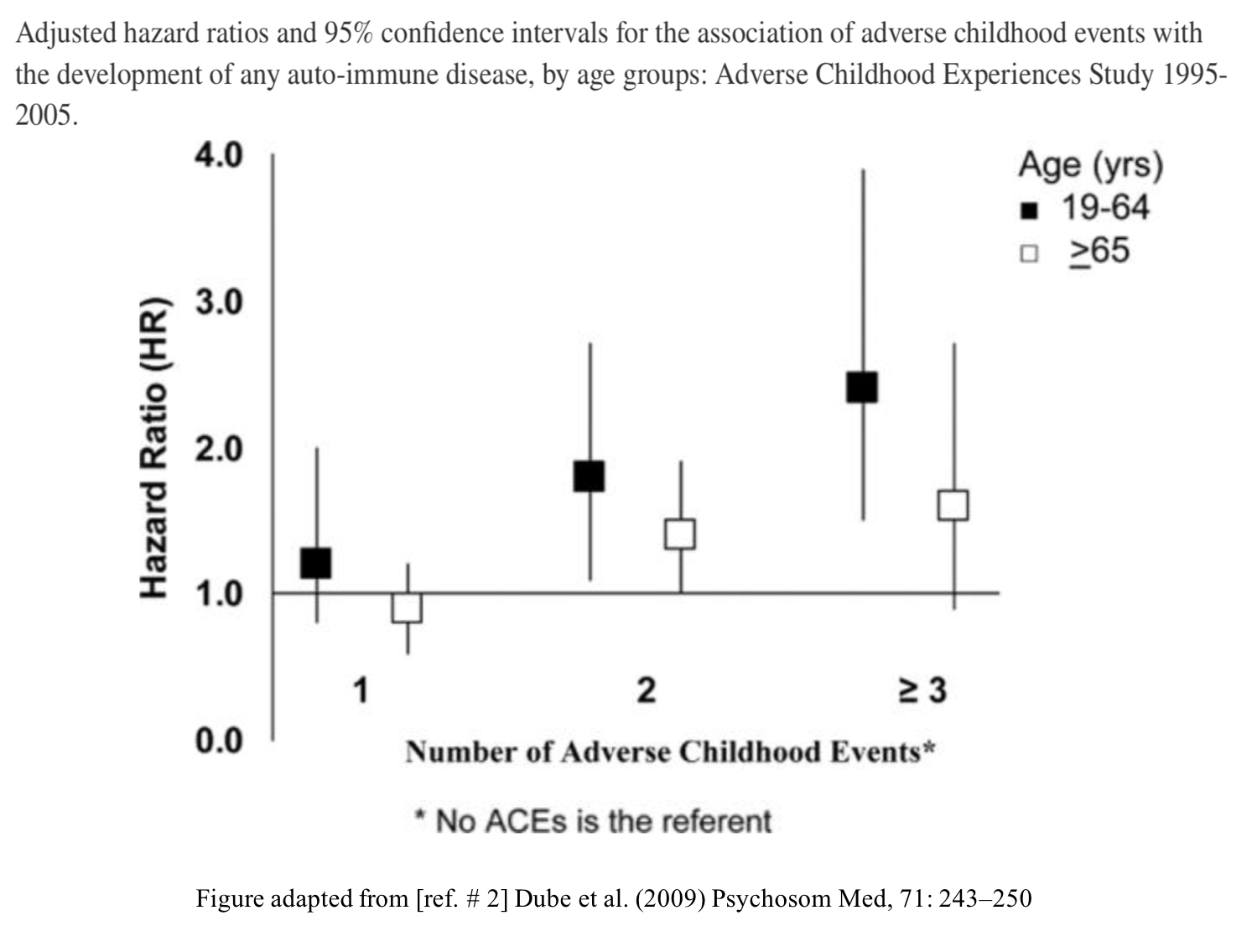 Figure is Open access
Figure is Open access
Disclosures: M. Allman, None.
Background/Purpose: Trauma can have profound detrimental influences on our health and well-being. I am tangibly familiar with how trauma can impact the individual due to my professional career as a (former) academic psychologist and neuroscientist, and my own story as a patient with rare autoimmune diseases (Relapsing Polychondritis, scleroderma, Sjogren's). There is an empirical literature from bench to bedside revealing childhood trauma and/or chronic stress (e.g., PTSD) increases the likelihood of autoimmune disease later in life. Yet this does not appear to have translated into clinical practice in rheumatology. The average time of diagnosis from symptom onset for autoimmune diseases is 4.5 years and during this time patients will have transferred across four doctors [1], likely because they feel dismissed. I've experienced this firsthand, having been told my symptoms were likely due to a broad spectrum of cockamamie diagnoses (ADHD, sports injury), until finally being diagnosed with rare autoimmune disease. I urge your use of patient trauma history questionnaires (e.g., Aversive Childhood Experiences) as this may overcome critical barriers that currently impede diagnosis and successful intervention strategies.
Intervention: The Aversive Childhood Experiences questionnaire [see CDC.gov] measures childhood chronic stress. With every score increase on the ACE questionnaire, risk for adult hospitalizations for autoimmune disease increases 20% [2, 3]. Despite the known mechanisms between inflammation and the stress response, I was never asked about chronic stress/trauma despite my PTSD dx; I have an ACE score of 6, which was dismissed by my rheumatologist. My autoimmune disease process took hold about 5 years ago when I began dealing with my childhood trauma. I am like the 80% of autoimmune patients whose onset of illness was precipitated by high emotional stress [4]. With the exception of Sjogren's, I was told it's due to stress (I was recommended tai chi over immunosuppressants by one rheumatologist).
Maintenance: The most effective physician to advance my healthcare has taken seriously my own trauma and autoimmune disease connection. For example, believing that the deterioration of my hip cartilage (bought on by a flare caused by emotional stress from my PTSD) and then evidenced on MRI was autoimmune in nature, and not because I must have had a sports-type injury and forgotten (as I was told by another physician). This led to my referral and diagnosis of RP.
Quality of Life: The fact childhood trauma and chronic stress may be an indicator for autoimmune disease is neglected when interacting with rheumatologists, and yet they are relatively quick to label our symptoms as due to acute stress, or other psychological aspects (e.g., health anxiety)-- particularly when they can't explain them or we return normal diagnostic test results (this can be harmful to both our body and mind, and led to a delay in my diagnosis and treatment). 'It is due to stress' – but which type of stress? Please consider any developmental trauma history in your patients as it is an indicator for an increased risk of underlying autoimmune disease.
References:
1. [1] AARDA
2. [2] Psychosom Med, 2009, 17: 243-50.
3. [3] PNAS, 2017, 104: 1319-24.
4. [4] Autoimm. Rev, 2008, 7: 209-13.
 Used with permission
Used with permission Used with permission
Used with permission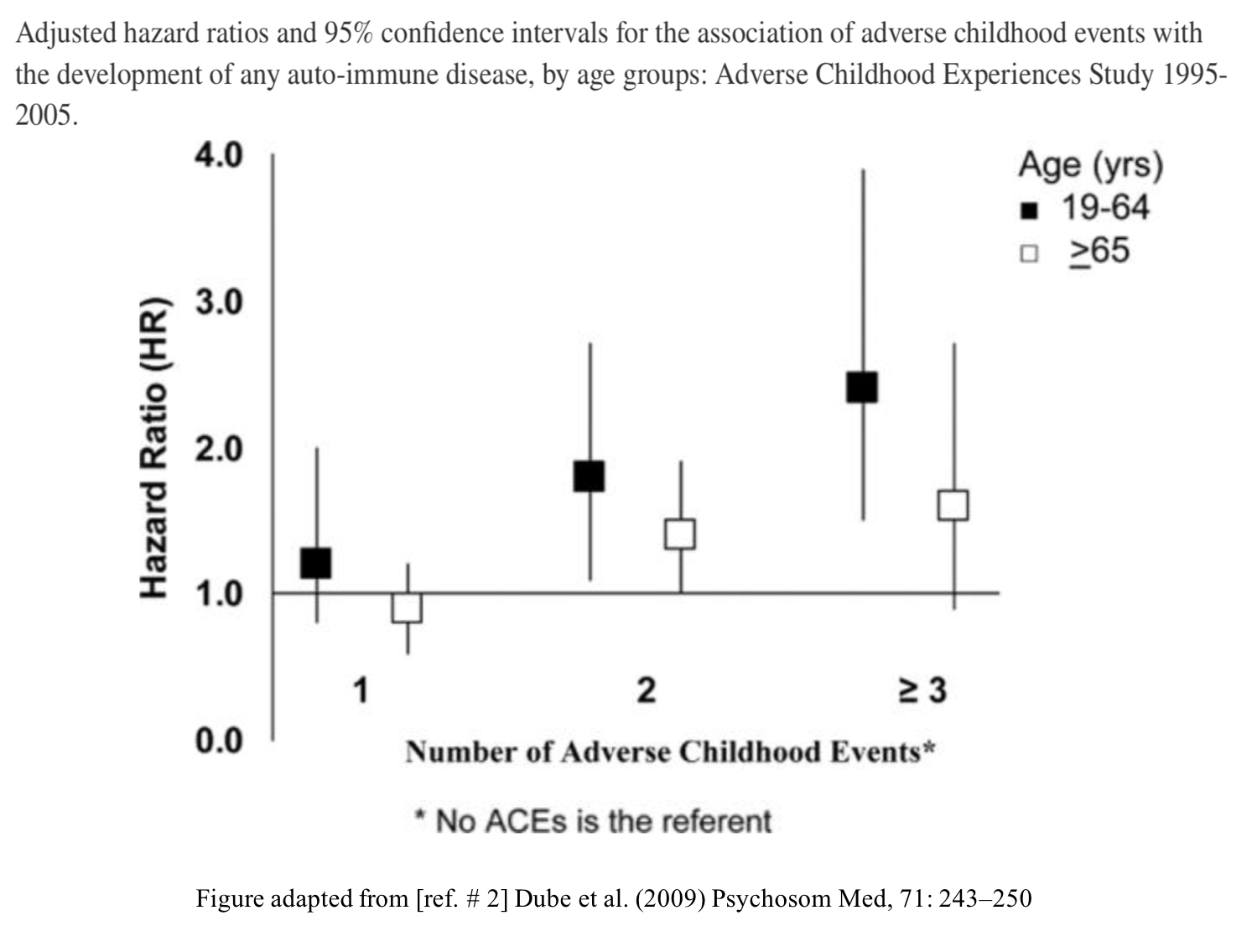 Figure is Open access
Figure is Open access Disclosures: M. Allman, None.

